Translate this page into:
Rare lung cancer subtype discovery by bone metastases: Synchronous traits
*Corresponding author: Dr. Souhail El Alami, Department of Orthopaedic Surgery, Mohammed V Military Instruction Hospital, Rabat, Morocco. dr.s.elalami@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: El Alami S, Laraichi A, Abakka M, El Ghoul N, El Aouni S, Bennis A, et al. Rare lung cancer subtype discovery by bone metastases: Synchronous traits. Asian J Oncol, 2023;9:5.
Abstract
This study investigates the synchronous traits of a rare lung cancer subtype, specifically Large Cell Neuroendocrine Carcinoma (LCNEC), discovered through bone metastases. Bone metastases are a common occurrence in lung cancer, significantly impacting the quality of life and survival of patients. Synchronous bone metastasis (SBM), defined as bone metastases diagnosed within three months of lung cancer diagnosis, and metachronous bone metastasis (MBM), diagnosed more than three months after lung cancer diagnosis, exhibit distinct clinicopathological characteristics, therapeutic sensitivities, and prognostic outcomes. This article presents a visual case discussion of a 64-year-old male patient who experienced a pathological fracture of the proximal femur, leading to the incidental discovery of LCNEC through bone biopsy. Further imaging and diagnostic tests confirmed the presence of a primary lung tumor and bone metastases. The treatment approach for LCNEC remains challenging due to limited data and varying outcomes reported in the literature, however our patient received cisplatin with etoposide chemotherapy following fracture management. The findings emphasize the importance of recognizing rare lung cancer subtypes, such as LCNEC, through bone metastases and tailoring individualized treatment plans.
Keywords
Bone metastases
Lung cancer
Synchronous
Large cell
Neuroendocrine carcinoma
CASE PRESENTATION
We present the case of a 64-year-old male patient with no significant medical history, working in a construction site, who presented to the emergency department with right lower limb pain and deformity following direct trauma to the right thigh from a heavy solid object dropped from a 2-meter height. The patient was immediately unable to bear weight on the affected leg and exhibited external rotation and shortening. Mild swelling and bruises were observed during physical examination. Radiographic imaging of the hips and femur revealed a pathological fracture of the proximal femur accompanied by Moth Eaten bone destruction lesions.
INTRODUCTION
Lung cancer is a complex disease with various subtypes that present unique challenges in diagnosis and treatment. While the most common types of lung cancer, such as adenocarcinoma and squamous cell carcinoma, have been extensively studied, rare subtypes remain less understood. In recent years, the discovery of rare lung cancer subtypes through bone metastases has emerged as a valuable approach, providing new insights into the molecular characteristics and clinical features of these subtypes. This article aims to explore the synchronous traits of a rare lung cancer subtype identified through bone metastases, shedding light on its diagnosis, prognosis, and potential therapeutic implications.
DISCUSSION
One of the most tragic complications of lung cancers are metastases to bones. Around 30 to 40% of patients with advanced lung cancer eventually develop this complication.[1] Roughly, 5.93% of newly discovered lung cancer patients had bone metastases. However, the accidental discovery of lung cancer through a skeletal-related event is not common, and a rare lung cancer entity being involved is even less common, such as large cell neuroendocrine carcinoma which represents a rare lung cancer subtype for which progress in management has fallen behind the significant developments seen in non-small cell lung cancer (NSCLC) using targeted therapies and checkpoint inhibitors.
Due to a special microenvironment in the bone matrix, bone was accepted to be one of the most common distal metastatic sites, especially for lung cancer.
Bone metastases is closely associated with compromised quality of life and shortened survival of the patients. The median survival of patients with bone metastases is 6–8 months, even after aggressive treatment.
Synchronous bone metastasis (SBM) is defined as the diagnosis of bone metastases within 3 months of lung cancer diagnosis, while metachronous bone metastasis (MBM) is defined as bone metastases diagnosis more than 3 months after lung cancer diagnosis.[2]
Synchronous and metachronous bone metastases in lung cancer may represent distinct clinicopathological characteristics, therapeutic sensitivity, and prognostic which resulted in creating individualized treatment plans.
Bone metastasis is the leading cause of pain and increases the risk of skeletal-related events in cancer patients.
Pain often starts gradually, giving the feeling of a muscle strain, before becoming severe. In advanced stages of cancer, the bone can weaken and lead to pathologic fractures.
The slow dissolution of bone can also increase calcium levels in blood. This can generate hypercalcemia, which can lead to confusion, muscle weakness, and loss of appetite.
The primary goal of treatment is to reduce pain and prevent fractures. Options include pain medications, radiation, surgery, and drugs used to slow the breakdown of bones.
