Translate this page into:
Metaplastic squamous cell carcinoma of the breast – A rare case report
Corresponding author: Dr. Aditya Adhav, Department of Surgical Oncology, HCG Manavata Cancer Centre, Nashik, Maharashtra, India. academics@manavatacancercentre.com
-
Received: ,
Accepted: ,
How to cite this article: Hussain M, Adhav A, Roy S, Ramesh YV, Nagarkar R. Metaplastic squamous cell carcinoma of the breast – A rare case report. Asian J Oncol, 2023;9:7.
Abstract
Metaplastic carcinomas of the breast are unusual conditions and account for 0.25% to 1% of annual breast malignancies. Among these, primary metaplastic squamous cell carcinoma (SCC) of the breast is an extremely rare entity occurring in less than 0.1% of all breast carcinomas. Management protocol and survival outcome for metaplastic breast carcinoma is relatively unknown because of the rarity of the disease, but studies suggest that removal of the tumor and adjuvant radiotherapy has the greatest impact. In this paper, we report the occurrence of this rare lesion in a 71-year-old lady who was treated and is recovering uneventfully. Early diagnosis and radical upfront surgery may warrant a good prognosis, as demonstrated in this case report.
Keywords
Breast cancer
Metaplastic squamous cell carcinoma
Diagnosis
Rare case report
INTRODUCTION
Metaplastic carcinomas of the breast are unusual conditions and account for 0.25% to 1% of annual breast malignancies. It consists of a wide variety of neoplasms with predominantly nonglandular differentiation of spindle cells, squamous cells, and/or mesenchymal cells. Among these, primary metaplastic squamous cell carcinoma (SCC) of the breast is an extremely rare entity occurring in less than 0.1% of all breast carcinomas.[1] These carcinomas usually present as well-defined tumors and on radiological evaluation, such as mammography, sometimes may exhibit morphological similarities with benign lesions as well as some variants of invasive ductal carcinoma. However, behaviorally, they tend to be more aggressive tumors having a worse prognosis than other varieties of triple negative invasive ductal carcinomas.[2,3] To confirm a diagnosis of primary SCC of the breast, three criteria must be fulfilled: absence of an associated SCC in a second site, absence of skin involvement, and a clear predominance (90%) of areas with SCC at histologic examination.[4] Management protocol and survival outcome for metaplastic breast carcinoma is relatively unknown because of its relatively rare occurrence, but studies suggest that removal of the tumor and adjuvant radiotherapy has the greatest curative impact. In this paper, we present a case of a 71-year-old lady afflicted with this rare type of lesion.
CASE REPORT
A 71-year-old post-menopausal, otherwise healthy lady presented with a palpable mass in her left breast since a period of 4 months. She denied any family history of breast, cervical, or ovarian cancer. She had no history of previous skin cancer or any skin, oral, pharyngeal, or anal lesions. On examination, a 4 × 4 cm hard, immobile, and nontender mass was palpable in the upper outer quadrant of her left breast. There was no nipple or areolar retraction, no nipple discharge, and no involvement of the outer skin. Left axillary lymph nodes were not palpable. A diagnostic bilateral mammography [Figure 1] was performed, which revealed a suspicious well-defined heterogenous lesion with solid and cystic components measuring 43 × 39 mm in the upper and outer quadrant of left breast. Another incidental finding was a small well-defined hypoechoic cystic lesion measuring 9 × 4 mm at 12 o’ clock position in the right breast, which was likely benign. The patient then underwent an ultrasound-guided core-cut biopsy from the left breast mass. Histopathological examination revealed invasive ductal carcinoma with high nuclear grade and a focus on squamous differentiation. Histologic examination of the entire lesion was suggested to rule out metaplastic carcinoma. Immunohistochemistry revealed that the tumor was negative for Estrogen Receptor (ER), Progesterone Receptor (PR), and her two receptors (TNBC). A chest X-ray and an ultrasonography of the abdomen and pelvis were done to grossly rule out a primary disease at these sites. In view of the histopathological report, the patient was promptly taken up for surgery and uneventfully underwent left modified radical mastectomy (MRM). In the post-operative surgical pathology report on gross examination, the tumor measured 3.5 × 3 × 3 cm, 1 cm away from the overlying skin and base. All margins were free of tumor. Nine axillary lymph nodes were dissected, largest measuring 1.5 × 1.3 × 1 cm, all free of tumor. On histopathological examination, multiple sections predominantly showed tumor cells showing squamous cell differentiation with extensive intratumoral keratinization [Figure 2]. Cells showed distinct cytoplasmic border with central nucleus and moderate amount of cytoplasm. All features favored metaplastic SCFC. Modified R.B Score was 8, Ductal carcinoma in situ (DCIS) was absent, lympho-vascular emboli and perineural invasion were negative, all margins including overlying skin was free of tumor. Tumour, Node, Metastasis (TNM) staging of the tumor was pT2pN0Mx. One week post-operatively, the patient seemed to be doing well and recovering uneventfully [Figure 3]. Further treatment options were discussed with the medical and radiation oncologists and she was subjected to adjuvant therapy.
