Translate this page into:
Suprasellar dermoid cyst masquerading as tumor: A case report
Corresponding author: Dr. Mustafa Ismail, Department of Neurosurgery, Neurosurgery Teaching Hospital, Al Risafa, Baghdad, Iraq. mustafalorance2233@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Al-Zaidy MF, Mustafa I, Alasady AF, Al-Hilfi MS, Al-Sandooq MS, Fatimah A, et al. Suprasellar dermoid cyst masquerading as tumor: A case report. Asian J Oncol, doi: 10.25259/ASJO_5_2023
Abstract
Intracranial dermoid cysts (DCs) are well-defined, rare ectodermal inclusion cystic lesions. Symptomatic DCs usually present with symptoms due to local mass effect, seizures, or recurrent meningitis, depending on the specific location of the lesion. Suprasellar DCs have fairly classical features and locations, allowing radiological diagnosis in most patients; however, they can sometimes mimic some tumors in the region. Despite the progress made in imaging modalities, it can still be difficult to exclude the differential diagnosis of other tumors. In this report, we present an interesting case of an atypical DC that mimicked a tumor, specifically a craniopharyngioma or meningioma.
A 60-year-old female presented with headaches for four months and left visual field defects. A cranial computed tomography (CT) scan revealed an iso-to-hyperdense suprasellar lesion with intralesional calcification, which was extended to the left parasellar region. Brain magnetic resonance imaging (MRI) showed a suprasellar and more in the left sphenoid lesion that was hyperintense on T1-weighted imaging (T1WI) and hyper to mixed signal on T2-weighted imaging (T2WI), with gadolinium enhancement. Sphenoid wing meningioma and craniopharyngioma were mainly suspected as differential diagnoses. Intraoperatively, fluid was evacuated, and it was like machine oil. It was very comparable to the typical fluid of craniopharyngioma. Consequently, part of the lesion wall was dissected and portions of fatty and calcified content were removed. While removing the deepest part of the lesion, we encountered several hair follicles within the lesion. Immediately, the diagnosis shifted into a DC. Histopathology confirmed the diagnosis.
The DCs can be considered in the differential diagnosis of suprasellar tumors, as they can have similar clinical and radiological features to more commonly encountered tumors such as craniopharyngiomas and meningiomas, particularly when located in the suprasellar region and presenting with imaging characteristics that are non-cystic and not hypodense.
Keywords
Dermoid cyst
Suprasellar lesion
Radiology
Craniopharyngioma
Meningioma
INTRODUCTION
Intracranial dermoid cysts (DCs) are well-defined, rare ectodermal inclusion cystic lesions, representing about 0.04%–0.6% of all brain tumors.[1,2] The most commonly arise in the midline and are more in the posterior fossa than the supratentorial compartment; moreover, they are relatively rare in the suprasellar and parasellar regions.[1–3] DCs in the suprasellar area can be considered part of the differential diagnosis of suprasellar masses, which include pituitary adenoma, craniopharyngioma, meningioma, and epidermoid cysts; in some situations, DCs can mimic them.[4,5] Symptomatic DCs usually present with symptoms due to local mass effect, seizures, or recurrent meningitis, depending on the specific location of the lesion.[1] Radiologically, DCs typically appear as a hypodense lesion on the brain computed tomography (CT) scan, the cranial magnetic resonance imaging MRI characteristics hyperintense on T1-weighted imaging (T1W1), variable appearance on T2-weighted imaging (T2WI), and absent of contrast enhancement with gadolinium.[3] However, in extremely rare cases, DCs can present atypical imaging features with hyperdense on CT or hypointense on T1WI, precluding diagnosis due to resembling other lesions that arise in the suprasellar and parasellar space, leading to a challenging diagnosis.[1]
Herein, we describe an interesting case of DC mimicking a craniopharyngioma and meningioma with atypical radiological findings on CT and MRI that led to a diagnostic dilemma.
CASE REPORT
A 60-year-old female presented to the emergency department with headaches for four months. She was fully conscious; neurological examination showed left visual field defects with no other focal neurological deficits. A head CT scan revealed an iso-to-hyperdense suprasellar lesion (about 60 × 45 × 50 mm dimensions) with intralesional calcification, and it was extended to the left parasellar region [Figure 1a and b]. Subsequent brain MRI showed a suprasellar and also more in left sphenoid lesion that was hyperintense on T1WI and hyper to mixed signal on T2WI, with gadolinium enhancement [Figure 2a, 2b and 2c]. The cerebral catheter angiogram ruled out any vascular lesions. The presence of iso-to-hyperdensity mass in the area of the sphenoid ridge with calcification on CT scan and no peripheral edema raised the suspicion of meningioma (possible sphenoid wing meningioma). However, extreme sellar extension is a point against this suspicion. In contrast to craniopharyngioma as a possible diagnosis, in this case, the feature on MRI that includes hyperintense on T1WI and hyper to mixed signal on T2WI and contrast enhancement may be caused by craniopharyngioma. Nevertheless, the later extension to the sphenoid ridge and the absence of extension to the third ventricle are atypical of craniopharyngioma.
