Translate this page into:
Primary Bilateral Ovarian Lymphoma: A Rare Case Report
Address for correspondence Salwa Bano, DNBNo. 120, F2, Emaar Paradise, 4th Main, 2nd Cross, BTM 1st Stage, Bangalore, KarnatakaIndia 560029dr.salwakhattab87@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary ovarian lymphomas constitute 0.5% of all ovarian malignancies. We report one such case in a middle-aged woman who presented with a bilateral ovarian tumor. Bilateral oophorectomy with salpingectomy was sent for frozen section analysis that revealed a round cell tumor. Final histopathology showed a mitotically active small round blue cell tumor arranged in diffuse sheets and chords with an evident starry-sky pattern. Extensive immunohistochemistry (IHC) panel was performed. Histopathology along with IHC did not classify the tumor into diffuse-large-B cell-lymphoma or Burkitt lymphoma and a final diagnosis of high-grade B cell lymphoma (HGBL) was made. This case is presented for its rarity and to discuss the challenges on IHC to subclassify a lymphoma as HGBL. Although rare, the possibility of primary ovarian non-Hodgkin lymphoma should be kept in mind when dealing with bilateral ovarian tumors as a timely and accurate diagnosis can save unnecessary surgeries and improve outcome.
Keywords
primary ovarian lymphoma
high-grade B cell lymphoma
bilateral ovarian non-hodgkin lymphoma
Key Message
Primary ovarian lymphoma (POL) is a rare entity, more so is the existence of high-grade B cell lymphoma. As the treatment plan and prognosis significantly changes for POL as compared with ovarian carcinoma, this entity should be kept in mind for all morphologically round blue cell tumors seen in ovaries.
Introduction
Primary ovarian lymphomas (POL) are rare.1 Alternatively, less than 0.5% tumors arising in the ovary are lymphomas.1 It is seen in patients of all age groups and usually presents with a unilateral ovarian mass.1 Both B cell and T cell non-Hodgkin lymphoma (NHL) can potentially arise in the ovary.2 However, more common is B cell derived-lymphomas.1 We report a case of high-grade B cell lymphoma (HGBL) of bilateral ovaries seen in a 37-year-old patient. Other tumors were ruled out on morphology along with immunohistochemistry (IHC).2
Incidence of HGBL in ovaries is unknown. As the treatment plan and prognosis significantly change for POL as compared with ovarian carcinoma, this entity should be kept in mind for all morphologically round blue cell tumors seen in ovaries.2
Case History
A 37-year-old woman presented with pain and distension of the abdomen. Menstrual history was unremarkable. General examination revealed mild pallor without evidence of hepatosplenomegaly or lymphadenopathy. Per-abdomen examination revealed a mass in the left iliac fossa with mild tenderness. The patient had no significant past history. Blood tests showed mild anemia. Biochemical tests, including serum calcium levels, were within normal limits. Tumor marker CA-125 was marginally elevated.
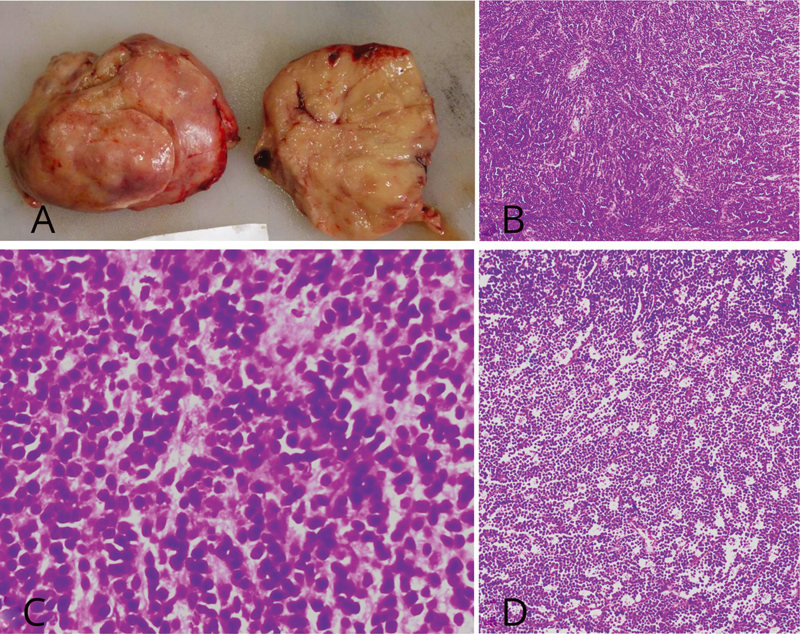
On ultrasonography, both ovaries showed heterogeneous masses measuring approximately 98 × 85 × 79mm on the left and 48 × 40 × 35mm on the right side. The radiological and clinical impression was of bilateral ovarian carcinoma. The lesion was not biopsied, instead bilateral salpingo-oophorectomy was planned and sent for frozen section assessment. Gross specimen of the left ovarian mass measured 95 × 90 × 80mm and the right mass measured 45 × 40 × 30mm. Externally, the capsule was intact in both masses and the cut surfaces showed entire ovarian parenchyma replaced by a soft, solid, homogenous, and grayish-white tumor (Fig. 1A). On frozen section, a presumptive diagnosis of “round blue cell tumor involving both ovaries” was given and a differential of small cell carcinoma of the ovary versus lymphoma of the ovary was offered.