Three prognostic factors in lung cancer patients with SBM were smoking, high level of neuron-specific enolase (NSE) and histological type.[2]
VISUAL CASE DISCUSSION
We report the case of a 64-year-old male patient, with no significant medical history working in a construction site, who came to the emergency department with right lower limb pain and deformity after receiving a heavy solid object from a 2-meter height, directly on the right thigh.
Immediately after the incident, the patient was unable to bear any weight on it directly. During physical examination, his right leg was shorter and in external rotation. Mild swelling and bruises were objectified. A radiograph of his hips and femur showed what appeared to be a pathological fracture of the proximal femur along with moth-eaten bone destruction lesions [Figures 1 and 2].
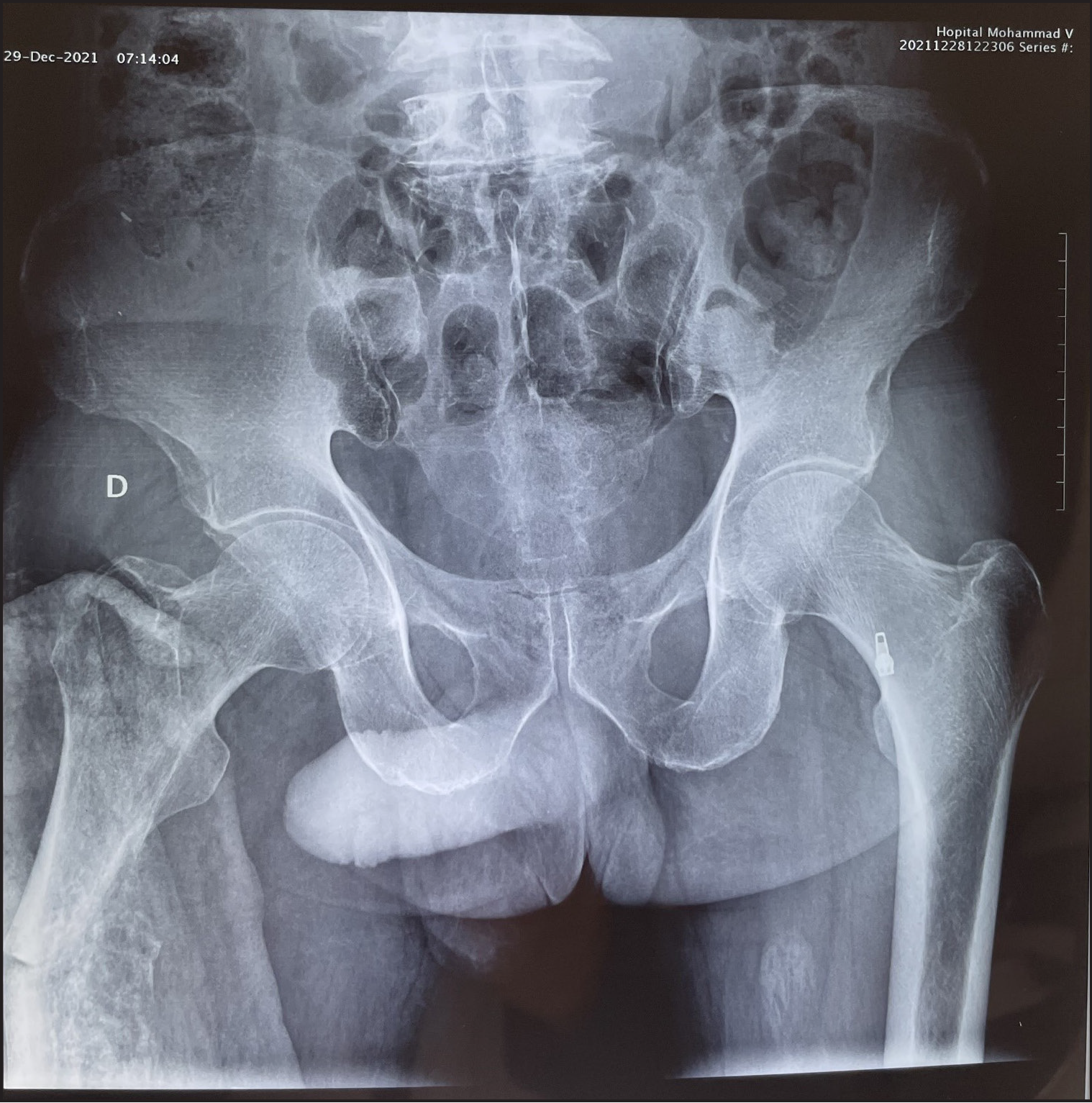
- Pelvic radiograph on AP view showing the proximal extension of the bone metastases.

- Standard AP view depicting the pathological fracture of the proximal femur along with Moth Eaten bone destruction lesions.
In this study, we conducted a comprehensive investigation, starting with a bone biopsy, which revealed immunohistochemical profile in favor of a secondary location of a lung large cell neuroendocrine carcinoma (LCNEC) which is a rare pulmonary tumor, with features of both small cell lung cancer (SCLC) and NSCLC.