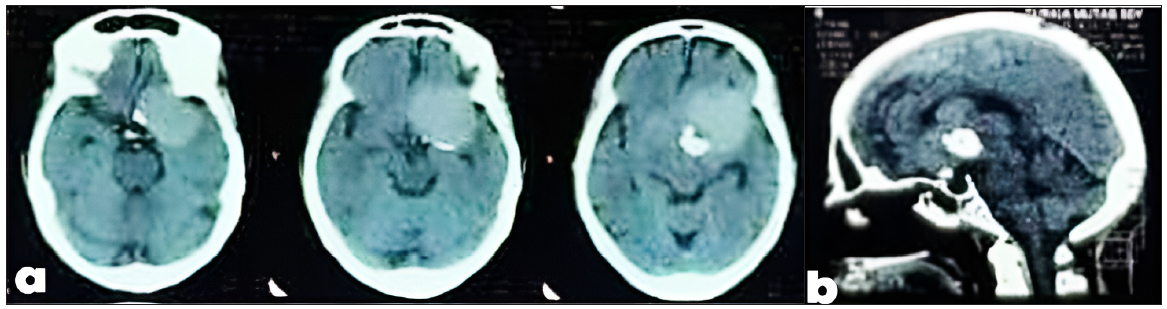
- (a) Non-contrast brain CT scan with axial view demonstrates a rounded iso-to-hyperdense suprasellar lesion with calcification and extension to the left, (b) Non-contrast brain CT scan with sagittal view demonstrates a rounded iso-to-hyperdense suprasellar lesion with calcification and extension to the left. CT: Computed tomography.
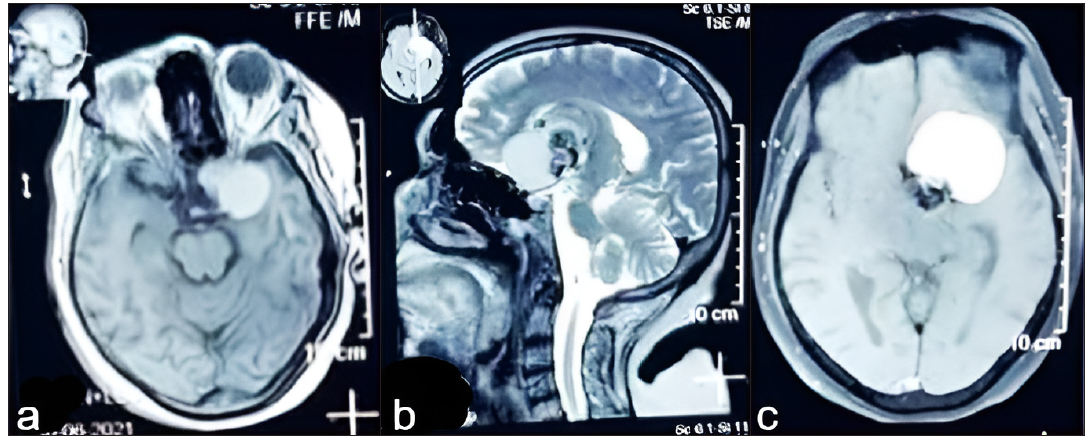
- (a) Brain MRI shows a suprasellar with extension to left sphenoid mass that was hyperintense on T1WI axial view, (b) Brain MRI shows a suprasellar with extension to left sphenoid mass that was hyper to mixed signal on T2WI sagittal view, (c) Brain MRI shows a suprasellar with extension to left sphenoid mass with gadolinium enhancement revealed on postcontrast T1WI axial view. MRI: magnetic resonance imaging, T1 weighted image (also referred to as T1WI or the “spin-lattice” relaxation time) is one of the basic pulse sequences in MRI and demonstrates differences in the T1 relaxation times of tissues.
Based on the above radiological discussion, we as a team decided to do the surgery via a pterional approach and have craniopharyngioma and sphenoid wing meningioma at the top of the differential diagnosis list; the craniotomy, osteoplastic bone flap, and durotomy were performed. Following the Sylvian fissure dissection, the initial exploration part of the lesion was explored, and the color of the evacuated fluid was like machine oil. Further, it was very comparable to the typical fluid of craniopharyngioma. Consequently, part of the lesion wall was dissected and portions of fatty and calcified content were removed. During the removal of the deepest lesion’s part, we encountered several hair follicles within the lesion. Immediately, the diagnosis shifted into a DC and all the other differential diagnoses were excluded [Figure 3]. Total resection of the cyst was not achievable because of the adherence of the calcified medial part to the surrounding neurovascular structure. The surgery was unremarkable and the postoperative course was uneventful. The postoperative CT scan confirmed the subtotal removal of the cyst with the remaining calcified medial sellar part [Figure 4a and b].