-
Fig. 1 (A) Gross picture of the left ovarian mass showing a solid, homogenous, soft, gray-white tumor entirely replacing the normal ovarian parenchyma. The capsule is intact. No areas of hemorrhage or necrosis were seen. (B) Hematoxylin and eosin (H and E) stain;4x; sections show a malignant tumor with cells arranged in diffuse sheets and chords. No normal ovarian parenchyma is seen. (C) H and E stain;10x; tumor cells are medium to large-sized, having a moderate amount of cytoplasm. (D) H and E stain;4x; A starry-sky pattern is evident on low power view that is characteristic of Burkitt lymphoma.
Histopathological examination of the mass revealed a malignant tumor with cells arranged in diffuse sheets and chords (Fig. 1B) and composed of medium to large-sized round to ovoid cells having a moderate amount of cytoplasm (Fig. 1C). Most of the cells showed prominent nucleoli. Occasional anaplastic cells were seen. The tumor was mitotically very active (20–25 mitosis/10 high power field). A starry-sky pattern, characteristic of Burkitt lymphoma (BL), was noted on low power view (Fig. 1D). Cytoplasmic hyaline globules and tumor necrosis, notable feature of small cell carcinoma of the ovary, were not identified.
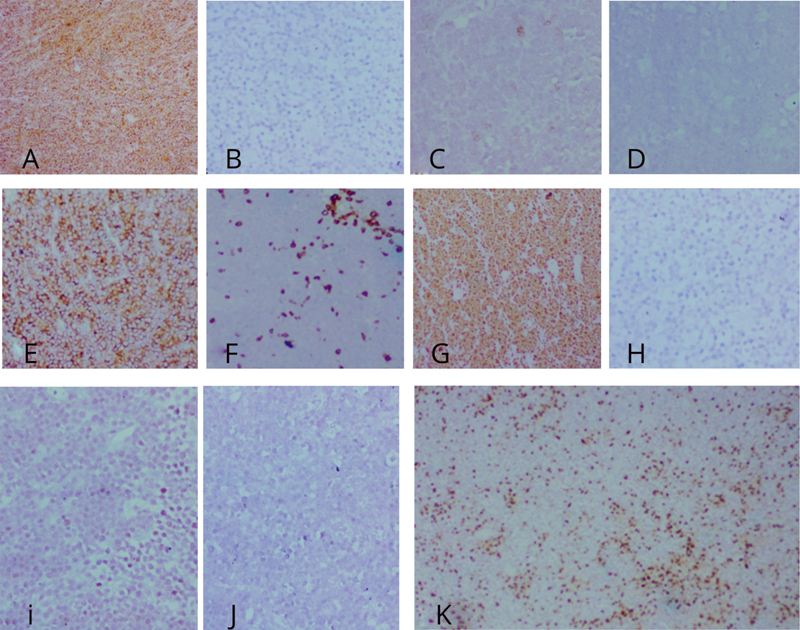
On IHC, tumor cells were immunoreactive for leukocyte common antigen and negative for vimentin, CD99, and cytokeratin (Fig. 2A–D) narrowing the diagnosis to lymphoma and ruling out possibility of small cell carcinoma, Ewing's sarcoma/peripheral neuroectodermal tumor, and epithelial tumors of ovary, respectively. Tumor cells were diffusely positive for CD20, negative for CD3, and showed a high proliferative index (Fig. 2E–G), hinting at a B cell-derived lymphoma.