After this, the patient underwent a series of screening tests, starting with a chest x-ray, which showed a unilateral pulmonary hilar mass [Figure 3], followed by a CT-scan that revealed a right upper lobe tumor along with multiple bilateral nodules in lung parenchyma [Figures 4 and 5]. Hypercalcemia, a frequent skeletal-related event, was present at a level of 13.4 mg/dL in his blood work, along with NSE serum levels at 290.48 ng/mL.
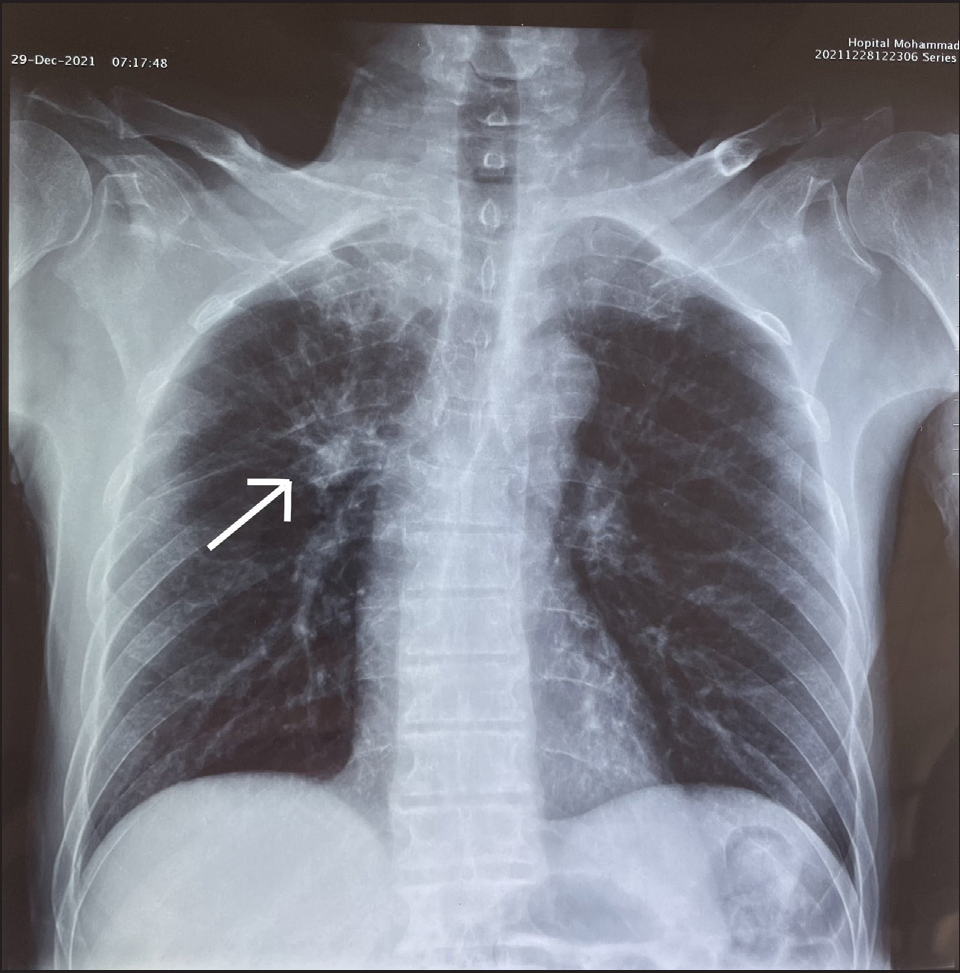
- Chest x-ray revealing a right hilar mass (white arrow).