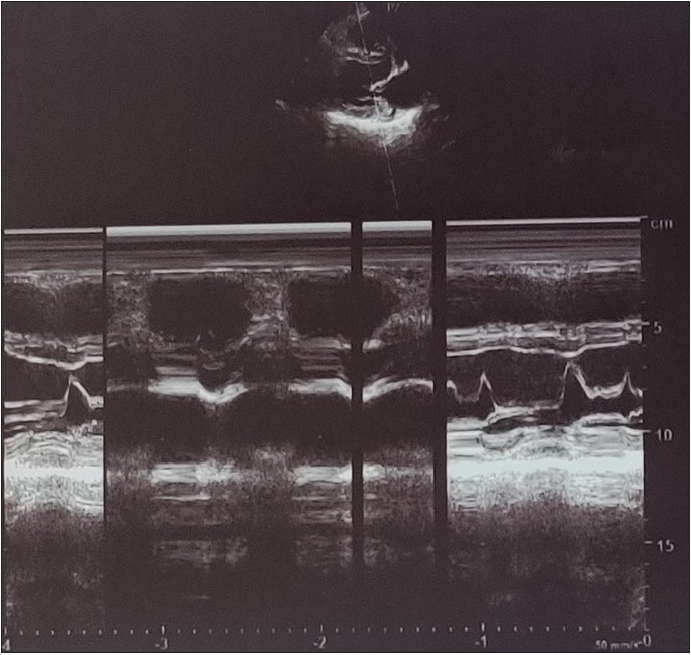
- Diagnostic bilateral mammography.
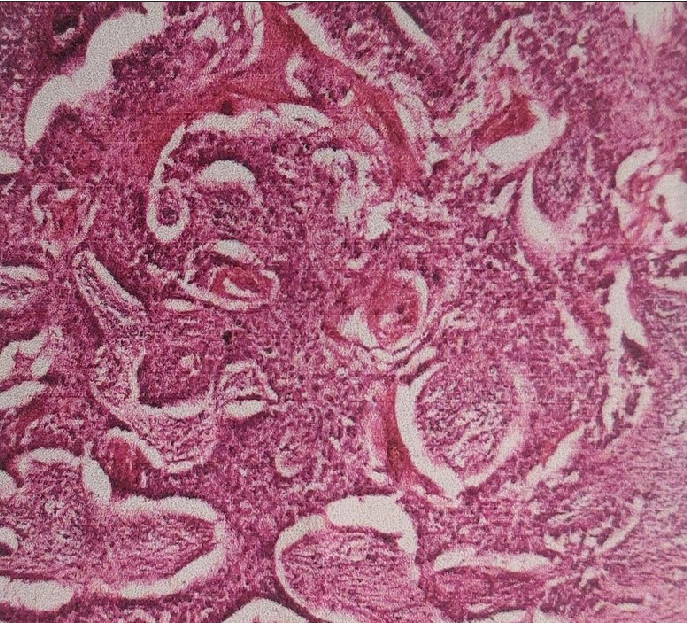
- Histopathological examination demonstrating tumor cells exhibiting squamous cell differentiation with extensive intra tumoral keratinization.

- Post-operative scar after MRM.
