Translate this page into:
Indian data on response of positive pelvic lymph nodes in carcinoma cervix patients treated with simultaneous integrated boost using volumetric modulated arc radiation therapy
Corresponding author: Dr. Rashmi Shivananjappa, Department of Radiation oncology, Kidwai Memorial Institute of Oncology, Hombegowda Nagar, Bengaluru, India. drrashmishivananjappa@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Perumareddy V, Shivananjappa R, Geeta SN, Tiwari R. An Indian data on response of positive pelvic lymph nodes in carcinoma cervix patients treated with simultaneous integrated boost using volumetric modulated arc radiation therapy. Asian J Oncol, 2023;9:9.
Abstract
Objectives
The percentage of pelvic lymph node positivity in cervical cancer patients varies from 19% in early stages to 68% in advanced cases. Thirty three percent of patients will develop recurrence within 2 years following therapy and 5-year relative survival for patients with affected regional lymph nodes is 57%. Hence, pelvic lymph nodes need to be included in the definitive plan of radiation treatment for better disease control and longer survival. With conventional radiation therapy, dose escalation was not possible because of small bowel constraints. With higher conformity of intensity modulated radiotherapy technique (IMRT), doses to pelvic and abdominal organs can be minimized. The added advantage of simultaneous integrated boost (SIB) is that high dose per fraction is delivered to the gross disease and low dose to the microscopic disease, thereby reducing the total treatment time and improving the therapeutic ratio.
Material and Methods
Forty one patients presenting to the Department of Radiation Oncology, between January 2016 and June 2017, with newly biopsy proven carcinoma cervix Stage IB to IVA were enrolled in the study and all the investigations were performed. The radiation dose was delivered using volumetric modulated arc therapy plan to a dose of 5000 cGy in 25 fractions to the whole pelvis and 5500 cGy in 25 fractions at 220 cGy per fraction to the involved nodes using SIB along with weekly cisplatin at 40 mg/m2. After completion of external beam radiation, all the patients received three fractions of brachytherapy to a total dose of 21 Gy. Acute toxicities were assessed using RTOG criteria. At 3 months after completion of treatment, all the patients had been followed up with DW MRI of abdomen and pelvis to assess the response.
Results
Of the 41 carcinoma cervix patients with significantly positive lymph nodes treated with SIB VMAT, 9.8% of the patients (4 patients) had residual nodal disease, 87.8% of the patients (36 patients) had complete response, 19.5% (8 patients) had residual disease of primary disease, and 78% (32 patients) had complete response at 3 months after completion of treatment with only Grade – I and Grade – II toxicities.
Conclusion
Treatment with SIB VMAT in carcinoma cervix patients with significant pelvic lymph nodes shows very good response with acceptable acute toxicities. But longer follow-up period is required to see if this response translates into better DFS and OS.
Keywords
Carcinoma Cervix
Brachytherapy
Positive Pelvic Lymph Nodes
Simultaneous Integrated Boost
Volumetric Modulated Arc Radiation Therapy
INTRODUCTION
Cervical cancer is the commonest cancer cause of death among women in developing countries.[1] India has a population of 432.2 million women aged 15 years and older who are at risk of developing cancer. In India, 122,844 women are diagnosed with cervical cancer every year and 67,477 die from the disease. It is the second most common cancer in women aged 15–44 years. India has the highest incidence of cervical cancer in South Asia, compared to Bangladesh, Sri Lanka, and Iran.[2] Mortality due to cervical cancer is also an indicator of health inequities, as 86% of all deaths due to cervical cancer are in developing, low- and middle-income countries.[3–6] Hence, it is imperative that we deliver the best treatment, which is going to have the maximum effect on local control, while having as little toxicities as possible.