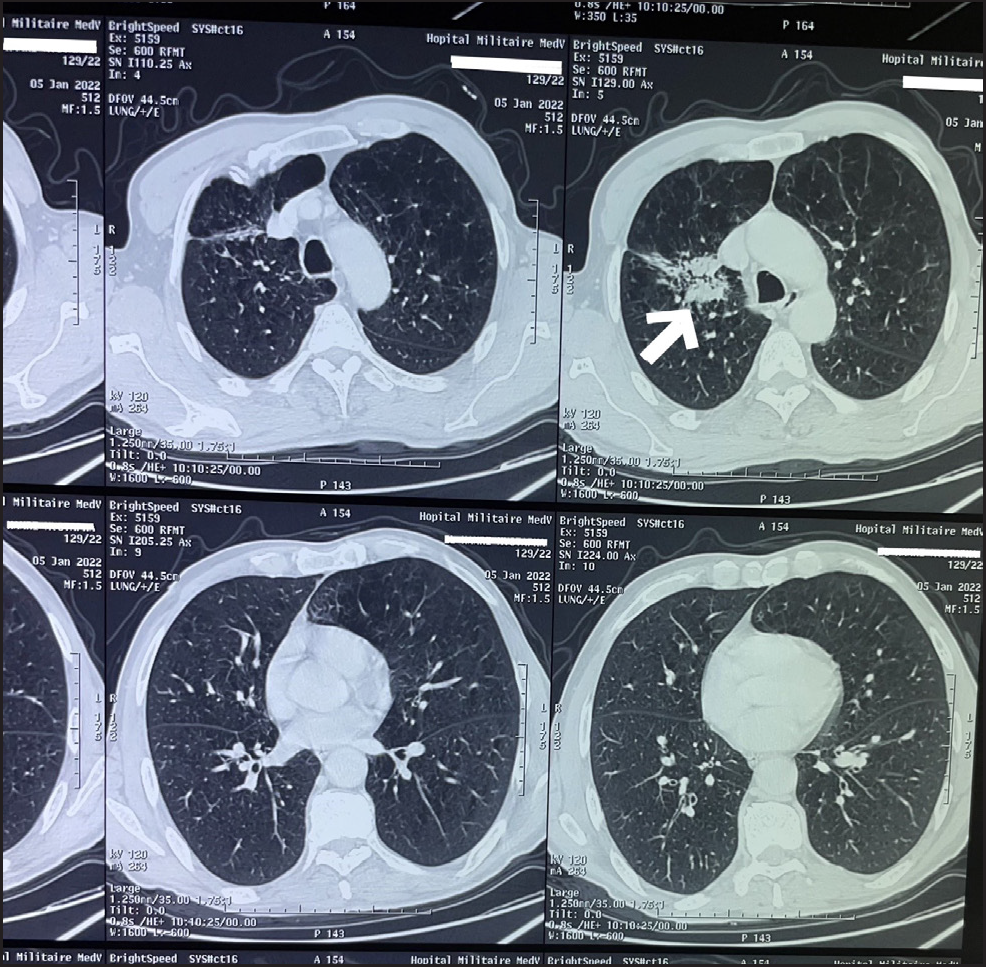
- CT-scan in favor of a right upper lobe tumor along with multiple bilateral nodules in lung parenchyma (White arrow).
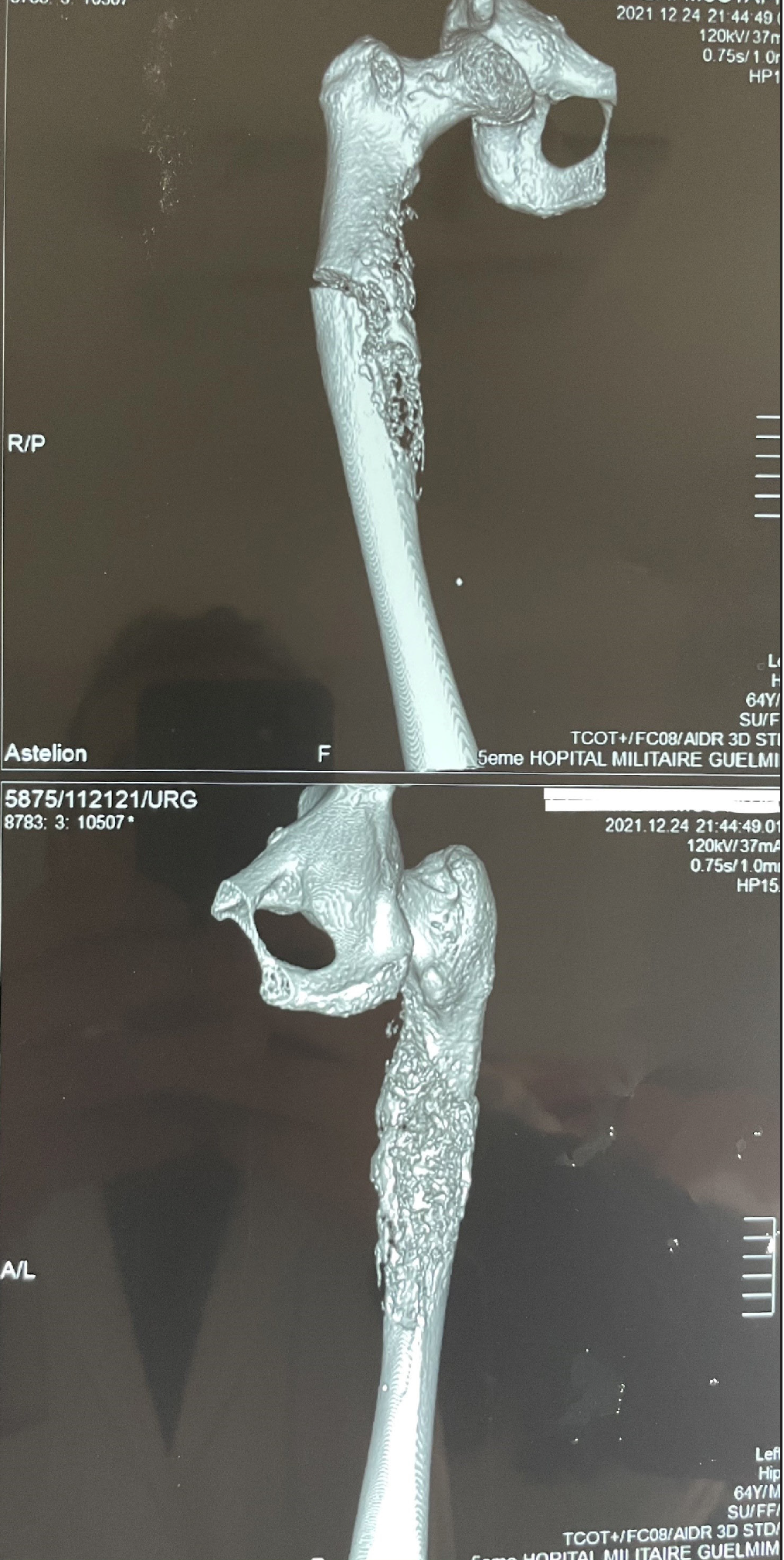
- 3D reconstruction CT of the pathologic fracture.
