Translate this page into:
Clinicoepidemiological profile of hematological malignancies in pediatric age group in Ahmedabad
Address for correspondence: Dr. Mayur J. Kokani, Department of Pathology, GMERS Medical College, Valsad, Ahmedabad, Gujarat, India. rockki1234@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background: This hematological malignancy comprises a major health problem in the society due to its high mortality and morbidity. There is a need for the accurate estimation of incidence and prevalence of acute lymphocytic leukemia (ALL), and other hematological malignancies in India to estimate the true disease burden and its impact on the population which may help in formulating the guideline which helps in better risk stratification and treatment. Unfortunately, there is a real paucity if epidemiologic data on pediatric cancers in India and particularly in several parts of Gujarat.
Objectives: To find out the prevalence and other epidemiological distribution of hematological malignancy in pediatric age group patients. Furthermore, it was objected to study hematological profile and bone marrow typing in pediatric patients with hematological malignancies.
Methodology: A prospective observational study carried out over 2½ years. Confirm cases of hematological malignancies were recruited from the pediatric outpatient and inpatient department. Data recorded in the preformed case record form include demographic data, data of clinical history and clinical examination, laboratory findings such as complete blood count, peripheral smear examinations, bone marrow examination for cellularity and differential count, and immunophenotyping. Fine needle aspiration cytology or biopsy of lymph node was done in suspected lymphoma patients.
Observations: ALL is the most common hematological malignancy among pediatric patients in the present study with 122 out of 158 patients (77.21%). Other malignancies are acute myeloid leukemia (AML) (13.29%) and chronic myeloid leukemia (2.59%) and lymphoma (5.69%). Nearly half of the patients were below 5 years of age (51.26%) and males were predominantly affected with frequency of 77.6%. Common clinical features were fatigue, fever, loss of appetite, bone pain, petechies, hepatic and splenomegaly, pallor, and lymphadenopathy. In ALL, most common blast type in bone marrow was L1 type (86.44%), whereas in AML, it is M2 type (80%).
Conclusion: The most common type of malignancies in pediatric age group is hematological malignancies with predominant variant is ALL. It is commonly affecting age below 5 years with male predominance.
Keywords
Acute lymphocytic leukemia
hematological malignancies
pediatric age
Introduction
Most frequent childhood cancers arise in the hematopoietic system, central nervous system (CNS), soft tissue, bone, kidney, etc. It is in sharp contrast to adults, in whom skin, lung, breast, prostate, and colon are the most common sites of tumors.1 Among all these cancers, most frequent cancer in pediatric age group is the hematological malignancy.
Worldwide, the annual number of new cases of childhood cancer exceeds 200,000 and more than 80% of these are from the developing world.2 The reported age of the standardized incidence rate for India ranges from 38 to 124 per million children per year.3 In India, one study at Tata Memorial Hospital at Bombay, in year 1979, found 271 (75.6%) of total 358 patients with acute lymphoblastic leukemia (ALL) were in pediatric age group with male predominance (70%).4 The outcome of hematological cancers in terms of long-term survival has significantly improved from 20% to 60% in ALL), from <70% to more than 90% in Hodgkin's disease, from 30% to 70% in non-Hodgkin's lymphoma (NHL), and from 10% to 40% in acute myeloblastic leukemia (AML).5
This hematological malignancy comprises a major health problem in the society due to its high mortality and morbidity. Unfortunately, there is a real paucity if epidemiologic data on pediatric cancers in India and particularly in Gujarat. In studies by Marwaha and Kulkarni,6 it is also stressed on the need for the accurate estimation of incidence and prevalence of ALL and other hematological malignancies in India to estimate the true disease burden and its impact on the population which may help in formulating the guideline. It is important to identify for prognosis and management lacunae in hematological malignancies in the pediatric population for better risk stratification and treatment.
Hence, the study is designed with special interest to find out its prevalence and early diagnosis of the disease, so more and more of this kind of malignancy can be made amenable to the treatment.
Methodology
It was a prospective observational study carried out by Pathology Department in congruence with Pediatrics Department during the period of July 2010 to October 2012. Institutional Ethics Committee permission was taken before starting the study.
