Translate this page into:
Novel method of identifying spinal accessory nerve during modified radical neck dissection in level 2: “SMS Hospital point” and “Upward Pointing Arrow” sign
*Corresponding author: Dr. Bhushan Sanjay Bhalgat, Surgical Oncology, Sahyadri Hospital, Shastrinagar, Pune, India. bhalgatbs@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhalgat BS. Novel method of identifying spinal accessory nerve during modified radical neck dissection in level 2: “SMS Hospital point” and “Upward Pointing Arrow” sign. Asian J Oncol, 2023;9:6.
Abstract
Neck dissection is now a part and parcel in management of oral malignancies. Like all other surgical procedures, it has a few morbidities, which include iatrogenic trauma to the spinal accessory nerve leading to atrophy of ipsilateral trapezius and sternocleidomastoid muscle. A few identification markers for the nerve have been described in the literature. The markers or structures described previously are not so accurate and give only an approximate idea of where the nerve could be. We have discovered a simple and easily reproducible marker and a sign which helps us identify the nerve each and every time without fail. The junction of posterior belly of digastric nerve, internal jugular vein, and spinal accessory nerve is the point where the proximal end of the nerve is found, and the structures together form an “upward pointing arrow” which helps identify the nerve precisely during neck dissection.
Keywords
Spinal accessory nerve
Operative technique
Identification
Level 2
Upward arrow sign
INTRODUCTION
Spinal accessory nerve is the eleventh cranial nerve. It courses through the neck in levels 2 and 5 dividing the levels into 2A and 2B, and 5A and 5B, respectively. It is a structure that has to be preserved during modified radical neck dissection to prevent loss of function of ipsilateral trapezius and sternocleidomastoid muscle. It is a very superficial structure in the neck in level 5. Every attempt has to be made to spare the nerve during neck dissection except in cases where extra nodal extension of malignancy is present around the nerve. Various ways to identify the nerve in levels 2 and 5 have been described and used practically by surgeons, of which “nerve point” (wrongly described in literature as Erb’s point) is the most widely.[1]
The literature lacks any simplified identification marker for the spinal accessory nerve in level 2.
After performing hundreds of neck dissections for oral cavity malignancies in our department in the past decade, we have found an innovative and simpler way of identifying the spinal accessory nerve in level 2.
TECHNIQUE
After having completed the level 1 dissection, the digastric muscle is stripped off of all the fibrofatty tissue and followed in superolateral direction upto its mastoid process insertion. Then, the sternocleidomastoid muscle is retracted laterally and the dissection proceeds through the angel hair tissue, hugging the sternocleidomastoid muscle along its entire length until one has a blurry visual of internal jugular vein (IJV). The IJV is then dissected on its medial surface in cranial direction upto its junction with posterior belly of digastric muscle, taking care of the medial tributaries, especially the common thyrofacial trunk. At the junction where the IJV meets the posterior belly of digastric muscle, just sweeping the tissue on lateral side of the IJV, one will always notice the proximal end of spinal accessory nerve running obliquely at an angle to the vein.
DISCUSSION
Radical neck dissection has been described by Crile in 1906,[2] and Bocca described the functional neck dissection in 1980.[3] Bocca encouraged surgeons around the world to avoid the major complications of radical neck dissection at no added oncological compromise. As per the current practice worldwide, spinal accessory, IJV, and the sternocleidomastoid muscle are preserved as and when possible, unless an extranodal extension into these structures is present.
To identify and preserve the spinal accessory nerve, various surgeons and anatomists have tried to find out the exact location of the spinal accessory nerve using the sternocleidomastoid, digastric muscle, vertebral process of C2,[4] IJV,[5] and the small veins near sternocleidomastoid muscle[6] as markers, but none of them are constant.
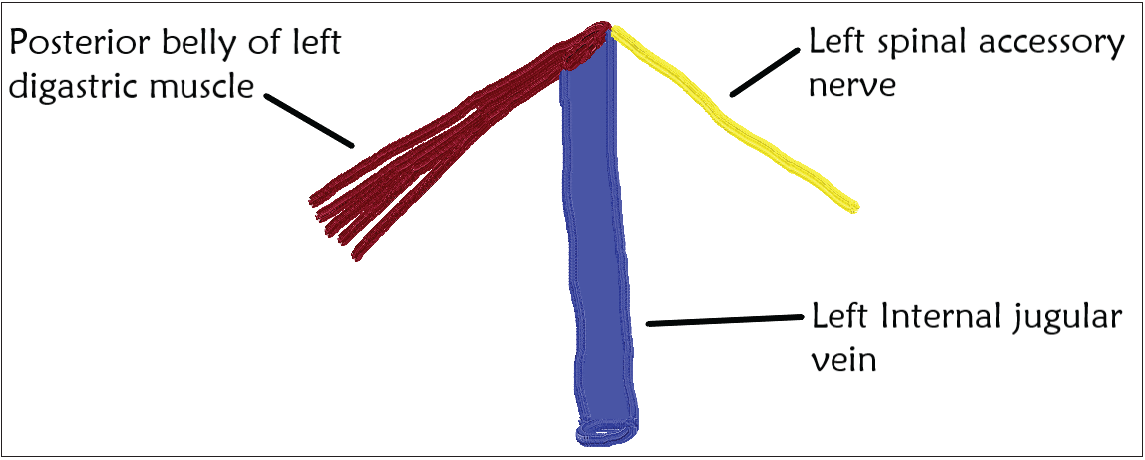
Hinsley et al. identified that the spinal accessory nerve travelled lateral to the IJV in the upper neck in 96% of the cases.[5] He, however, did not describe the ease with which this junction of posterior belly of digastric muscle, IJV, and spinal accessory nerve combined together could be used as an easy identification point for spinal accessory nerve in the anterior neck as shown in Figure 1.
