Translate this page into:
Malignant intracranial hemangiopericytoma in a 22-year-old male with head injury and implications
Address for correspondence: Dr. Mukesh Sharma, Department of Radiotherapy, Regional Cancer Centre, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India. muk00008@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a case of intracranial hemangiopericytoma of a young male of 22 years who presented with neurological signs of impaired memory, left hemiparesis, headache, and two episodes of focal seizures. A significant history of head trauma 9 years back was given. A space-occupying lesion was identified in the bilateral frontoparietal region. The surgical intervention involved bilateral frontoparietal craniotomy and Simpson Grade II excision of tumor. Postoperative conformal radiotherapy was administered. A marked neurological improvement was subsequently observed. Peak incidence of this disease is in the fourth or fifth decade. However, our case is an exception presenting at an age of 22 years. Associated history of head trauma has only been infrequently reported in the past.
Keywords
Hemangiopericytoma
trauma
young adult
Introduction
Initially described in 1942, hemangiopericytoma (HPC) is an uncommon malignancy. Arising from the Zimmerman pericytes and postcapillary venules (found in practically all types of tissue), it is not surprising that HPCs have been reported in many areas of the body.
Central nervous system (CNS) HPCs are uncommon. Intracranial HPCs constitute 1% of all intracranial tumors.1 No consistent risk factors have been identified. Surgery followed by adjuvant radiotherapy is the most common treatment regimen. Here, we report a case of intracranial HPC of a young male of 22 years with a significant history of head trauma 9 years back. This is a rare presentation in young adult age group. Furthermore, the relationship of intracranial HPC with head trauma has only been infrequently reported.
Case Report
A 22-year-old male presented to our outpatient department with complaints of left hemiparesis and two episodes of focal seizures in the left hand for the last 1 month, headache and vomiting for 15 days. There was no history of loss of consciousness, speech abnormalities, or urinary disturbances.
The history was noncontributory except an episode of hospitalization after an accident 9 years back. Records revealed that he had sustained a lacerated head injury and had been unconscious for an hour after injury. After a week of conservative management, he had been discharged.
On clinical examination, he was found to be fully conscious and well oriented. The power of left limbs was 0/5, all reflexes were absent bilaterally, and bilateral plantars were mute. There was sensory deficit in the left limbs. On examination, he had markedly deteriorated vision in both the eyes and there was gross papilledema and an old healed scar on the left temporoparietal region.
Contrast-enhanced magnetic resonance imaging (MRI) revealed a large lobulated heterogeneous solid cystic soft tissue mass lesion in the bilateral high frontoparietal lobe, measuring 70 mm × 67 mm × 65 mm with cystic areas, extensive vascularity, adjacent white matter edema, compressing adjacent parenchyma and bilateral lateral ventricles, midline shift to the right of 12 mm. It was isointense on T1- and T2-weighted which showed no diffusion restriction Figure 1a and b.
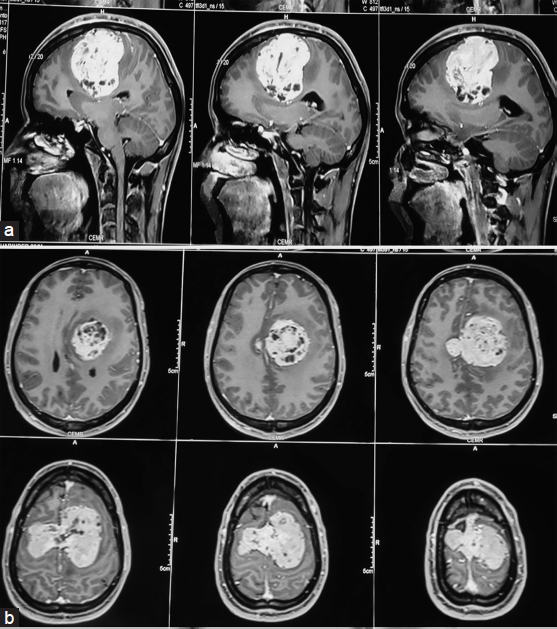
- (a) Preoperative T1-weighted image is showing postcontrast enhancement of an extra-axial mass in frontoparietal lobe: Saggital section. (b) Preoperative T1-weighted image showing postcontrast enhancement of an extra-axial mass in frontoparietal lobe: Axial section
The patient underwent bilateral frontoparietal craniotomy and Simpson Grade 2 excision of tumor in the department of neurosurgery.
Peroperatively, tumor on the surface was breaching dura, tumor was pinkish, gray, vascular, suckable, with some necrotic areas. Tumor was found attached to dura. Gross total excision was done. Following surgery, there was a drastic improvement in the symptoms of patients. Power in limbs improved to normal in the postoperative period.
Microscopy showed a highly cellular tumor with staghorn vascular pattern. The individual tumor cells were oval to elongated showing mild nuclear pleomorphism with conspicuous nucleoli having scant to moderate eosinophilic cytoplasm Figure 2. Peripheral rim of the brain tissues had shown focal invasion by the tumor. Two to three mitoses per high power field were seen Figure 3. There was no necrosis or endovascular proliferation. Thus, features were suggestive of HPC-Grade II (WHO 2007). Immunohistochemistry was positive for CD 34 and BCL2 while epithelial membrane antigen was negative.