Patients were recruited from outdoor and indoor Department of Pediatrics. Before enrollment in the study, the legal guardians and the patients were clearly explained about the nature of the study. The written informed consent was taken from them before enrollment of the patient in the study. Details of the patients who gave consent were noted down on the preformed case record form. Data of the patients noted were age, gender, clinical histories such as presenting symptoms, past history of any viral infection or similar complaints, family history, history of chronic disease and drug history, clinical examination data such as general examination for pallor, hepatomegaly, splenomegaly, lymphadenopathy, and systemic examination. Clinical investigations such as complete blood count (CBC), peripheral smear examination, bone marrow examination for cellularity and differential count, and immunophenotyping; biochemical examinations such as serum uric acid, serum lactate dehydrogenase, and serum electrolytes. Investigations such as renal function test, cerebrospinal fluid routine, and microscopic examination and radiological examinations were done as per the requirements. Fine-needle aspiration cytology or biopsy of lymph node was done, when lymphoma is suspected in the patient.
In laboratory investigations, the CBC was done by automated cell counter. For peripheral smear examination, blood smear was prepared manually from fresh blood without the use of anticoagulant and stained by Romanowsky stains. For bone marrow examination, the marrow was collected from anterior iliac crest, posterior iliac spines, or in case of infant anteromedial surface of tibia. The stains used for the examination of bone marrow used were Wright's stain, Giemsa stain, Leishman's stain, and Romanowsky stains and hematoxylin and eosin stain for bone marrow biopsy. Some special stains were also utilized for accurate staging of cancer differentiating from another type, like myeloperoxidase (MPO) showing brown color and stain enzyme located in the primary granules of myeloid cells. So, myeloperoxidase (MPO) stains myeloid cells of AML only and not stains lymphoblasts of ALL, which easily differentiate AML and ALL. Periodic acid–Schiff stain shows bright red color and stains glycogen. It shows characteristic block cytoplasmic positivity in ALL, so it is used in its diagnosis. It is positive in L1 and L2 but negative in L3. It is also diffusely positive in leukemic myeloblast, monoblast, and erythroblast. Sudan black B is a lipophilic dye binds irreversibly to granular component of granulocytes and give results comparable to MPO. It gives black color to granules of granulocytes.
Results
The study was carried out by pathology department with the collaboration of pediatric department. During the study duration of 2½ years, nearly about three lakh pediatric patients were examined from both indoor and outdoor pediatrics department. Moreover, within that period, a total of 158 were diagnosed as having hematological malignancy. Hence, the prevalence of hematological malignancy found in the present study was to be 52 cases per 1 lakh among pediatric patients.
The age incidence of hematological malignancy in present study shows that it is highest in 0–5 years of age with 51.26% (81) of all patients Table 1. Out of 158 patients, 123 (77.6%) patients were male and 35 (22.4%) were female. Hence, male to female ratio for hematological malignancy found to be 3.4:1. Table 2 shows frequency and age-wise distribution of various hematological malignancies in pediatric patients. ALL is the most common hematological malignancy among pediatric patients in the present study with 122 out of 158 patients (77.21%). Other malignancies are AML (13.29%) and chronic myeloid leukemia (CML) (2.59%). Lymphoma was seen in 9 (5.69%) patients. Furthermore, most of the patients (75 out of 81) below 5 years had ALL. In CML, all 4 cases are in 11–15 years age group. In lymphoma, 2 cases were of Hodgkin's Lymphoma, which is in 11–15 years age group, and 7 cases were of NHL, from which 4 cases in 6–10 years group, 2 cases in 0–5 years group, and only 1 in 11–15 years group, while AML and lymphoma were distributed evenly throughout in all age groups in pediatric patients. Figure 1 shows gender-wise distribution of various hematological malignancies. Out of 122 cases of ALL, 100 were male and 22 were female Table 2.
