Translate this page into:
Keratinising Squamous cell carcinoma-A rarity
Address for correspondence: Dr. Akheel MohammadBlock 5, 4H, VGN Laparasiene, Nolambur, Mogappair West, Chennai - 600 037, Tamil Nadu, India. drakheelomfs@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Keratocystic odontogenic tumor (KCOT) is still a dilemma in the field of medical science because of its biological behavior and transformation of this benign odontogenic tumor to a carcinomatous type, which is called as odontogenic carcinoma. We are presenting here a case of squamous cell carcinoma occurring in recurrent KCOT of temporal region. The rarity of this article is the location of the lesion which is rarest at temporal region. Malignant transformation of these KCOT’s has been reported only in 15 cases in literature, the majority occurring in jaws but no case reported for lesion of temporal region. The pathogenesis of the tumor, the biologic progression, overall clinical, and histopathological features of this rare malignancy, and its management is reported and discussed.
Keywords
Keratinizing squamous cell carcinoma
odontogenic carcinoma
temporal region
Introduction
Keratocystic odontogenic tumor (KCOT) is still a unique pathological entity due to its anatomical and biological behavior since it description by Phillipsen in 1956.1 Squamous cell carcinoma (SCCA) arising from the wall of KCOT is rare which occurs mainly in jaw bones called as keratinizing squamous cell carcinoma (odontogenic carcinoma) as first described by Loos in 1913.2,3 Management of these lesion at rare anatomic location possess a challenge for the surgeon.
Case Report
A 66-year-old female patient reported to our Department of Oral and Maxillofacial Surgery complaining about a slow growing painless swelling in the right side temporal region from past 1 month. Her medical history was noncontributory. According to her previous reports, she had a history of enucleation of KCOT in the right side posterior region with the extraction of 46, 47, and 48, 5 years back. There was a recurrence of multilocular KCOT again 2 years back for which she underwent hemimandibulectomy with disarticulation of the condyle on the right side till 32. She had no history of tobacco or illicit substance use. Maxilla was edentulous and atrophic. On examination, there was a painless swelling measuring about 5 cm × 4 cm, round with well-defined borders in the right temporal region which was fixed to the temporalis muscle. The swelling was nontender, nonfluctuant, and nonpulsatile no palpable local, or regional lymphadenopathy was seen.
Radiological examination included computed tomography brain. There was a hypodense swelling involving soft tissue on the right side temporal region. No involvement of the bone was seen Figure 1. On aspiration biopsy, we got a dark yellow straw colored fluid. After a complete clinical, radiological and biopsy examination, provisional diagnosis of recurrent KCOT was made. Wide local surgical excision of the tumor in general anesthesia was performed Figures 23. The completely resected specimen was sent for histopathological examination, which was suggestive of well-differentiated keratinizing SCCA of the temporal region. In some areas, the lining showed increasing dysplastic change, transforming ultimately into invasive keratinizing SCCA.
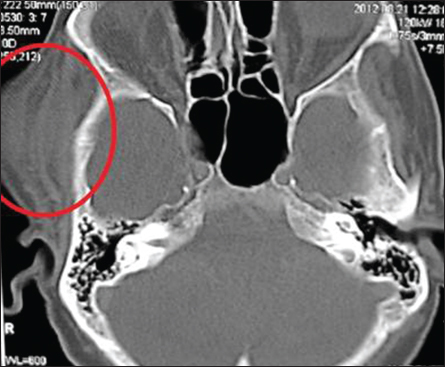
- Computed tomography brain showing the lesion on right side involving the muscle
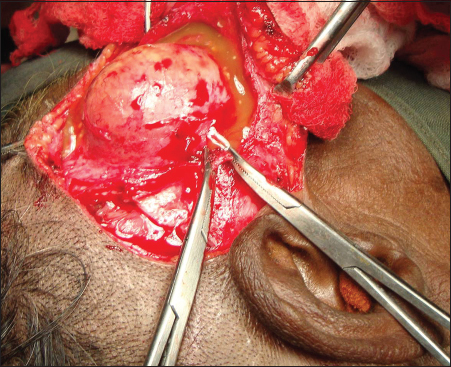
- Exposure of the lesion within temporalis muscle with fluid coming out due to accidental puncture of the lesion
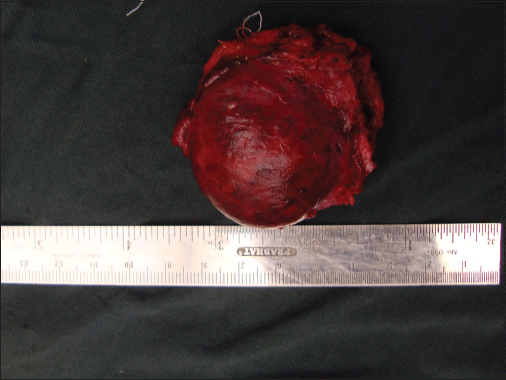
- Wide local excision of the lesion along with temporalis muscle with 1.0 cm clear margins
Postoperative ultrasonography of the abdomen was done which was negative to rule out any primary site of tumor. There was transient facial nerve palsy which has recovered in 3 months. Otherwise, postoperative recovery was uneventful. There was the presence of temporal hollowing but considering the age of the patient it was of minimal facial esthetic concern. The patient was sent for prophylactic radiotherapy. In follow-up of 6 consecutive months, the patient is doing well, and there was no recurrence of lesion or lymphadenopathy seen till present.
