Translate this page into:
Locally Advanced Carcinoma of Maxillary Sinus with Orbital Involvement
Address for correspondence Gaurav Mittal, BDS, MDS, Department of Oral and Maxillofacial Surgery, Institute of Dental Studies and Technologies, Modinagar 201204, Uttar Pradesh, India. drgauravmittal@rediffmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Maxillary sinus carcinoma is a rare neoplasm, with incidence of 0.2 to 0.8% of all systemic malignancies. Patients are diagnosed in the advanced stage when there is orbital invasion with abnormal ocular signs and symptoms. The standard treatment of maxillary sinus carcinoma is en bloc radical maxillectomy along with orbital exenteration, followed by postoperative adjuvant therapy. Orbital exenteration is used when the malignancy extends to the orbit in case of squamous/basal cell carcinoma. The aim of the current review is to provide an insight into the management of advanced maxillary carcinoma with orbital involvement in a 42-year-old male.
Keywords
maxillary sinus carcinoma
en bloc radical maxillectomy
orbital exenteration
anterolateral thigh flap
adjuvant therapy
Introduction
Sinonasal malignancies involve maxillary, ethmoid, frontal, sphenoid and nasal cavities, of which maxillary antrum is 25 to 60% involved and sphenoid sinus is the least commonly involved. Sinonasal tumors constitute 0.2 to 0.8% of all systemic malignancies and 3 to 4% of all head and neck neoplasms. These are more commonly seen in elderly male patients. Local recurrences occur in approximately 25 to 35% of cases and distant metastases in 10% of cases. Sinonasal tumors have relatively poor prognosis, because they are diagnosed at advanced stages of disease due to relative paucity of pain in the early stages, with other clinical symptoms such as nasal congestion, rhinorrhea, epistaxis, and sinus pressure being treated for presumed infection.1,2
Squamous cell carcinoma is the commonest type of sinonasal malignancy that has been reported mostly in people who come into contact with hazardous material such as wood furniture, isopropyl alcohol, radium, nickel, chromium pigment, bantu snuff, thorotrast, mustard gas, polycyclic hydrocarbons, and cigarettes.3,4 Invasion of malignant paranasal and nasal sinus neoplasms into the surrounding structures and beyond the sinuses occur in 75% of cases and up to the orbit in 45% of cases. The orbital invasion may exhibit proptosis, facial or eye pain, visual loss, epiphora, globe displacement, limitation of extraocular movements, diplopia, inequality of palpebral fissures, conjunctival chemosis, a palpable mass within the orbit, bony erosion, fundus findings (optic disc edema), and dacryocystitis.5,6,7
The treatment of sinonasal malignancies requires a multidisciplinary team approach that includes radiologists, head and neck surgeons, neurosurgeons, oral prosthetics specialists, radiation oncologists, and medical oncologists. The treatment of choice for sinonasal malignancies includes combined surgery and irradiation and more concern about oncologic cure. The advent of new diagnostic technologies, advances in anesthesia, perioperative antibiotic prophylaxis, surgical reconstruction, and adjunctive therapy have prompted oncologic surgeons to become more conservative regarding the extirpation of functional structures.8
Case Report
A 42-year-old male presented with complaints of gradually increasing painless swelling over the left side of the face since 3 to 4 months with associated focal pain. Physical examination revealed thin built with no history of systemic illness. No history of trauma was present. On examination, there was a well-defined irregular fungating growth approximately 6 × 8 cm, involving left maxilla infiltrating into the left orbit, with displacement of left eyeball laterally and superiorly. On extraoral examination, the lesion extended from lateral border of nose to cheek bone transversely and vertically from nasolabial fold to supraorbital margin. Left eyeball was not seen due to growth. The surrounding area of lesion was glossy, red inflamed, and edematous (Fig. 1).

-
Fig.1 Preoperative extraoral image.
The inflamed lesion was tender on palpation. Mouth opening was normal. Left submandibular lymph nodes of 3 × 3 cm were palpable with stony hard consistency and fixed to the neighboring structures with clinical extra capsular extension. Level II and III nodes were also enlarged. Left-sided malar swelling and nasal block were present. Left hemipalate was involved with the tumor. There were no significant findings from other systemic examinations.