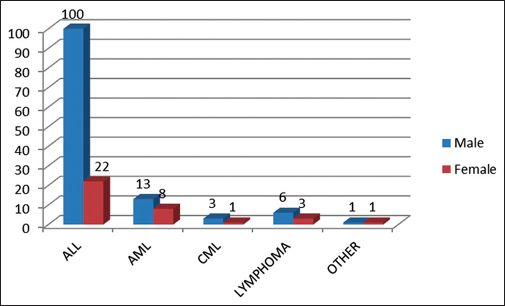
- Gender-wise distribution of each hematological malignancy
|
Age group (years) |
Number of cases (%) |
|---|---|
|
0-5 |
81 (51.26) |
|
6-10 |
53 (33.54) |
|
11-15 |
24 (15.19) |
|
Malignancy |
Age group (years) Number of cases (%) |
Total number of cases (%) |
||
|---|---|---|---|---|
|
0-5 |
6-10 |
11-15 |
||
|
ALL |
75 (47.47) |
38 (24.05) |
09 (5.70) |
122 (77.21) |
|
AML |
04 (2.53) |
10 (6.33) |
07 (4.43) |
21 (13.29) |
|
CML |
- |
- |
04 (2.53) |
04 (2.53) |
|
Lymphoma |
02 (1.27) |
04 (2.53) |
03 (1.90) |
09 (5.70) |
|
Other |
01 (0.63) |
01 (0.63) |
02 (1.27) |
|
|
Total |
81 (51.27) |
53 (33.54) |
24 (15.19) |
158 (100) |
ALL - Acute lymphocytic leukemia; AML - Acute myeloid leukemia; CML - Chronic myeloid leukemia
In the present study, the most common presenting symptom was fatigue, which was seen in 84.4% of patients followed by fever in 77.5% of cases. Other symptoms were loss of appetite (44.8%), loss of weight (36.2%), bone pain (29.3%), cough and cold (29.3%), petechiae (25.8%), and CNS symptoms (10.3%). While most common presenting signs were splenomegaly and pallor, which were seen in 82.7% and 81.0%, respectively, other common signs found were hepatomegaly (65.5%) and lymphadenopathy (36.2%) Table 3.
|
Symptoms |
Number of cases (%) |
|---|---|
|
Fatigue |
133 (84.4) |
|
Fever |
122 (77.5) |
|
Loss of appetite |
70 (44.8) |
|
Weight loss |
57 (36.2) |
|
Bone pain |
46 (29.3) |
|
Cough/cold |
46 (29.3) |
|
Petechiae |
39 (25.8) |
|
CNS symptoms (vomiting) |
15 (10.3) |
|
Clinical signs |
|
|
Splenomegaly |
130 (82.7) |
|
Hepatomegaly |
103 (65.5) |
|
Pallor |
128 (81.0) |
|
Lymphadenopathy |
57 (36.2) |
CNS - Central nervous system
Table 4 shows laboratory findings in all the patients. Anemia was seen in 98.20% of patients and among them 68.96% patients have severe anemia (<7 g%). These findings are correlating with clinical examination, which shows pallor in 82.7% of cases. Most of the patients (98.87%) had white blood cell (WBC) count >10,000/mm3 with 27.60% had >50,000/mm3. Two patients had WBC count <5000/mm3. Type of blast found in bone marrow examination seen in Table 5. In the present study, total ALL cases were 122, but four cases were in remission. Hence, bone marrow shows normal finding in that cases, but they were known case of ALL-L1. Figures 23 show the peripheral smear and bone marrow smear from a 5-year-old child diagnosed as ALL-L1. Peripheral smear stained with Leishman's stain and bone marrow smear stain with negative peroxide smear. There are small lymphoblasts and homogenous chromatin with scant cytoplasm. Out of remaining 118 cases, L1 type of lymphoblast was seen in 86.44% case,’ L2 type in 11.86% cases, and L3 type in 1.69% of cases. Hence, L1 is predominant type of lymphoblast in ALL, comprising three-fourth of the cases. In AML, 10% of cases had blasts of M1 type, 80% had M2 type, and 10% had M3 type of myeloblast. Figure 4 shows peripheral smear of AML M3 case. It shows myeloblasts with high N: C ratio, prominent nucleoli, and Auer rods in cytoplasm, while Figure 5, which is bone marrow aspirate from a case of AML – M3, shows promyelocytes with primary granules and faggot cell. Two cases of chronic phase of CML and six cases of NHL show no increase marrow blast. Only one case of NHL showed bone marrow involvement.