Brachytherapy (BT) plays a major role in the treatment of patients with cervical cancer from stage I to IV. The rapid dose fall-off allows a very high dose to the central pelvis, while relatively sparing organs at risk. Concomitant chemoradiation followed by BT represents the standard of care in patients with tumors larger than 4 cm, i.e., from stage IB2 to stage IVA.[7] For stage IB1, BT is a treatment option either as a part of radical external beam RT, or as a preoperative BT in combination with colpohysterectomy and lymphadenectomy.[8]
MATERIAL AND METHODS
This prospective single-arm study included 41 patients, recruited from our department of radiation oncology, during the period of January 2016 to June 2017 with newly biopsy proven carcinoma cervix Stage IB2 to IVA. Complete physical examination with complete blood count, renal function test, liver function test, serum electrolytes, viral markers (HIV/HBSAg), biopsy from the primary site, DW-MRI of abdomen and pelvis or PET-CT scan, 2D Echo, and chest X-ray were done for all eligible patients. Informed written consent was taken from all the patients. Patients between the age of 20 and 70 years with biopsy proven FIGO stage IB1 to IVA cervical cancer patients with either PET CT or MRI DWI positive pelvic lymph nodes were included in the study. Patients with positive paraaortic lymph nodes, distant metastatic disease, previous pelvic radiation, and recurrent cervical cancer cases were excluded from the study.
Radiotherapy: All the patients underwent CT simulation after preparation of bowel on the previous night of the scan and bladder protocol was followed. The area to be scanned was localized and axial scans were acquired at 2.5-mm-slice thicknesses. For external beam radiation (EBRT) planning and treatment, MRI scan was used for target delineation as it has better soft tissue delineation. T2W images were used for the delineation of the tumor and normal structures, whereas for positive lymphnodes ADC images in DWI sequence are used which are fused with our simulation CT scan. CTV delineation was done as per Taylor et al. guidelines. PTV 50 Gy: CTV-N and CTV-T with 5 mm margin. PTV 55Gy: GTV-N with 5 mm margin. Contouring of normal surrounding critical structures such as rectum, bladder, right and left femoral heads, and bowel bag were done.
Dose Prescription: 5000 cGy in 25 fractions to the whole pelvis with 200 cGy per fraction and 5500 cGy in 25 fractions to the significant lymph nodes with 220 cGy per fraction five fractions per week, as shown in Figure 1.
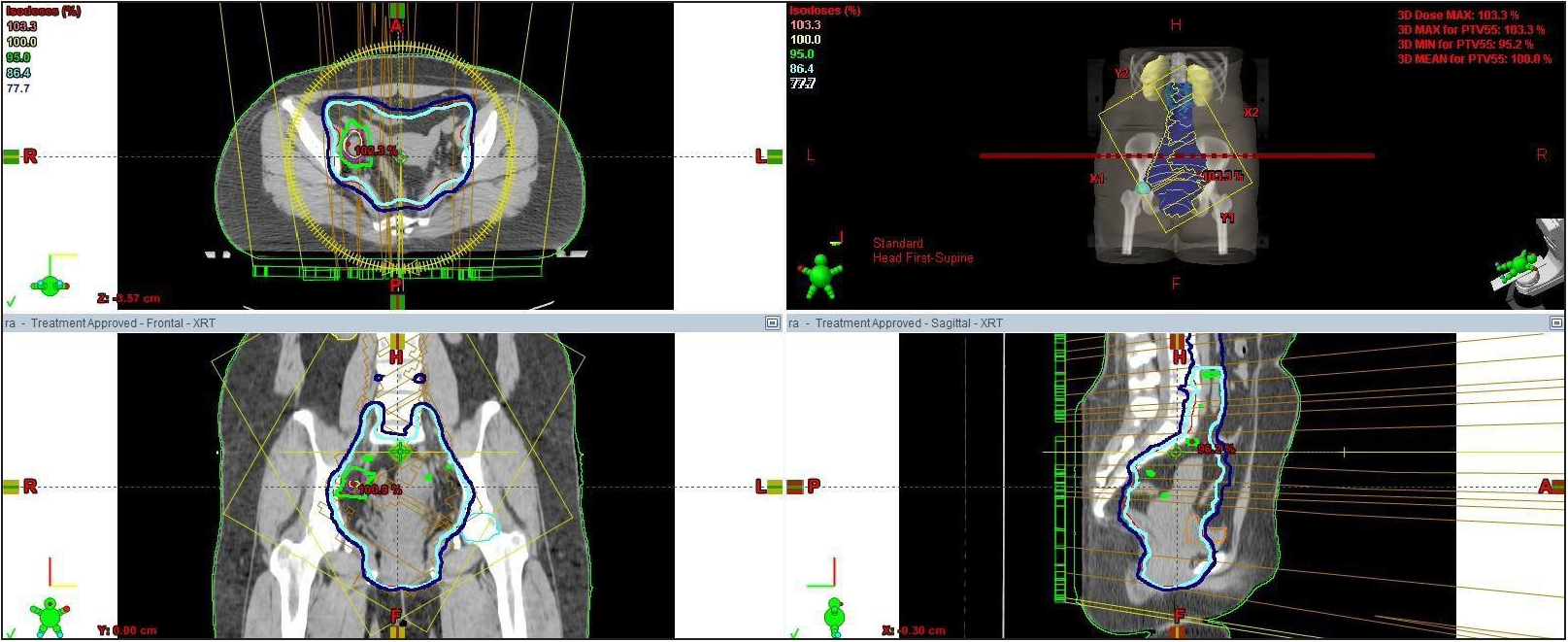
- EBRT planning using SIB VMAT.
Chemotherapy: Weekly Inj Cisplatin – 40 mg/m2 concurrently along with radiation was administered intravenously.