Discussion
Van der Wal et al.4 reported that the presence of keratinization in the cystic lining is a risk factor for malignant changes and Gardner et al. indicated that odontogenic cysts with keratinization are often prone for malignant changes than nonkeratinizing cysts. Eversole et al.5 in 1975 reported out of 32 cases of central carcinoma, 75% were often associated with a cyst.
In 1975, Gardner6 proposed certain criteria for the diagnosis of SCCA arising in an odontogenic cyst. They are microscopic transition area from benign cystic epithelial lining to invasive SCCA; there must be no carcinomatous changes in the overlying epithelium and no source of carcinoma in the adjacent structures. A fourth criterion added by Waldron and Mustoe7 was the possibility that the lesion represents a metastasis from a distant tumor must be ruled out by physical and radiological examination and the subsequent clinical course. Several features of this case support Waldron’s criteria. There was no evidence of any primary tumor elsewhere in the body. There were no signs of paresthesia probably because the malignant changes were confined within the cystic lining. Discovery of SCCA arising in this KCOT was unexpected.
Magnetic resonance imaging is an investigation of choice for soft tissue swellings, but since our patient was having a financial crisis, it could not be done. Bone scintigraphy can be done to rule out any metastatic disease. Treatment of choice for these lesions is surgery with wide margins with 1–1.5 cm clearance of unaffected tissue. Intraoperative Frozen section analysis can be done to achieve tumor-free surgical margin if the diagnosis of malignancy is made before the treatment procedure. Addressing of the nodes has to be done if there is local or regional lymph node metastasis with the appropriate type of neck dissection. In this case, since the patient did not have any local or cervical lymphadenopathy; hence, neck dissection was not done. Radiation therapy can be given as an adjuvant as in this case. Bone scintigraphy can be done to rule out any metastatic bone diseases. In general, the prognosis is poor, and metastasis to cervical lymph nodes is observed in up to 50% of cases in a well-established SCCA. Two years survival rate of patients has been reported in 53%.8
Conclusion
This article analyzes the origin, clinical and histopathological features, and surgical outcome of a malignant transformation of a KCOT of the temporal region into SCCA. It illustrates the importance of adequate microscopic investigation of all recurrent excised cysts and their appropriate management to improve the prognosis of a patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Characterization and management of the keratocystic odontogenic tumor in relation to its histopathological and biological features. Oral Oncol. 2010;46:219-25.
- [Google Scholar]
- Central epidermoid carcinoma of the jaws. Dtsch Montatschr Zahnheilkd. 1913;31:308.
- [Google Scholar]
- Primary intraosseous odontogenic carcinoma with osteoid/dentinoid formation. J Oral Pathol Med. 2004;33:121-4.
- [Google Scholar]
- Squamous cell carcinoma arising in a residual cyst. A case reportInt J Oral Maxillofac Surg. 1993;22:350-2.
- [Google Scholar]
- Aggressive growth and neoplastic potential of odontogenic cysts: With special reference to central epidermoid and mucoepidermoid carcinomas. Cancer. 1975;35:270-82.
- [Google Scholar]
- The odontogenic cyst as a potential carcinoma: A clinicopathologic appraisal. J Am Dent Assoc. 1969;78:746-55.
- [Google Scholar]
- Primary intraosseous carcinoma of the mandible with probable origin in an odontogenic cyst. Oral Surg Oral Med Oral Pathol. 1989;67:716-24.
- [Google Scholar]
- Primary intraosseous carcinomas of the jaws arising within an odontogenic cyst, ameloblastoma, and de novo: Report of new cases with reconstruction considerations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e29-33.
- [Google Scholar]