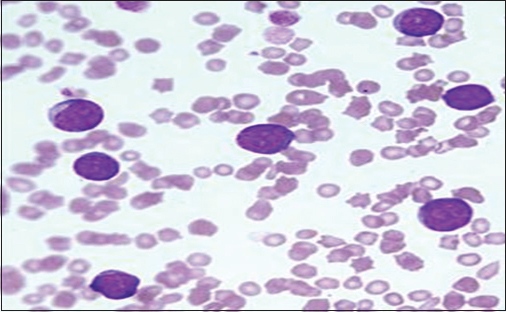
- Peripheral smear from a 5-year-old child diagnosed as acute lymphocytic leukemia-L1 (Leishman's stain, oil immersion field)
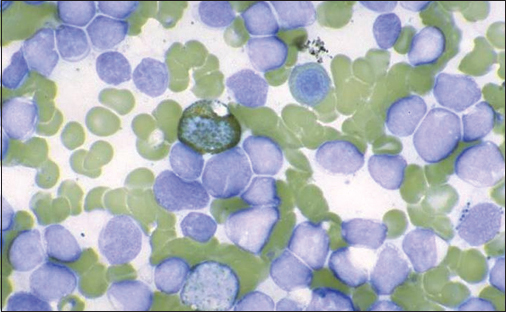
- Negative peroxidase stain in acute lymphocytic leukemia, bone marrow aspirate

- Peripheral smear from a case of acute myeloid leukemia show myeloblasts with high N:C ratio, prominent nucleoli, and Auer rods in cytoplasm

- Bone marrow aspirate from a case of acute myeloid leukemia - M3 shows promyelocytes with primary granules and faggot cell
|
Laboratory feature |
Value |
Number of cases (%) |
|---|---|---|
|
Hemoglobin (g%) |
<7 |
108 (68.96) |
|
7-11 |
46 (29.32) |
|
|
>11.0 |
02 (1.72) |
|
|
WBC count (per mm3) |
<5000 |
02 (1.72) |
|
5000-9999 |
13 (8.62) |
|
|
10,000-49,999 |
98 (62.06) |
|
|
>50,000 |
44 (27.60) |
|
|
Platelet count (per mm3) |
<20,000 |
32 (20.68) |
|
20,000-99,999 |
95 (60.36) |
|
|
≥1 lakh |
30 (18.96) |
WBC - White blood cell
|
Blast type |
Number of cases (%) |
|---|---|
|
Lymphoblast (among total cases of ALL) |
|
|
L1 |
102 (86.44) |
|
L2 |
14 (11.86) |
|
L3 |
02 (1.69) |
|
Myeloblast (among total cases of AML) |
|
|
M0 |
- |
|
M1 |
02 (10) |
|
M2 |
17 (80) |
|
M3 |
02 (10) |
|
M4 |
- |
|
M5 |
- |
|
M6 |
- |
|
M7 |
- |
|
No increase marrow blast |
04 |
ALL - Acute lymphocytic leukemia; AML - Acute myeloid leukemia
Discussion
Hematological Malignancies accounts approximately for one-third of total cancers occurring in early childhood, with ALL being the most common entity with peak prevalence 2-5 years of age.7,8 In the present study, within 2½ years duration nearly three lakh patients from indoor and outdoor departments of pediatrics were screened for hematological malignancies. Among them, 158 patients found various clinical and hematological findings of hematological malignancies.