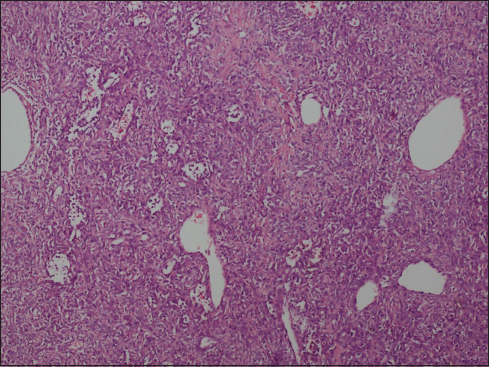
- Low power photomicrograph showing moderately cellular tumor with many hemangiopericytomas and branching vascular channels (H and E, ×2)
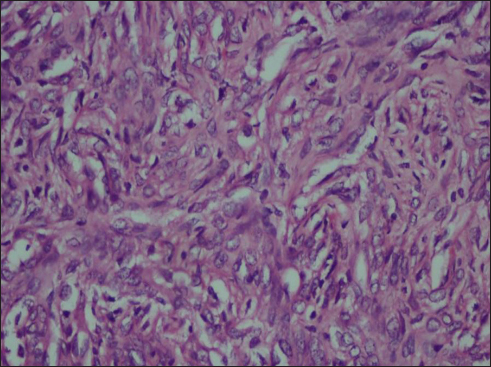
- Tumor cells seen as oval to spindle shaped cells with monomorphic nuclei (H and E, ×20)
Postoperative MRI of the brain was depicting areas of gliosis and subacute hemorrhage in frontoparietal lobe with minimal extra-axial subacute hematoma bilateral frontal regions with dural enhancement (postoperative status). No definite nodular enhancing lesion was seen.
The patient was subsequently given conformal radiotherapy delivered at a dose of 60 Gy in 30 fractions over 6 weeks. At present, our patient has completed 9 months of follow-up. He is asymptomatic with normal neurological examination at each follow-up. However, as disease recurrence and distant metastases can take years to develop, we need a prolonged patient follow-up to observe long-term outcome of HPC in young patients.
Discussion
HPCs have received prominence in the last two decades. They had initially been included in a specific group of CNS tumors (WHO classification 1993) and subsequently as a group by itself (WHO classification 1997 and 2000). HPC closely mimics meningiomas in clinical and radiological features; thus, the detailed histopathological review is the only means of its accurate diagnosis. The usual presentation of intracranial hemangiopericytoma is in the fourth to fifth decades of life.2
Adequate surgical resection, when feasible, is the first choice of treatment in all the cases of HPC. In case of benign HPC, complete surgical resection is sufficient. On the other hand, in case of malignant HPC, postoperative radiotherapy is strongly recommended even after an apparently complete tumor resection and must be given after subtotal tumor resections. However, the role of adjuvant chemotherapy is less clear.
A recent review identified 523 patients of intracranial HPCs, with a mean age of 44 years. The age of presentation of adult intracranial HPC has been variously reported from 34 to 44 years.3
Our report shows that malignant HPC can also be seen in a young adult in this site, and in such a case, diligent surgery followed by radiosurgical approach may prove fruitful. The role of chemotherapy in this setting is still unclear. Moreover, a lifelong vigilant clinical and radiological follow-up is mandatory due to very high malignant and metastatic potential of this tumor, years after the initial diagnosis.
Another point of concern is the associated history of trauma. The past inflammatory responses due to injury have been a cause of concern in many neoplasms. Although trauma has been implicated in brain tumors, especially meningioma,4 it has not been associated with HPC. A case series of two cases of HPC after a prior history of head trauma has been reported earlier.5 It needs to be emphasized that such a history is also important in patients suffering from this rare malignancy whenever such cases are reported.
Conclusion
Intracranial HPCs are rare neoplasms. Although the age of onset is generally fourth to fifth decades of life, they may even arise in young adults. A history of traumatic brain injury has been infrequently reported in intracranial HPCs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Meningeal hemangiopericytoma: Histopathological features, treatment, and long-term follow-up of 44 cases. Neurosurgery. 1989;25:514-22.
- [Google Scholar]
- Four cases of meningeal hemangiopericytoma treated with surgery and radiotherapy. Jpn J Clin Oncol. 2001;31:548-52.
- [Google Scholar]
- CNS Hemangiopericytoma: A Systematic Review of 523 Patients. Am J Clin Oncol. doi: 10.1097/COC.0000000000000146. [Epub]
- [Google Scholar]
- History of head trauma and risk of intracranial meningioma: Population-based case-control study. Neurology. 2002;58:1849-52.
- [Google Scholar]
- Hemangiopericytoma of brain in children after head trauma: Report of two cases. Clin Neurol Neurosurg. 1997;99:239.
- [Google Scholar]