Contrast-enhanced CT of orbit and paranasal sinuses (PNS) was suggestive of a large, well-defined heterogeneously hyperdense solid exophytic mass lesion seen involved with left maxillary sinus and extensive destruction of its walls. The mass is seen extending into the left orbit and displacing the globe superolaterally with loss of fat plane (Fig. 2). Medially, the mass is seen involved with left osteomeatal complex, turbinates, ethmoid air cells, and lateral nasal wall and septum (Fig. 3).

-
Fig. 2 CECT PNS (contrast-enhanced computed tomography and paranasal sinuses): axial View depicting lesion extending into left orbit and displacing the globe superolaterally with loss of fat plane.

-
Fig. 3 CECT PNS (contrast-enhanced computed tomography and paranasal sinuses): corornal view showing the mass present medially involving left osteomeatal complex, turbinates, ethmoid air cells and lateral nasal wall and septum.
Routine investigation for preanesthetic clearance was carried out, and counseling of the patient in the presence of guardians was conducted, explaining the risks and benefits of surgery. Written informed consent for surgery and removal of one eye was obtained after counseling. Left radical Type IIIb maxillectomy, according to Cordeiro’s classification, with orbital exenteration, followed by left modified radical neck dissection type III, reconstruction with left anterolateral thigh flap and, finally, adjuvant therapy were planned.
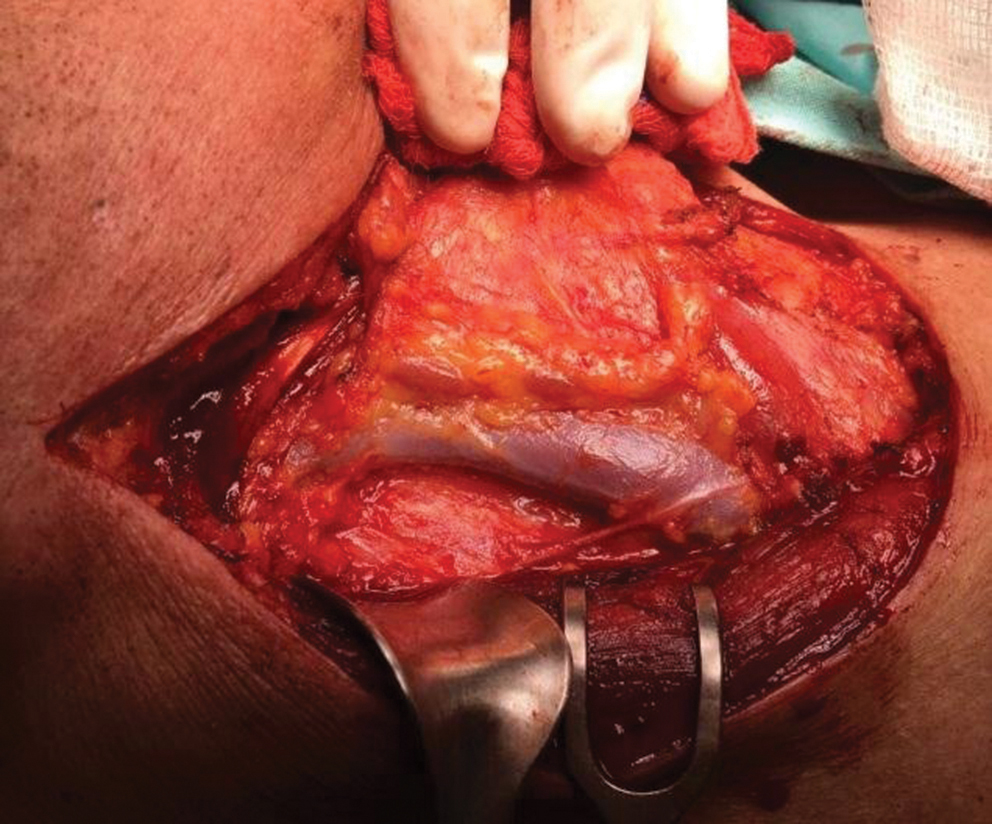
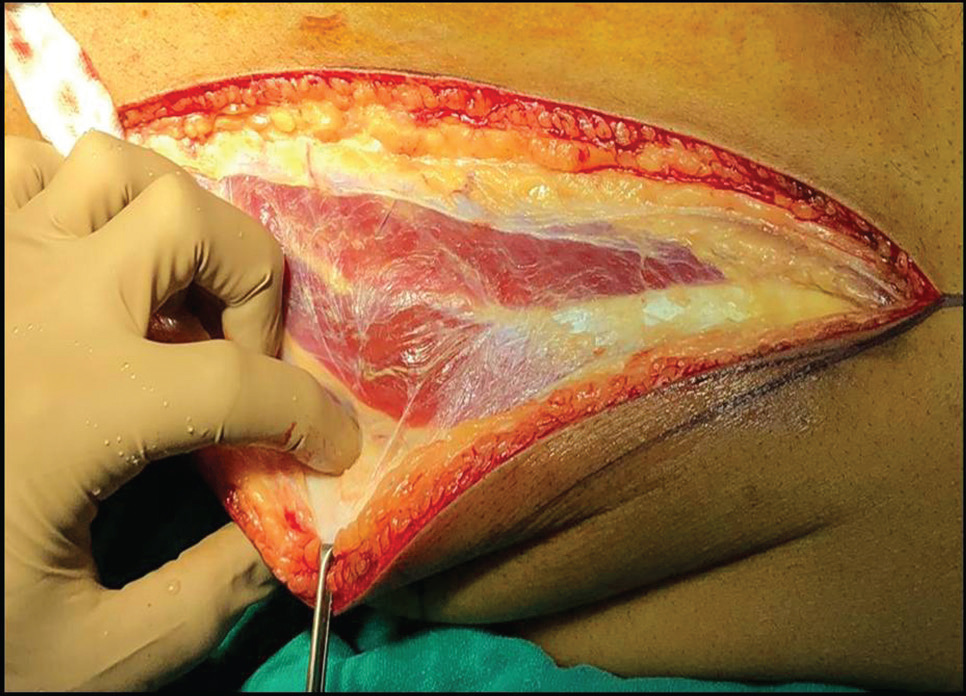
Tracheostomy was performed and general anesthesia was administered through the tracheal tube. The patient was positioned supine with head up, and parts were cleaned and draped. The Weber–Fergusson incision was made around the involved skin. The left cheek flap was raised and radical maxillectomy was performed, along with upper gingivobuccal sulcus and an buccal mucosa