-
Fig. 2 Immunohistochemistry immunoreactivity of tumor cells shows positivity for leukocyte common antigen (A) and negative for vimentin (B), CD99 (C), and cytokeratin (D). Immunoreactivity for CD 20 (E) is bright and diffuse, while CD 3 (F) is seen highlighting only the background T cells. Ki 67 proliferative index (G) is almost 100%. These features imply a high-grade B cell-derived lymphoma. Immunonegativity for Tdt (H), Alk protein (I), and cyclin D1 (J) rule out close differentials. Strong reactivity for Bcl2 (K) hints toward the diagnosis of high-grade B cell lymphoma as Burkitt lymphoma is typically negative or weakly positive for Bcl2.
Immunonegativity for Tdt, Alk protein, and cyclin D1 ruled out lymphoblastic lymphoma, anaplastic large cell lymphoma, and blastic variant of mantle cell lymphoma, respectively (Fig. 2H–J). Further IHC was done to differentiate between DLBCL and BL. C-myc IHC staining and analysis for MYC gene was not attempted as it is seen in both the entities in varying proportion.3 Further IHC showed strong reactivity for Bcl2 (Fig. 2K). BL is typically negative for this antiapoptotic marker; however, weak expression may be seen in some cases.4 However, in the present case, a diffuse and strong positivity of Bcl2 was suggestive of an additional BCL2 breakpoint consistent with HGBL (with MYC and BCL2 and/or BCL6 rearrangements).4
IHC was also done for BCL6, Mum 1, and CD10, which showed weak immunoreactivity in more than 30% of tumor cells for all three markers. This is a known pattern of reactivity in DLBCL cases.4
Available clinical and morphological studies could not classify this entity into either DLBCL or a BL that are the common types of NHL seen in POLs.6 However, as quoted above, strong immunohistochemical reactivity for BCL2 hinted toward a diagnosis of “High-grade B-cell lymphoma” (previously called “B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and Burkitt lymphoma”). Genetic studies to subclassify HGBL into not otherwise specified type or HGBL with MYC and BCL2 and/or BCL6 rearrangements were not available.
Discussion
Involvement of the ovary in lymphomatous process is rare and it may occur in two ways: primary or secondary.6 Although both B cell and T cell NHL can arise in the ovaries,2 literature suggests that nearly all primary lymphomas (92%) of the ovary are B cell neoplasms.2 DLBCL appears to be the most common type of primary ovarian NHL1,5 followed by BL and follicular lymphoma.1 The incidence of HGBL in bilateral ovaries is unknown.
HGBL is a new entity added in the 2017 classification of World Health Organization (WHO) hematolymphoid tumors that is defined as aggressive, mature B cell lymphomas with MYC and BCL2 and/or BCL6 rearrangements or in absence of these rearrangements have features intermediate between DLBCL and BL or appear blastoid.4 Most cases of HGBL exhibit morphology resembling DLBCL (medium-size to large cells, abundant cytoplasm, irregular nuclear contours),4 while a small portion may have a blastoid appearance.4 Half the cases show a morphology resembling BL4 (medium-size to large cells with large nuclei, monomorphic and with starry sky macrophages)4 or, as seen in our case, features intermediate between DLBCL and BL(larger cells with less basophilic cytoplasm).4
IHC plays a limited role in the diagnosis of HGBL, as BL, DLBCL, and HGBL are variably reactive for most markers7 nevertheless, high BCL 2 positivity is suggestive of HGBL, and weak positivity may be seen in BL.4
Although rare, the possibility of primary ovarian non-Hodgkin lymphoma (PONHL) should be kept in mind when dealing with bilateral ovarian tumors as ovarian lymphomas are treated significantly different from ovarian carcinomas. The treatment principles and prognosis for PONHL remain the same as that of other nodal NHLs,2 yet the outcome of PONHL remains worse (0–36% cases expected to survive less than 3 years) due to delayed and incorrect diagnosis and treatment.5
Conclusion
POL constitutes a minority of ovarian malignancies1 nevertheless, the possibility should be considered in bilateral ovarian tumors to prevent inaccurate diagnosis and incorrect treatment.3
Conflict of Interest
None declared.
References
- Lymphoid and myeloid tumors In: Robert J K, Maria L C, Simon C H, Robert H Y, eds. WHO Classification of Tumours of Female Reproductive Organs (4th Edition,). Lyon: IARC Press; 2014.
- [Google Scholar]
- MYC Immunohistochemistry predicts MYC rearrangements by FISH. Front Oncol. 2017;7:209.
- [Google Scholar]
- WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues Lyon, France: International Agency for Research on Cancer; 2017.
- [Google Scholar]
- Five cases of non-hodgkin B-cell lymphoma of the ovary. Case Rep Obstet Gynecol.