Brachytherapy: All patients were clinically assessed at 3 weeks of EBRT, and after completion of full course of EBRT. Patients were then assigned for BT. Treatment duration was kept to ≤8 weeks. Prescription dose of 700 cGy in three fractions is considered.
Follow-Up: All patients were assessed weekly during the treatment, every 3 months thereafter for 2 years. Toxicities were recorded according to common terminology criteria for adverse events (CTCAE) version 4.0.[9] All the patients underwent DWI-MRI imaging during follow-up to assess for the loco-regional response using response evaluation criteria in solid tumors (RECIST).[10]
Statistical Analysis: The sample size was estimated in consultation with a bio-statistician. The sample size given was 41 cases. This was estimated based on the study by Wakatsuki et al.[11]
RESULTS
Patients selected for the study aged from 28 to 76 years. Mean age of the patients was 50 years. Patients with stage – IB2 to stage – IVA were included in the study. All patients had ECOG status of either 0 or 1. All patients except one received treatment without any interruptions. One patient discontinued her treatment as she developed myocardial infarction. Hence, all the remaining 40 patients underwent BT after completion of concurrent chemo-radiation. Response assessment and toxicities are shown in Table 1–7, respectively.
Frequency
Percent
Valid percent
Cumulative percent
Residual
8
Valid
Disease
19.5
19.5
19.5
Complete
32
Response
78.0
78.0
97.6
Treatment discontinued
1
2.4
2.4
100.0
Total
41
100.0
100.0
Frequency
Percent
Valid percent
Cumulative percent
Valid
Residual disease
4
9.8
9.8
9.8
Complete response
36
87.8
87.8
97.6
Treatment discontinued
1
2.4
2.4
100.0
Total
41
100.0
100.0
Frequency
Percent
Valid percent
Cumulative percent
Valid
Residual disease
8
19.5
19.5
19.5
Complete response
32
78.0
78.0
97.6
Treatment discontinued
1
2.4
2.4
100.0
Total
41
100.0
100.0
Frequency
Percent
Valid percent
Cumulative percent
Valid
No Toxicity
35
85.4
85.4
85.4
Grade 1
4
9.8
9.8
95.1
Grade 2
2
4.9
4.9
100.0
Total
41
100.0
100.0
Frequency
Percent
Valid percent
Cumulative percent
Valid
No Toxicity
10
24.4
24.4
24.4
Grade 1
6
14.6
14.6
39.0
Grade 2
25
61.0
61.0
100.0
Total
41
100.0
100.0
Frequency
Percent
Valid percent
Cumulative percent
Valid
No Toxicity
23
56.1
56.1
56.1
Grade 1
5
12.2
12.2
68.3
Grade 2
13
31.7
31.7
100.0
Total
41
100.0
100.0
Frequency
Percent
Valid percent
Cumulative percent
Valid
No Toxicity
25
61.0
61.0
61.0
Grade 1
15
36.6
36.6
97.6
Grade 2
1
2.4
2.4
100.0
Total
41
100.0
100.0
RESPONSE ASSESSMENT
Response of the primary clinically after 6 weeks of radiation [ Table 1 ]: Out of the 41 patients studied, 8 patients (19.5%) had residual disease, 32 patients (78%) had complete response, and 1 patient (2.5%) discontinued treatment.