resection done as an en bloc specimen, by giving anterior cut through extraction socket of left upper central incisor, midline palate cut, posterior cut at pterygoids, superior cut at midline incorporating the left nasal bone, inferiorly midline cut along nasal floor incorporating the lateral nasal wall, sparing the left ala of nose, and lateral cut through lateral orbital rim and zygomatic arch. The orbital cut was placed along the medial orbital wall, incorporating the floor and orbital contents and laterally connected to the cut placed on the lateral orbital wall. The specimen was oriented and sent for frozen section (Fig. 4). Coronoidectomy was done for access. Hemostasis was achieved. Modified radical neck dissection (type III) was performed at an extended neck position turned toward right. The skin flap was elevated in subplatysmal plane (Fig. 5).

-
Fig. 4 Labeled excised specimen.
-
Fig. 5 Modified radical neck dissection type III.
After maxillectomy, the defect (Fig. 6) was closed by using anterolateral thigh flap with double paddle of 25 × 10 cm for intraoral reconstruction of hard palate and buccal mucosa, extraoral reconstruction of orbit, maxilla and zygoma, muscle to fill the cavity, and a portion of the flap turned into form the lateral wall of the nose. The left thigh was used as a donor site with three musculocutaneous perforators, including fascia and partial vastus lateralis muscle (Fig. 7). The donor site was closed primarily over room suction drain, and distal pulsation of femoral artery was confirmed. Anastomosis of facial artery was done by using 9–0 nylon, and that of common facial vein was done by 3–0 coupler. The flap was evaluated at the end of the procedure and found to be well-perfused (Figs. 8).

-
Fig. 6 Postoperative surgical defect.
-
Fig. 7 Harvesting of anterolateral thigh flap.

-
Fig. 8 (A, B) Postoperative extraoral view showing viable flap.