![The diagram shows upper part left sided neck dissection. The junction of three structures namely posterior belly of digastric muscle, left internal jugular vein, and left spinal accessory nerve is seen forming an “upward pointing arrow” configuration. [Labels: 1- Left facial artery, 2- Lower end of left masseter, 3- Inferior cut end of left parotid gland, 4- Left sternocleidomastoid muscle, 5- Left common facial vein]](/content/155/2023/9/1/img/ASJO_52_2022-fig1.png)
- The diagram shows upper part left sided neck dissection. The junction of three structures namely posterior belly of digastric muscle, left internal jugular vein, and left spinal accessory nerve is seen forming an “upward pointing arrow” configuration. [Labels: 1- Left facial artery, 2- Lower end of left masseter, 3- Inferior cut end of left parotid gland, 4- Left sternocleidomastoid muscle, 5- Left common facial vein]
These three structures form an “upward pointing arrow” as shown in Figures 2 and 3.
- Diagrammatic representation of “SMS hospital” point which denotes the junction of posterior belly of digastric muscle, internal jugular vein, and spinal accessory nerve. (This diagram shows the left sided structures only; but similar point denotes the junction on right side too.)
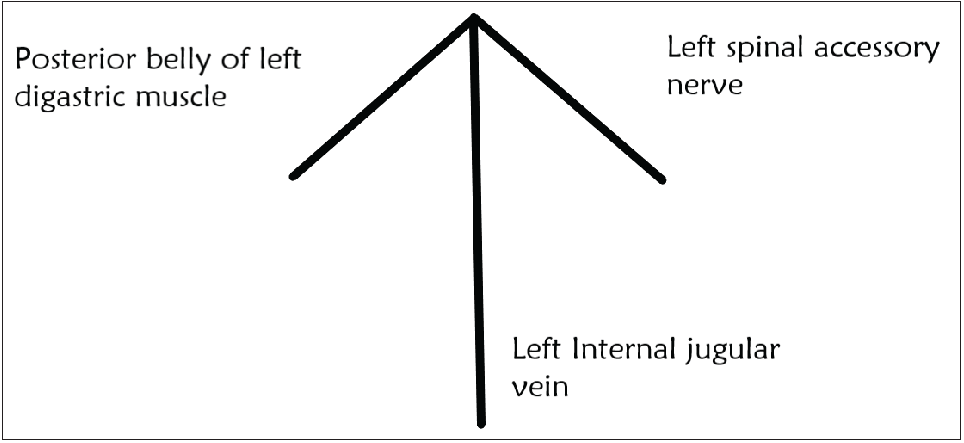
- Geometric representation of the “upward pointing arrow” sign formed by posterior belly of digastric muscle, internal jugular vein, and spinal accessory nerve.
Imagining these three structures in this manner and dissecting accordingly help the surgeon to identify the spinal accessory nerve with ease and without injuring it. I would like to name this point as “SMS hospital point” (after the institute where this innovative idea came up) and the sign as “upward pointing arrow” sign.
CONCLUSION
Although studies to prove that this technique is better than others have not been done, we find it easier to identify and preserve the nerve and would want others to try this innovative and simpler way and put it into their practice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Excision of cancer of the head and neck with special reference to the plan of dissection based on one hundred and thirty-two operations. JAMA. 1906;XLVII:1780.
- [Google Scholar]
- Functional neck dissection: A description of operative technique. Arch Otolaryngol Head Neck Surg. 1980;106:524-7.
- [Google Scholar]
- Anatomic landmarks for localization of the spinal accessory nerve. Clin Anat. 2009;22:471-5.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic relationship between the spinal accessory nerve and internal jugular vein in the upper neck. Otolaryngol Head Neck Surg. 2010;143:239-41.
- [CrossRef] [PubMed] [Google Scholar]
- A technique to identify and preserve the spinal accessory nerve during neck dissection. J Laryngol Otol. 2006;120:494-6.
- [CrossRef] [PubMed] [Google Scholar]







