Translate this page into:
Gastrointestinal stromal tumor and extragastrointestinal stromal tumor: Rare pattern of recurrence of disease
Address for correspondence: Dr. Amitabh Ray, Apollo Gleneagles Hospital, 58, Canal Road, Kadapara, Kankurgachi, Kolkata - 700 054, West Bengal, India. dramitabhray@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
GIST and EGIST are known to be distinct clinico-pathological entities. The occurrence of both in the same patient as a pattern of recurrence is extremely rare. We report one such case which was managed successfully due to high index of suspicion and interdisciplinary co-ordination.
Keywords
Extragastrointestinal stromal tumor
gastrointestinal stromal tumor
recurrent GIST
Introduction
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal neoplasm of the gastrointestinal (GI) tract, driven by oncogenic activation of KIT or platelet-derived growth factor receptor α.1,2 Hitherto, most GI mesenchymal neoplasms were thought to be smooth muscle derivatives and were thus classified, but identification of KIT - a receptor tyrosine kinase protein in this tumor necessitated reclassification. GISTs are consequently thought to arise from interstitial cells of Cajal or their precursor spindle cells that are equally known to express KIT.2
GISTs occur mainly in adult population, about 60% of which are located in the stomach and very rarely in children (<1% of reported cases).3 Small intestinal GISTs are said to account for about 30% of all GISTs with specified location and jejunum is more frequently involved than the ileum.3,4 GISTs can also develop outside the intestinal tract in the omentum, mesentery, uterus, and the retroperitoneum. They are called extra-GISTs (EGISTs). Approximately, 80% of EGISTs are located in the omentum or mesentery, and the remainder develop in the retroperitoneum.
The occurrence of EGIST is extremely rare, and little is known about their actual origin. Occurrence of GIST following EGIST is even more uncommon. We report the successful management of one such patient in this case report.
Case Report
A 69-year-old man with diabetes and hypertension presented in May 2011 with 2 months history of abdominal pains, vomiting, and general body weakness to the gastroenterology outpatient of Apollo Gleneagles Hospital, Kolkata. Important clinical finding on examination was a huge abdominal mass that measured 18 cm × 16 cm in dimension extending from the epigastrum to the lower abdomen. Abdominal ultrasound was suggestive of a retroperitoneal tumor. Contrast enhanced computed tomography scan of the whole abdomen revealed a large tumor arising from retroperitonem compressing left kidney Figure 1. Exploratory laparotomy revealed a retroperitoneal reniform mass, measuring 20 cm × 15 cm × 10 cm in close relation to the left kidney. It was surgically removed with tumor free margins Figure 1. Microscopy revealed spindle shaped cells with elongated nuclei and fibrillary cytoplasm. Mitotic count was rate ≤5 per 50 high-power fields (HPFs). Histopathology and immunohistochemistry (IHC) confirmed c-kit positive GIST. The patient was started on adjuvant treatment with imatinib mesylate (IM) 400 mg OD for 1 year as per prevalent recommendations5 and in view of old age.
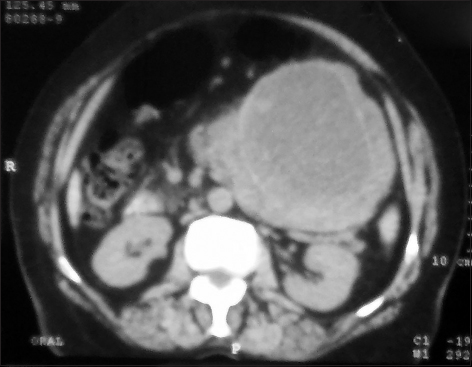
- Retroperitoneal reniform mass
The patient presented again in March 2014 with features of subacute intestinal obstruction and pain right iliac fossa. Clinicoradiological examination revealed right sided abdominal tumor suspicious of recurrent GIST Figure 2. Exploratory laparotomy revealed a jejunal mass that measured 15 cm × 10 cm × 6 cm. Histopathology and IHC were confirmatory for recurrent GIST. The patient was subsequently started on dose escalated IM 600 mg/day. He is on regular follow-up without evidence of active disease.
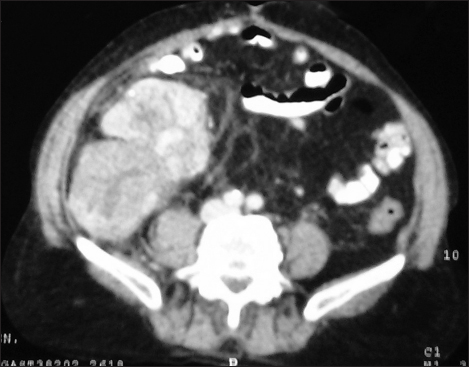
- Recurrent gastrointestinal stromal tumor
Discussion
The annual incidence of GISTs from a population-based study conducted in Western Sweden was found to be 14.5 cases per million.6 In the AFIP study of 906 stromal tumors involving jejunum or ileum, jejunal location tends to be more common by a factor of 1.6:1. There is slight male predominance and the median age of 59 years was reported.4 IHC KIT positivity is a defining feature of GISTs and virtually all small intestinal GISTs (>98%) are KIT positive.4
Tumor size is an important prognostic factor that independently could influence recurrence/metastasis.7 Based on a long-term follow-up studies on GISTs, 52% of patients with jejunal and ileal GISTs with tumor size >10 cm and mitotic rate ≤5 per 50 HPFs tend to have progressive disease during follow-up.4
Histologically, there are three types of GISTs: Spindle celled (70%), epithelioid (20%) and mixed. The presence of the epithelioid pattern is significantly linked to malignant transformation.4 The presence of extracellular collagen fibers referred to as skenoid fibers confer a favorable prognostic feature and is commonly seen in nonmalignant cases.8 Mitotic count is another important prognostic parameter, tumors with mitotic rate ≤5 per 50 HPFs have comparatively better prognosis compared to those with mitotic rate >5 per 50 HPFs when other factors are constant.3,7 The mitotic count in the case presented is low, ≤5 per 50 HPFs, and this probably had a positive influence on the progression of the disease in this case.