Discussion
Cancer of the maxillary sinus, a lethal neoplasm with an insidious onset, is most often diagnosed at an advanced stage of the disease, because it might be misdiagnosed with common sinus infection at the early stage of clinical symptoms. It is most commonly predilected in elder males. Clinical classification of the cancer is dependent on the location of antrum involvement as well as its size.9
Staging systems are used to define the extent of neoplastic disease and provide some basis to determine prognosis. The tumor, node, and metastases (TNM) system of classification of maxillary sinus cancers is based on an imaginary line, separating the maxillary antrum into anteroinferior and superoposterior compartments, as shown by Ohngren10 in 1933. Lederman11 drew two parallel lines through the antral floor of the maxillary sinus and across the antral roof, on coronal view, and divided into infrastructure, mesostructure, and suprastructure. Tumors extending into the suprastructure also often require an orbital exenteration. Sisson12 et al suggested inclusion of carcinoma of the antrum into the TNM classification. T1 tumors are confined to the mucosa, T2 lesions are associated with osseous erosion or destruction, and T3 and T4 tumors extend outside the sinonasal cavity into the masticator space, cheek, adjacent paranasal sinuses, orbital apex, base of skull, nasopharynx, or intracranially.13 Contrast-enhanced imaging is essential to assess the extent of local disease, and the presence of perineural spread and intracranial extension. Potential areas of tumor extension that must be assessed in all patients with sinonasal malignancies include intracranial spread (the anterior and middle cranial fossa), the palate, the orbits, the pterigopalatine fossa, and the skull base.14
Spreading of sinonasal malignancies usually takes place directly or by perineural extension. Prognosis and designing of the surgical management depend on superior and posterior boundaries of the maxillary sinuses. If there is posteriorly direct extension of tumor into the orbit, or spread to the intracranial compartment via the ethmoid air cells, then it is difficult to obtain tumor-free surgical margins. Medially, extension to the nasal cavity and inferiorly to the alveolus leads to less problematic en bloc resection.15 The lamina papyracea, lateral wall of the ethmoid air cells when violated, may result in intraorbital spread that requires orbital exenteration. Duke-Elder16 states that carcinoma of the maxillary sinus is the commonest malignant disease of any of the sinuses to invade the orbit. Iannetti17 et al identified three stages of orbital invasion: Grade I, erosion or destruction of the medial orbital wall; Grade II, extraconal invasion of the periorbital fat; Grade III, invasion of the medial rectus muscle, optic nerve, ocular bulb, or the skin overlying the eyelid. They propose that only grade III orbital invasion warrants orbital clearance or exenteration. Regional lymph node metastases from sinonasal malignancies are not so common, but when present, usually indicate tumor extension outside of the sinonasal cavity and poor prognosis. Lateral retropharyngeal nodes are primary nodal drainage site. Therefore, the upper internal jugular and submandibular nodes are the most common sites for nodal metastases. The above-mentioned case presenting with Grade III stage of orbital invasion presented with the following clinical symptoms: globe displacement, limitation of extraocular movements, inequality of palpebral fissures, and palpable mass overlapping the orbit. Left submandibular lymph nodes were palpable, and Level II and III nodes were also enlarged, with no significant indication of distant metastasis. In our case, TNM staging is cT3N3bM0.
We have performed combined treatment in cases of locally advanced maxillary sinus carcinoma which includes en bloc radical maxillectomy by making the Weber–Ferguson incision with orbital exenteration along with modified neck dissection and reconstruction of defect with flap, followed by radiotherapy. Cordeiro’s classification18 of maxillary defects provide an idea about extent of maxillectomy procedure. In the above-mentioned case, it was Type IIIb (total maxillectomy with orbital exenteration).