MRI revealed a metaphyseal–diaphyseal lesion of the right femur with intramedullary extension invading adjacent soft tissues and complicated with a pathologic fracture [Figure 6].
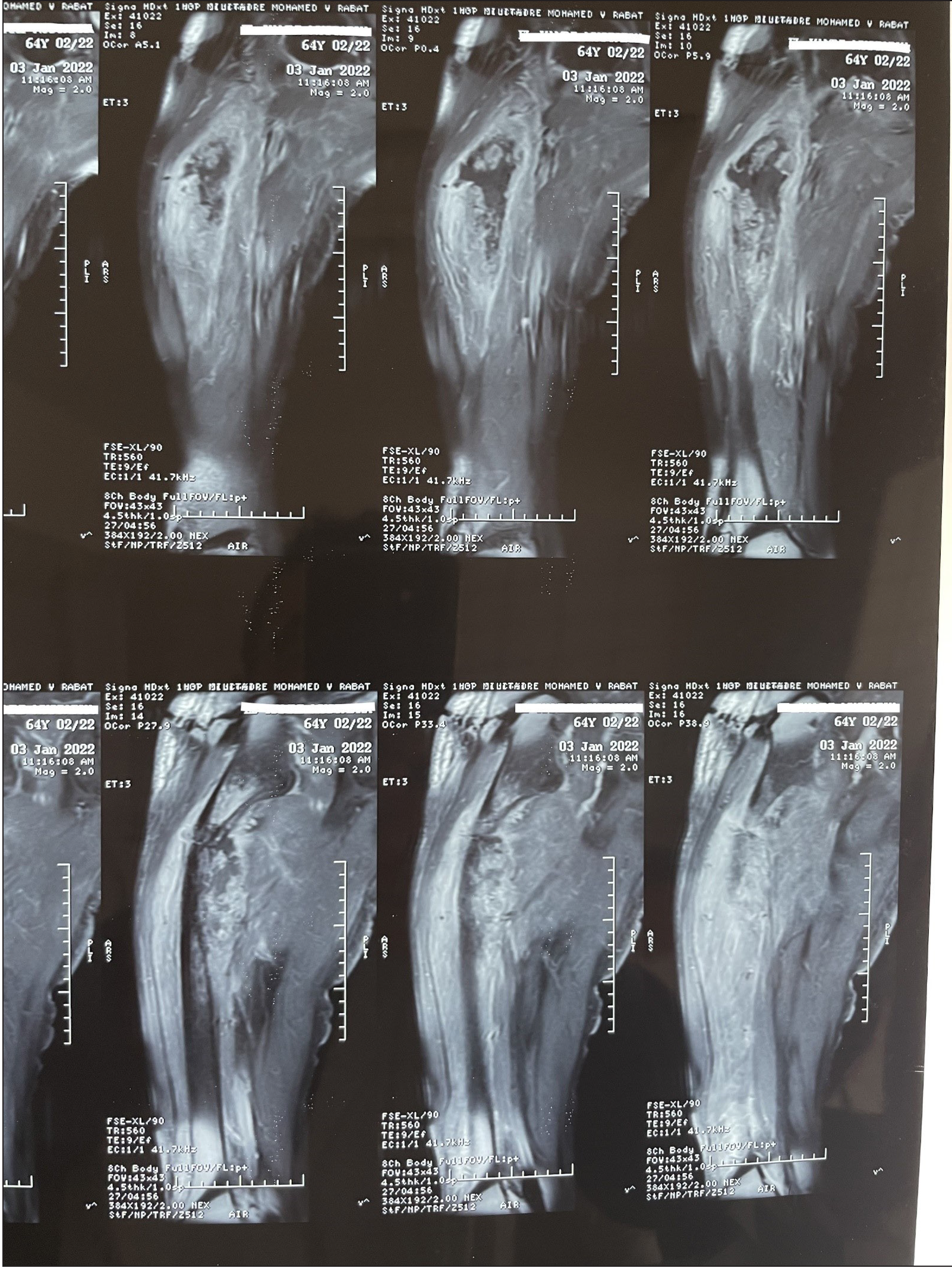
- MRI showing a metaphyseal-diaphyseal lesion of the right femur with intramedullary extension invading adjacent soft tissues and complicated with a pathologic fracture.