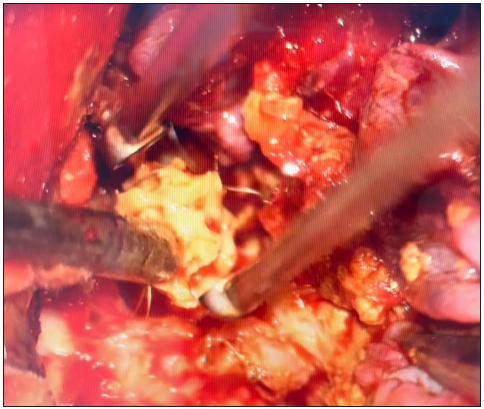
- Intraoperative microscopic view (viewed through left pterional approach) showing yellowish fatty material and hair during the evacuation of dermoid contents.
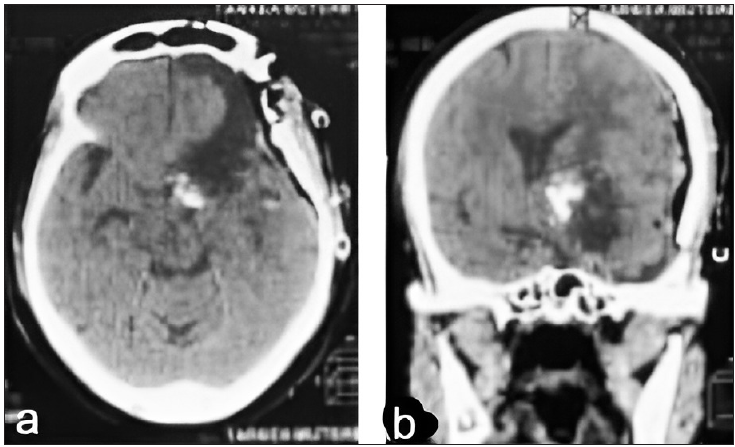
- (a) Postoperative brain CT scan axial view showed complete removal of the mass with residual part of calcification, (b) Postoperative brain CT scan coronal view showed complete removal of the mass with residual part of calcification. CT: Computed tomography.
Furthermore, the patient was discharged six days after surgery. Histopathology report shows the stratified squamous epithelium with its adnexa and foreign body giant cell reaction, confirming the diagnosis of a DC.
DISCUSSION
Intracranial DCs are rare cystic lesions that are supposed to originate from the ectopic ectodermal remnants in the course of the neural tube closure during the third to the fifth month of embryonic development.[2] They contain a fibrous capsule formed by stratified squamous epithelium, and the cyst has dermal attachments such as hair follicles, sebaceous glands, or sweat glands.[2,3]
The literature reports a single analogous instance of a pediatric patient with suprasellar DCs exhibiting radiological characteristics that resembled those of craniopharyngioma.[5] In this case, the DC presented with radiological features that can mimic both craniopharyngioma and meningioma. The identification of an isodense mass in the sphenoid ridge region with calcification on CT scan coupled with the lack of peripheral edema gives rise to the possibility of sphenoid wing meningioma. Brain MRI revealed an imaging pattern that suggested the presence of fatty tissue and raised the possibility of craniopharyngioma as a significant differential diagnosis. The machine oil-like fluid was evacuated intraoperatively, which closely resembled the typical fluid of craniopharyngioma, thereby precluding DCs inclusion in the preliminary differential diagnosis.