DISCUSSION
Metaplastic breast carcinoma is a variant of adenocarcinoma characterized histologically by a combination of mesenchymal and epithelial cells. It accounts for less than 1% of all breast malignancies and a relatively rare condition as compared to invasive ductal carcinoma.[5,6] Many theories are put forward to explain the histogenesis of SCC of the breast; however, it remains unclear. One school of thought suggests that its origin is by squamous metaplasia, which is found in the epithelium of cysts, fibroadenomas, phyllodes tumors or papillomas and chronic abscess, whereas others believe that it originates from myoepithelial cells.[7] We assume that our patient had cystic lesions in her breasts for a long period of time which went unnoticed and because of the chronic irritation, the cells underwent metaplasia and developed metaplastic SCC in her left breast. The incidental finding of a separate cystic lesion in her right breast also supports our assumption of prolonged undiagnosed cystic lesions in her breasts, the epithelium of which underwent squamous metaplasia in her left breast but remained unchanged in her right breast mostly due to its small size. The mean age at which metaplastic SCC of the breast is presented is 54 years.[8] We assumed that in our patient, it went unnoticed and remained asymptomatic for a long time and hence was presented late at 71 years. The 5-year disease-free survival rate is estimated to be around 40% with an overall survival rate in the range of 49% to 68%.[6] Breast metaplastic SCC usually tends to be a relatively large, rapidly growing mass that becomes palpable within 2 to 3 weeks attaining a size of 2–5 cm to 4 cm.[4,9,10]
There is also no pathognomonic radiographic imaging found for metaplastic SCC of the breast. A metaplastic carcinoma mass typically presents as either a well-circumscribed lesion or an indistinct, very dense mass with infrequent calcifications.[8] In our case, it was a well-defined heterogenous lesion demonstrating both solid and cystic components. More than 90% of metaplastic SCC of the breast is considered triple-negative (TNBC), which is generally expected as most SCC of the breast has the basal-like molecular subtype.[8] These carcinomas demonstrate a lower rate of axillary lymph node metastasis as compared to the invasive breast carcinoma of the same size, but late distant metastasis can be documented without lymph node involvement. 6 In our case too, axillary lymph nodes were dissected but all were free of tumor. Due to its rare occurrence, there is little data on the optimal treatment regimen for metaplastic squamous cell breast cancer and similar management protocols are followed to that of Invasive ductal carcinomas (IDCs).[11] On reviewing the available literature on surgical management in this rare group of patients, we found that similar to our surgical plan of MRM, the majority of patients were treated with similar type of surgery and breast conservation was seldom used. Important contributing factors on why mastectomy was the reported surgery of choice in this group of patients were the rapid progression of the cancer, and its poor response to neo-adjuvant and conventional chemotherapy.[11] This emphasizes the importance of early treatment in this subtype of patients as was given in our case.
CONCLUSION
In conclusion, the outcome of the patient afflicted with metaplastic SCC of the breast is influenced by the rarity, aggressiveness, and triple negativity of the tumor. Early diagnosis and radical upfront surgery usually warrant a good prognosis in these cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Metaplastic breast cancer: clinicopathological features and its prognosis. J Clin Pathol. 2012;65:441-6.
- [CrossRef] [PubMed] [Google Scholar]
- Metaplastic carcinoma of the breast with squamous differentiation: a case report from the University Teaching Hospital of Kigali (CHUK), Rwanda. Case Rep Pathol. 2020;2020:1-3.
- [Google Scholar]
- Squamous cell carcinoma of the breast. J Clin Oncol. 2005;23:7827-35.
- [CrossRef] [PubMed] [Google Scholar]
- Metaplastic breast cancer: histologic characteristics, prognostic factors and systemic treatment strategies. Exp Hematol Oncol. 2013;2:1-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Case reports on metaplastic squamous cell carcinoma of the breast and treatment dilemma. https://www.hindawi.com/journals/crionm/2019/4307281/ (accessed 2022-05-30).
- Konkankit VV, Reusser GE, Ding PD. A case report on a rare finding: metaplastic squamous cell carcinoma of the breast. 2016.
- Primary pure squamous cell carcinoma of the breast. Clin Breast Cancer. 2005;6:270-2.
- [CrossRef] [PubMed] [Google Scholar]
- Primary squamous cell carcinoma of breast with ipsilateral axillary lymph node metastasis: an unusual case. Int J Surg Case Rep. 2011;2:194-7.
- [CrossRef] [PubMed] [Google Scholar]
- Natural history of metaplastic squamous cell breast cancer: a case report and literature review on surgical management. Gland Surg. 2017;6:738.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