Although unspecific, a technetium-99 m bone scintigraphy was performed on the patient given its high sensitivity and ability to detect lesions earlier than that observed in plain radiographs, which revealed intense hyperfixation within the right proximal femoral diaphysis [Figure 7].
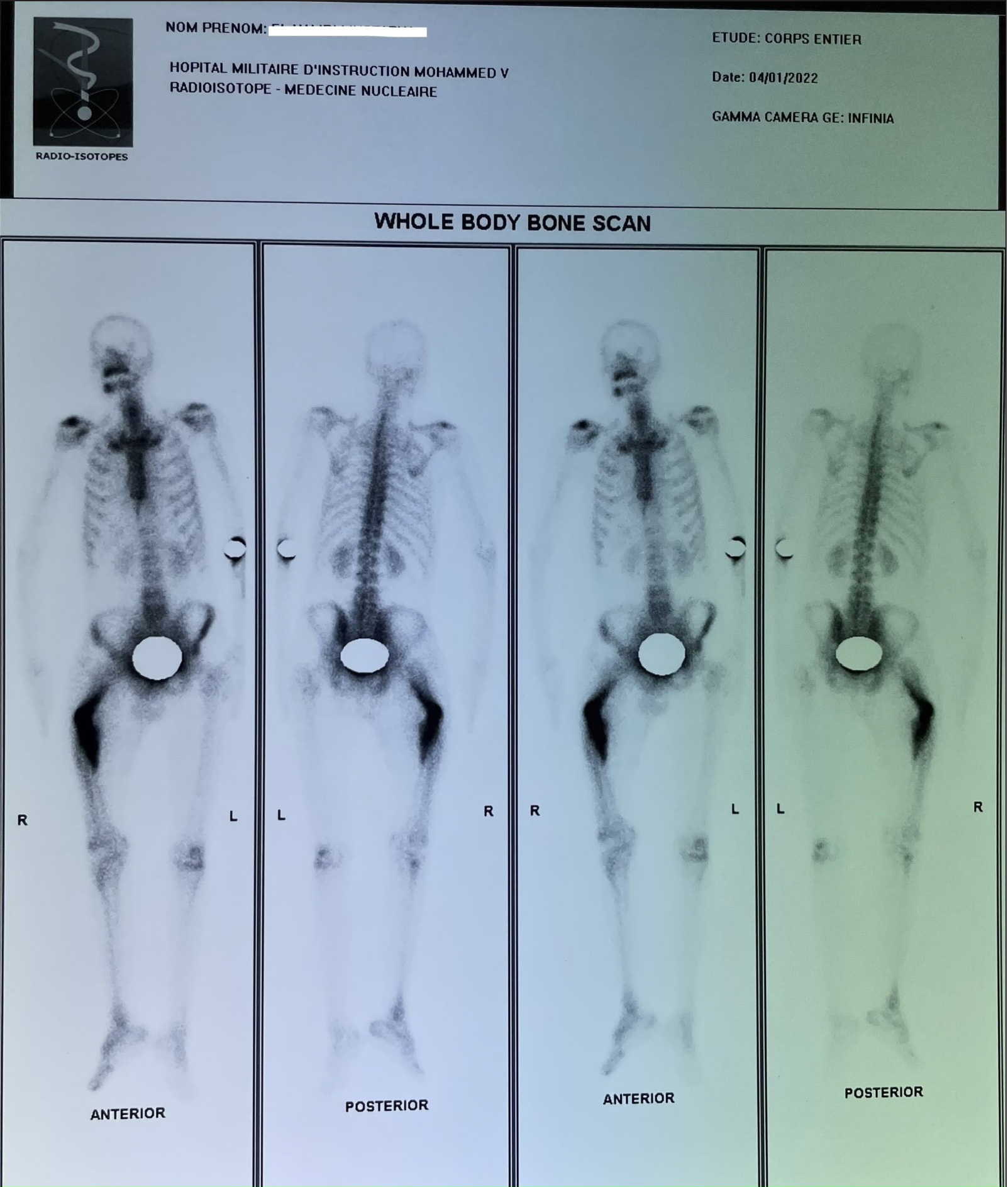
- Technetium-99m bone scintigraphy revealing Intense hyperfixation within the right proximal femoral diaphysis.