In the present study, it was found that nearly 94% patients had leukemia. Similar finding was seen with other studies done by Young et al. and Teppo et al.9,10 However, the frequency of leukemia is quite high in the present study as compared to the above-mentioned studies. This difference can be explained by the large number of patients (51.26%) in the age group 0–5 years, in which ALL is the most common malignancy. The studies done in various states of India showed similar findings like present study. A study in West Bengal had incidences of 84% and 16%, respectively, for leukemia and lymphoma.11 Similarly, studies done in Odisha in 2007 show 90% and 10%, respectively, and in Gujarat in 2010, the incidences for leukemia and lymphoma were 91% and 9%, respectively.12 While one study in Rajasthan (1991) had reverse finding with incidence of leukemia and lymphoma were 48% and 52%, respectively.13 The incidence of ALL found in the present study was 77.21%. It shows that more than three-fourth patients in the present study are suffering from ALL. Similarly, data of other countries show the ALL is the most frequently diagnosed malignancy in children, representing nearly one-third of all pediatric cancers.14 Data from Hong Kong shows that ALL is contributing 57% in all hematological malignancies with AML and CML combined 22% and 21% lymphoma. Similar findings were seen in the United States. While in France, the incidence of lymphoma was slightly higher than other countries. In France, lymphoma was contributing 31% of the total hematological malignancies.15 In the present study, incidence of hematological malignancy was very much high in male patients, i.e., 77.6% of cases were male. Similar findings were seen with other studies done by Das et al. and Li et al.16,17
Presenting signs and symptoms of the patients in the present study were fatigue, pyrexia, anorexia, pallor, splenomegaly, and hepatomegaly, which is seen with similar frequencies in the study by Das et al. and Siddaiahgari et al.16,18 Anemia is invariably present in all patients in the present study. Only 1.72% patient in this study and 3% in Das study have hemoglobin level >11 g%. Looking at total count, most of the patients have total count between 10,000 and 50,000. While interpreting the total count, we should keep leukemoid reaction in mind as it can produce total count in the same range too. Leukemia can be differentiated from leukemoid reaction by examining the peripheral smear and bone marrow.
Conclusion
In summary, the most common age group of hematological malignancies in the present study is below 5 years with most common is ALL. Males are commonly affected than females. In ALL, the most common type of lymphoblast seen was L1 type. While in AML, the most common myeloblast was M2 type.
The sample size of the study was quite good. However, because of less funding the laboratory evaluation by flow cytometry, karyotyping, and fluorescence in situ hybridization analysis could not be done.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders; 2005. p. :499.
- [Google Scholar]
- Pediatric oncology in countries with limited resources In: Pizzo P A, Poplack D G, eds. Principles and Practice of Pediatric Oncology (5th ed.). Philadelphia: Lippincott Williams and Wilkins; 2006. p. :1605-17. editors.
- [Google Scholar]
- Biology and treatment of acute lymphoblastic leukemia. J Pediatr. 1994;124:491-503.
- [Google Scholar]
- Pediatric oncology in India: Past, present and future. Indian J Med Paediatr Oncol. 2009;30:121-3.
- [Google Scholar]
- Childhood acute lymphoblastic leukemia: Need of a national population based registry. Indian Pediatr. 2011;48:821.
- [Google Scholar]
- Principle and Practice of Paediatric Oncology (5th ed.). Philadelphia: Lippincott Williams & Wilkins; 2006. p. :539-90.
- [Google Scholar]
- A study of 1226 leukemia cases-Epidemiologic and end result analysis. The Indian J of Cancer. 1979;16:8-17.
- [Google Scholar]
- Descriptive epidemiology of leukemias in Greater Mumbai. Natl Med J India. 1998;11:116-9.
- [Google Scholar]
- The pattern of paediatric malignancies is Rajasthan. Indian Pediatrics. 1991;28:1517-8.
- [Google Scholar]
- Acute lymphoblastic leukemia in adolescents and young adults. Hematol Oncol Clin North Am. 2009;23:1033-42. vi
- [Google Scholar]
- Incidence of childhood cancer in France: National Children Cancer Registries, 2000-2004. Eur J Cancer Prev. 2010;19:173-81.
- [Google Scholar]
- Clinical presentation of leukemias in children in south Kerala. Indian Pediatr. 1974;11:431-8.
- [Google Scholar]
- Epidemiology of paediatric cancer in Hong Kong, 1982 to 1991. Hong Kong Cancer RegistryHKMJ. 1999;5:128-34.
- [Google Scholar]
- Clinical, immunophenotype and cytogenetic profile of acute lymphoblastic leukemia in children at tertiary health care centre in India. Muller J Med Sci Res. 2015;6:112-8.
- [Google Scholar]