IHC staining confirming GISTs is a prerequisite for diagnosis. The panel of stains commonly employed includes KIT, CD34, smooth muscle actin (SMA), desmin, S100 DOG 1 and protein kinase C theta.9 Although KIT was positive in this case, and it is a major defining feature for GIST, it is no longer considered an absolute requirement. CD34, which was negative in this case, is reported to be positive in about 50% of small intestinal GISTs but it has little prognostic value. SMA is positive in about 35% of small intestinal GISTs and showed an inverse pattern in the frequency of expression as compared with CD34. Desmin and S100 are very rarely encountered in small intestinal GISTs. Protein kinase C theta is positive in a high percentage of GISTs, but the staining pattern is less distinctive and weaker compared to KIT positivity.9
Targeted treatment with KIT and other receptor tyrosine kinase inhibitors such as IM in unresectable, recurrent and metastatic GISTs have considerably improved survival and disease-free interval in large number of patients.10
EGISTs are mesenchymal tumors that may originate in sites outside the GI tract with clinico-pathological and molecular profiles similar to GISTs. The occurrence of EGIST is extremely rare and little is known about their actual origin. The usual pathogenesis is a gain of function mutations in the c-KIT gene that results in overexpression of the KIT receptor also called CD117 or stem cell factor receptor. As seen in this patient they manifest through bulky masses and need aggressive surgical intervention. Adjuvant imatinib is recommended, and a strict follow-up is necessary due to high recurrence rates. The majority of EGISTs are found to be either GISTs with extensive extramural growth resulting in loss of contact to the external muscle coat of the gut or as a metastasis from an inoperable GIST or from a previously resected deceptively benign tumor. Thus, a great percentage of EGISTs appeared to be due to metastasis from a primary GIST.11 However in this case the GIST presented itself almost 3 years after diagnosis of primary EGIST supporting an independent origin for the two diseases. To the best of our knowledge, this is the first case in the literature with such an unusual presentation.
Conclusion
Treatment of GIST with IM is a success story in modern oncology. However, a high index of suspicion should be kept for disease recurrence either in the GI or extra-GI location. EGIST and GIST very rarely present in the same patient as in this case. Paradigm shifts have happened in the way we deal with advanced stage primary and recurrent solid tumors, and this case serves as a good example of this fact.
Financial support and sponsorship
Nil.
Acknowledgement
Apollo Gleneagles Hospital, Kolkata, West Bengal, India.
Conflicts of interest
There are no conflicts of interest.
References
- Clinicopathologic profile of gastrointestinal stromal tumors (GISTs) with primary KIT exon 13 or exon 17 mutations: A multicenter study on 54 cases. Mod Pathol. 2008;21:476-84. et al.
- [Google Scholar]
- Gastrointestinal stromal tumors (GISTs): Definition, occurrence, pathology, differential diagnosis and molecular genetics. Pol J Pathol. 2003;54:3-24.
- [Google Scholar]
- Gastrointestinal stromal tumors: Pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23:70-83.
- [Google Scholar]
- Gastrointestinal stromal tumors of the jejunum and ileum: A clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol. 2006;30:477-89.
- [Google Scholar]
- Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: A randomised, double-blind, placebo-controlled trial. Lancet. 2009;373:1097-104. et al.
- [Google Scholar]
- Gastrointestinal stromal tumors: The incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era – A population-based study in western Sweden. Cancer. 2005;103:821-9. et al.
- [Google Scholar]
- Gastrointestinal stromal tumours (GISTs): A clinicopathological and molecular study of 66 cases. Pathology. 2005;37:22-31. et al.
- [Google Scholar]
- Small intestinal stromal tumors with skeinoid fibers. Clinicopathological, immunohistochemical, and ultrastructural investigationsAm J Surg Pathol. 1992;16:145-55.
- [Google Scholar]
- PKC theta, a novel immunohistochemical marker for gastrointestinal stromal tumors (GIST), especially useful for identifying KIT-negative tumors. Pathol Int. 2005;55:106-12.
- [Google Scholar]
- Gastrointestinal stromal tumor (GIST) recurrence following surgery: Review of the clinical utility of imatinib treatment. Ther Clin Risk Manag. 2010;6:453-8. et al.
- [Google Scholar]
- Extragastrointestinal stromal tumor (EGIST) in the abdominal wall: Case report and literature review. Int J Surg Case Rep. 2011;2:253-5.
- [Google Scholar]