PET CT scans are widely used to stage patients and assess treatment response, while producing high resolution images and detecting increased metabolic activity in oncologic lesions. In our case, it revealed intense hypermetabolic, right parahilar activity related to a parenchymal mass, measuring 40 × 35 mm corresponding to the known primitive, associated with multiple small, moderately hypermetabolic lymph node foci, pre- and subcarinal of SUVmax 3.4 and 3.3, respectively.
We eventually proceeded with a lung biopsy that was concordant with our first diagnosis [Figures 8–10].
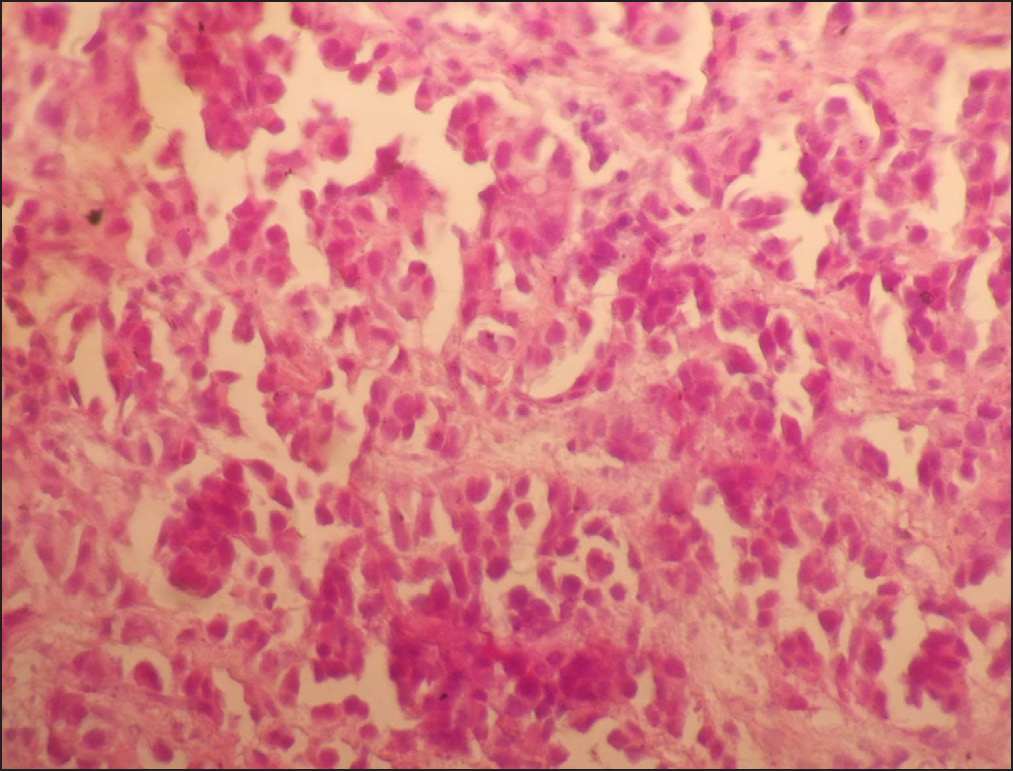
- Microscopic view showing tumor cell proliferation of solid architecture made of cells large in size and with large nuclei often nucleolated at 400x magnification under light micrograph.
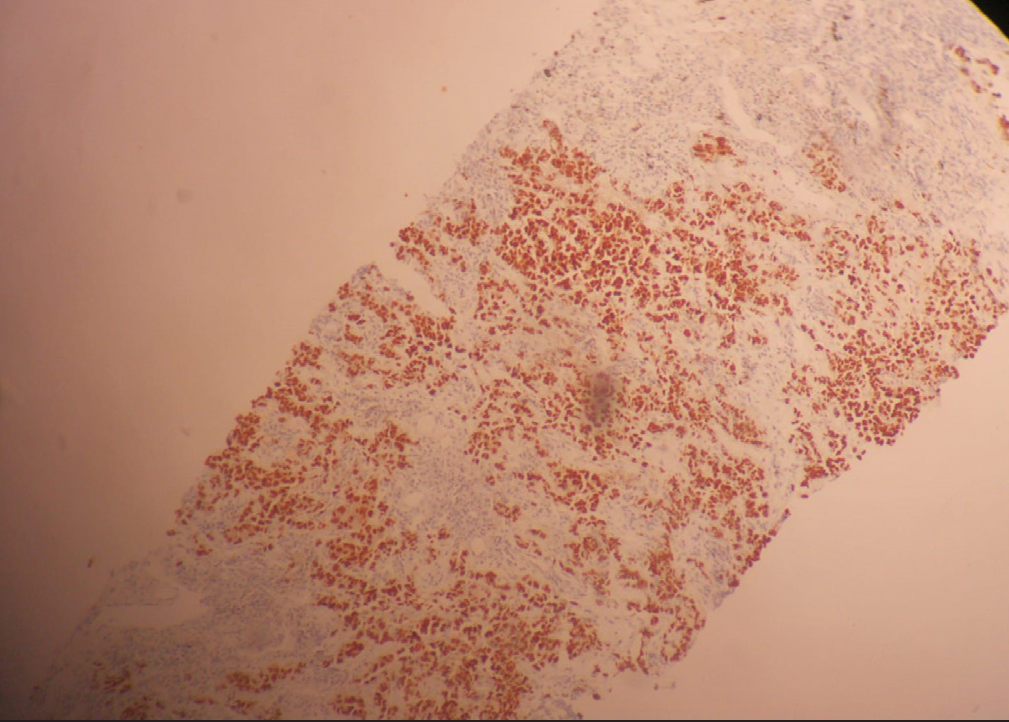
- Immunohistochemistry image revealing nuclear TTF-1 positivity by tumor cells demonstrating the pulmonary origin.