Response of the nodes on MRI after 3 months of treatment [ Table 2 ]: Out of the 41 patients studied, 4 patients (9.75%) had residual nodal disease, 36 patients (87.75%) had complete response in nodes, and 1 patient (2.5%) discontinued treatment.
Response of the primary on MRI after 3 months of treatment [ Table 3 ]: Out of the 41 patients studied, 8 patients (19.5%) had residual disease, 32 patients (78%) had complete response, and 1 patient (2.5%) discontinued treatment.
TOXICITIES
Skin toxicity [ Table 4 ]: Four patients (9.75%) developed grade I toxicity, two patients (4.8%) developed grade II skin toxicity. Rest of the patients had no skin toxicity. There were no grade III, IV, or V toxicities.
Upper Gastrointestinal toxicity [ Table 5 ]: Six patients (14.6%) had grade I toxicity, Twenty five patients (60.9%) had grade II toxicity. Rest of the ten patients had no upper gastrointestinal toxicity.
Lower Gastrointestinal toxicity [ Table 6 ]: Five patients (12%) had grade I toxicity, thirteen patients (31%) had grade II toxicity. Rest of the patients had no lower gastrointestinal toxicity. Genitourinary toxicity [Table 7]: Fifteen patients (36.5%) had grade I toxicity, one patient (2.5%) had grade II toxicity. Rest of the patients had no genitourinary toxicity.
DISCUSSION
A total of 41 patients were included in the study. Significant lymph nodes with ADC uptake were noted and delineated in all the patients. Volumetric modulated Arc radiotherapy with simultaneous integrated boost (SIB VMAT) is being used recently by many centers. With SIB VMAT, we can achieve improved dose distributions by allowing more conformal dose to the involved nodes and the adjacent organs are increasingly spared from risk. Also, VMAT-SIB regimens may result in improved local control due to the shortened overall treatment time. The total duration of the treatment does not exceed 7–8 weeks; hence, the overall treatment time remains the same without compromising the loco-regional control.
In a study by Nikola Chioric et al.,[12] 10 patients with 18FDG-PET/CT positive lymph nodes underwent chemoradiation with IMRT and SIB. A dose of 62Gy in 2Gy per fraction was delivered to FDG-PET/CT positive lymph nodes and finally a high-dose rate BT boost (15–18Gy) was administered to the primary tumor. These patients were evaluated for loco-regional control, acute and early late toxicities for a median follow up of 20 months. Acute and late grade-3 toxicity was observed in one patient. Three patients developed recurrence. Overall, the study showed SIB to be an effective therapy with acceptable toxicity and might be useful in the treatment of patients with locally advanced cervical cancer.
The limitations of this study were small sample size and the retrospective nature of the study, but the present study contributes to the notion that the application of a high dose of radiation in the region of 18FDG-PET\CT positive LNs by means of IMRT and SIB is feasible, with an acceptable profile of unwanted events and good loco-regional control.