The typical appearance of DCs can be readily identified through imaging techniques. On CT scans, they appear hypodense owing to their lipid content, while on MRI, they exhibit hyperintense characteristics on both T1WI and Fluid-attenuated inversion recovery (FLAIR) is an advanced magnetic resonance imaging sequences, with variable signals ranging from hypointense to hyperintense on T2WI. These types of cysts do not enhance with contrast.[3,6] However, DCs may present with atypical radiological findings on CT and MRI. They may appear hyperdense on CT scan due to the high protein content of the lesion, while hypointensity on MRI is mostly attributed to saponification of lipid or keratinized debris, along with secondary microcalcification in suspension.[7] Along with a broad spectrum of lesions, ranging from benign cysts to malignant tumors can manifest in the suprasellar and parasellar regions. Although the differential diagnoses for these lesions are extensive, the clinical presentation of these lesions typically varies in severity.[8] Suprasellar DCs tend to be located in the midline above the sella turcica, and this location can often mimic other sellar tumors.[3] Craniopharyngiomas are considered the most common lesions that occur exclusively in the suprasellar region.[9] The imaging characteristics of craniopharyngioma typically reveal calcifications and cysts on CT scans and MRI.(10) Calcifications in craniopharyngiomas are present in approximately 80% of the cases and may be nodular or curvilinear.[9] Although cysts are present in almost all cases of craniopharyngiomas, the cystic portions tend to predominate in children while the solid parts are more prominent in adults. The solid portions and cystic walls of all craniopharyngiomas typically enhance, often heterogeneously. It has been suggested that edema spreading along the optic tract may be a specific sign of craniopharyngioma[9,10]. However, meningiomas are the second most common tumor in the sellar region in adults, with pituitary macroadenomas being the most common. Approximately 5%–10% of meningiomas occur in this region.[11] A CT scan typically shows hyperostosis of the surrounding bone and intratumoral calcification. MRI is the imaging modality of choice for meningiomas; they are isointense to grey matter on T1WI and iso-to-mildly-hyperintense on T2WI, with intense enhancement visible after the administration of medium contrast.[12]
In our case, a brain CT scan showed an iso-to-hyperdense suprasellar lesion extended to the left parasellar area with intralesional calcification. The presence of isodensity mass in the area of the sphenoid ridge with calcification on CT scan and the absence of peripheral edema raises the suspicion of sphenoid wing meningioma. However, extreme sellar extension was a point against this suspicion. On the brain MRI, we noticed a partially calcified non-cystic suprasellar and more in the left sphenoid lesion that was hyperintense on T1WI and hyper to mixed signal on T2WI, with gadolinium enhancement. This presentation suggests a fatty tissue signal, making us think about craniopharyngioma as an important differential diagnosis. However, the later extension to the sphenoid ridge and the absence of extension to the third ventricle were not quite typical features of craniopharyngioma. No other features were referring to DCs, which led to excluding it from the preoperative differential diagnosis list. Intraoperatively, the color of the evacuated fluid was like machine oil, which is very comparable to the typical fluid of craniopharyngioma. We identified the DC only during the dissection of the lesion when we encountered several hair follicles within the lesion, confirmed by the histopathological report that demonstrated stratified squamous epithelium with its adnexa (eccrine glands and hair follicles), fibrous wall, and foreign body giant cell reaction.
In summary, this case report highlights the importance of considering suprasellar DC as a potential differential diagnosis in patients presenting with symptoms suggestive of a tumor; we describe the challenge scenario where a DC mimics meningioma and craniopharyngioma tumors in the sellar region.
CONCLUSION
Intracranial DCs may present with clinical and radiological features similar to those of the more commonly encountered suprasellar tumors such as craniopharyngiomas and meningiomas, and hence should be included in the differential diagnosis of such tumors. This is particularly relevant when the DC is located in the suprasellar region and demonstrates imaging characteristics that are non-cystic and not hypodense.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- A rare case of an intracranial dermoid cyst with atypical appearance on computed tomography and magnetic resonance imaging. Am J Case Rep. 2022;23:e935115.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Intrasellar dermoid cyst mimicking pituitary apoplexy: A case report and review of the literature. J Clin Neurosci. 2017;45:125-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperdense suprasellar mass: An unusual radiological presentation of intracranial dermoid cyst. J Clin Neurosci. 2015;22:1208-10.
- [CrossRef] [PubMed] [Google Scholar]
- Frontal dermoid cyst coexisting with suprasellar craniopharyngioma: A spectrum of ectodermally derived epithelial-lined cystic lesions? Neurosurg Focus. 2016;41:E16.
- [CrossRef] [Google Scholar]
- Child dermoid cyst mimicking a craniopharyngioma: The benefit of MRI T2-weighted diffusion sequence. Childs Nerv Syst. 2018;34:359-62.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical imaging features of posterior fossa’s dermoid cyst: Case report and review of literature. Surg Neurol Int. 2018;9:97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An unusual CT and MR appearance of a posterior fossa dermoid. Eur J Radiol. 1995;20:46-7.
- [CrossRef] [PubMed] [Google Scholar]
- Masses of the sellar and juxtasellar region. In: Drevelegas A., ed. Imaging of brain tumors with histological correlations. Berlin, Heidelberg: Springer; 2002. p. :227-52.
- [Google Scholar]
- T1 signal hyperintensity in the sellar region: Spectrum of findings. Radiographics. 2006;26:93-113.
- [CrossRef] [PubMed] [Google Scholar]
- Craniopharyngioma and other cystic epithelial lesions of the sellar region: A review of clinical, imaging, and histopathological relationships. Neurosurg Focus. 2010;28:E4.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging characteristics of common suprasellar lesions with emphasis on MRI findings. Clin Radiol. 2008;63:939-47.
- [Google Scholar]