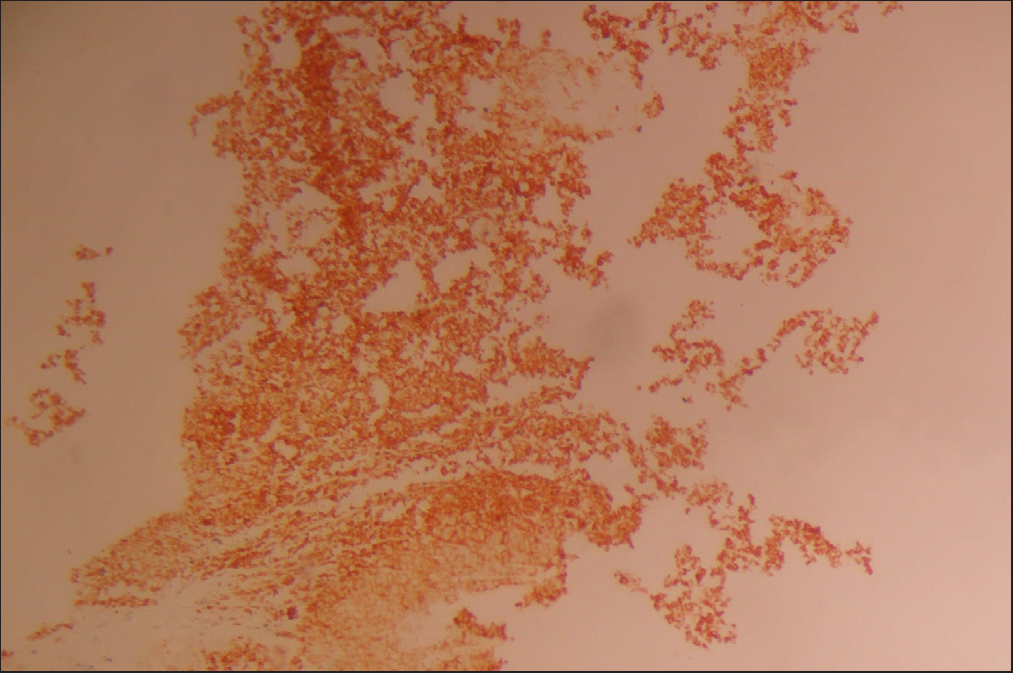
- Immunohistochemistry image depicting synaptophysin-positive tumor cells in favor a neuroendocrine tumor.
LCNEC is a rare, aggressive, and difficult-to-treat tumor.
The optimal treatment strategy for LCNEC is debated, given limited data and different outcomes based on chemotherapy type reported in the available literature.
Our patient first received a long gamma nail for his pathologic fracture to allow early weight bearing [Figure 11], and then was presented to our fellow oncologists for further chemotherapy that eventually consisted of cisplatin with etoposide.

- Post operative standard AP radiograph view of the long gamma nail used for the pathologic fracture fixation.
CONCLUSION
In conclusion, the identification of rare lung cancer subtypes through bone metastases offers a promising avenue for research and clinical practice. The synchronous traits observed in this particular subtype provide valuable insights into its molecular profile, clinical behavior, and potential therapeutic targets. Understanding the distinct characteristics of rare lung cancer subtypes can guide personalized treatment strategies and improve patient outcomes. Further studies and collaborations are warranted to validate these findings and expand our knowledge of this subtype and its implications for precision medicine in lung cancer.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Bone metastases: When and how lung cancer interacts with bone. World J Clin Oncol. 2014;5:149-55.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Synchronous bone metastasis in lung cancer: Retrospective study of a single center of 15,716 patients from Tianjin, China. BMC Cancer. 2021;21:613.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