Ketcham et al19 suggested combined intracranial facial approach to overcome the difficulty in the complete extirpation of the cancer. Jesse20 suggested radical maxillary resection, followed by radiotherapy, permits definition of the extent of the tumor at the initial surgery for moderately advanced cancer in older people. Yasuo et al21 included chemotherapy in combination with radiation and surgery to overcome the limitation of oncologic excisional surgery. Som et al22 have suggested that orbital preservation is possible by preoperative radiation therapy. However, there is no significant improvement in survival rate by use of planned combination therapy, radiation therapy before or after surgery. Larson et al23 reported indications for orbital exenteration which included invasion of the periorbita, infraorbital nerve, posterior ethmoid sinuses, or orbital apex, and suggested that the survival of patients whose orbit was preserved was not different from those whose orbits were exenterated. In 1988, Perry9 et al reported their experience preserving the orbit, even when a sinonasal tract malignancy has invaded the periorbita (localized invasion), and concluded that preservation of the orbit in selected cases did not compromise the cure rate of these patients.
Conclusion
Carcinoma of the maxillary sinus presents the typical signs, symptoms, and course of the disease. CT and MR imaging play complementary roles in the assessment and staging of these malignancies by determining the presence or absence of extension of disease. Patient survival rate can be increased in patients of maxillary sinus carcinoma by way of a collaboration of oncologist and radio-oncologist. This association includes aggressive surgical therapy by performing en bloc radical maxillectomy with orbital exenteration accompanied by postoperative radiotherapy and chemotherapy.
Conflict of Interest
None declared.
References
- Diseases of the nose, paranasal sinuses, and nasopharynx In: Barnes L, ed. Surgical Pathology of the Head and Neck. New York: Marcel Dekker; 1985. p. :403-51.
- [Google Scholar]
- Carcinoma of the antrum: a clinical and histopathologic study. Oral Surg Oral Med Oral Pathol. 1960;13:269-281.
- [Google Scholar]
- Malignant tumors of the paranasal sinuses: radiologic, clinical, and histopathologic evaluation of 200 cases. Head Neck Surg. 1984;6(03):761-776.
- [Google Scholar]
- Pathways of orbital extension of extraorbital neoplasms. J Comput Assist Tomogr. 1982;6(03):593-597.
- [Google Scholar]
- Orbital exenteration in surgery of malignant neoplasms of the paranasal sinuses. The value of preoperative computed tomography. Arch Otolaryngol Head Neck Surg. 1989;115(08):977-980.
- [Google Scholar]
- Management of the orbital contents in radical surgery for squamous cell carcinoma of the maxillary sinus. Chin Med J (Engl). 1995;108(02):123-125.
- [Google Scholar]
- Preservation of the eye in paranasal sinus cancer surgery. Arch Otolaryngol Head Neck Surg. 1988;114(06):632-634.
- [Google Scholar]
- Tumours of the upper jaw: natural history and treatment. J Laryngol Otol. 1970;84(04):369-401.
- [Google Scholar]
- Cancer of the maxillary sinus: clinical classification and management. Ann Otol Rhinol Laryngol. 1963;72:1050-1059.
- [Google Scholar]
- Cancer of the nasal cavity and paranasal sinuses: a new staging system. Int J Oral Maxillofac Surg. 1996;25(01):34-39.
- [Google Scholar]
- Sinonasal undifferentiated carcinoma: CT and MR imaging of an uncommon neoplasm of the nasal cavity. Radiology. 1997;202(02):477-480.
- [Google Scholar]
- CT of perineural tumor extension: pterygopalatine fossa. AJNR Am J Neuroradiol. 1984;5:731-737.
- [Google Scholar]
- A classification system and algorithm for reconstruction of maxillectomy and midfacial defects. Plast Reconstr Surg. 2000;105(07):2331-2346, discussion 2347–2348.
- [Google Scholar]
- A combined intracranial facial approach to the paranasal sinuses. Am J Surg. 1963;106:698-703.
- [Google Scholar]
- Paranasal sinuses and nasal cavity In: MacComb W S, Fletcher G S, eds. Cancer of Head and Neck. Baltimore: Williams & Wilkins; 1967. p. :329-356.
- [Google Scholar]
- Combined surgery, radiotherapy, and regional chemotherapy in carcinoma of the paranasal sinuses. Cancer. 1970;25(03):571-579.
- [Google Scholar]
- Surgical management of carcinoma of the maxilla. Arch Otolaryngol. 1974;99(04):270-273.
- [Google Scholar]
- Preservation of the orbital contents in cancer of the maxillary sinus. Arch Otolaryngol. 1982;108(06):370-372.
- [Google Scholar]