In another study done by Ariga et al.,[13] the study population comprised 174 patients, who were treated with definitive radiotherapy (RT) or concurrent chemoradiotherapy (CCRT) and high-dose-rate intracavitary brachytherapy (HDR-ICBT). Patients with positive paraaortic or common iliac nodes were ineligible for the study. Fifty-seven patients (33%) had clinically positive pelvic nodes. Fifty-two of 57 patients (91%) with positive nodes were treated with boost EBRT (6–10 Gy in three to five fractions). The median prescribed dose of EBRT for nodes was 56 Gy. The median follow-up time for all patients was 66 months. The 5-year overall survival rate, disease-free survival rate, and pelvic control rate for patients with positive and negative nodes were 73% and 92% (P = 0.001), 58% and 84% (P < 0.001), and 83% and 92% (P = 0.082), respectively. Five of the 57 node-positive patients (9%) developed pelvic node recurrences. No significant difference was observed with respect to the incidence or severity of late complications by the application of boost EBRT.
Our study has shown that out of 41 carcinoma cervix patients with significantly positive lymph nodes treated with SIB VMAT, 87.8% of the patients (36 patients) had complete response and 9.8% of the patients (4 patients) had residual nodal disease, 78% (32 patients) had complete response at 3 months after completion of treatment, and 19.5% (8 patients) had residual disease in the primary and with acceptable Grade – I and Grade – II toxicities. There were no Grade – III or Grade – IV toxicities in any of the patients studied. With a total frequency of 41, the valid frequency for the patients without any interruptions was 97.6%, and the valid frequency for the patients with interruptions was 2.4%.
All the patients had undergone DWI-MRI pre- and post-treatment for the determination of lymph nodes due to financial constraints and hence PET-CT was not used in the study. Lymph node groups involved in the study were common iliac, external iliac, internal iliac, obturator, and inguinal lymph nodes in cases where lower third of vagina was involved. A total of 66 significant lymph nodes were included in the study and the most common group of lymph nodes which were positive are external iliac and internal iliac group of lymph nodes which were followed by obturator and common iliac group of lymph nodes.
CONCLUSION
The present prospective nonrandomized study was performed for patients treated with SIB using volumetric modulated arc radiation therapy in carcinoma cervix staged IB2 to IVA. EBRT with SIB VMAT along with HDR BT and concurrent cisplatin appears to be a safe and effective treatment modality for pelvic lymph node metastatic uterine cervical carcinoma providing a high rate of regional response with acceptable toxicity. Hence, we suggest using the SIB VMAT technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- ICO Information Centre on HPV and cancer. Human papillomavirus and related diseases in India (Summary Report 2014-08-22);2014.
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10 Lyon, France: International Agency for Research on Cancer; 2010. [Accessed May 1 2012]. Available at: http://globocan.iarc.fr.
- Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011;22:2675-86.
- [CrossRef] [PubMed] [Google Scholar]
- Global cancer statistics. 2. Vol. 61. CA: A Cancer Journal for Clinicians 2011:69-90. Epub 2011 Feb 4. Erratum in: CA: A Cancer Journal for Clinicians. 2011;61:134
- [CrossRef] [PubMed] [Google Scholar]
- Management for locally advanced cervical cancer: new trends and controversial issues. Radiat Oncol J. 2018;36:254-64.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Radiochimiothérapie concomitante dans les cancers du col utérin: modifications des standards. Cancer Radiother. 2000;4:134s-140.
- [PubMed] [Google Scholar]
- National Cancer Institute. National Institutes of Health, Common Terminology Criteria for Adverse Events (CTCAE), Version 4.03. 2010 http://evs.nci.nih.gov/ftp1/CTCAE/About.html.
- Eur J Cancer. 2009;45:228-47.
- [CrossRef] [PubMed]
- Impact of boost irradiation on pelvic lymph node control in patients with cervical cancer. J Radiat Res. 2013;55:139-45.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- IMRT with 18FDG-PET/CT based simultaneous intergrated boost for treatment of nodal positive cervical cancer. Radiat Oncol. 2014;9:83.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- External beam boost irradiation for clinically positive pelvic nodes in patients with uterine cervical cancer. J Radiat Res. 2013;54:690-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







