Translate this page into:
Challenging Management of Large Aggressive Fibromatosis of the Anterior Abdominal Wall: A Case Report
Address for correspondence Rhita Salah, Department of Orthopedic Surgery and Traumatology, Military Hospital Mohammed V, Rabat, Morocco. rhita.salah@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aggressive fibromatosis is a rare and benign tumor of soft tissues, locally invasive but never metastasizes. This proliferation arises in musculoaponeurotic structures. It is more common in young fertile women due to hormonal influences. Radical resection with free margins is the key to an effective outcome. We present here the case of a 47-year-old woman, without medical history, who was referred to our hospital for a painful swelling of the left iliac fossa, diagnosed with aggressive fibromatosis of the anterior abdominal wall based on radiological and histological findings. She underwent an excision of the mass with free margins followed by reconstruction of the musculo-fascial defect. After a follow-up of 12 months, there was no evidence of recurrence. Management of aggressive fibromatosis remains a challenge for surgeons. Complete excision of the tumor followed by reconstruction of abdominal wall defect is the first choice of treatment.
Keywords
abdominal wall
aggressive fibromatosis
radical excision
Introduction
Aggressive fibromatosis, also known as desmoid tumor, is a rare and benign tumor of soft tissues. It was first described by Macfarlane in 1832. Although benign, this tumor is characterized by aggressive local infiltration of surrounding tissues, without metastatic potential. Aggressive fibromatosis is more common in women and usually occurs between puberty and 40 years. Most cases are sporadic but sometimes it is associated to familial adenomatous polyposis and Gardner's syndrome. Surgery is the mainstay of treatment. There is, however, a high risk of recurrence especially when excision is incomplete.
Case Presentation
A 47-year-old woman, without medical history, gravida 3, para 3, all deliveries were natural, with regular menses, presented with a painful swelling of the left iliac fossa.
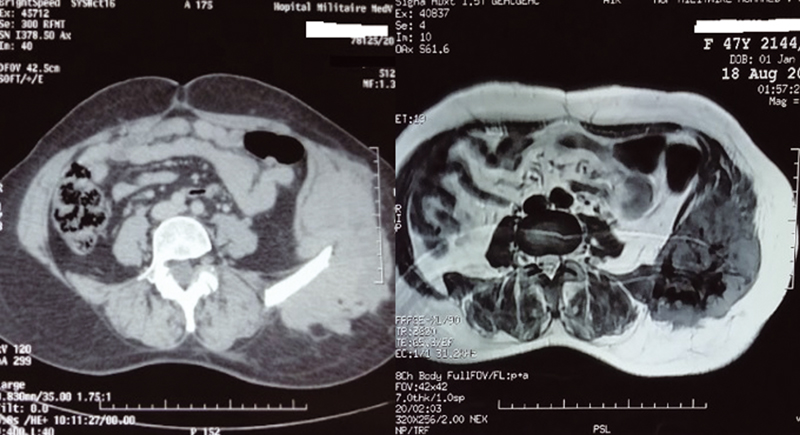
The mass was slowly increasing in size in the last year. The patient had normal vital signs and no fever. Physical examination found a nontender, firm, well-circumscribed mass measuring 15 × 7 cm in the left iliac fossa, adherent to the anterior abdominal wall musculature. The neurological and vascular examination found no abnormalities. The examination of lymph nodes showed no lymphadenopathy. Abdominal computed tomography (CT) revealed the presence of a voluminous soft tissue mass of the left flank, centered on the left iliac crest without bone invasion, measuring 80 × 125 × 140 mm (Fig. 1).
-
Fig. 1 Abdominal computed tomography (CT) revealing the presence of a voluminous soft tissue mass of the left flank, centered on the left iliac crest without bone invasion (left) and magnetic resonance imaging (MRI) sequences showing the lesion (right).
Magnetic resonance imaging (MRI) showed a heterogeneous process of the left anterolateral abdominal wall, centered on the left iliac crest, with extensive local invasion of soft tissues. The lesion is in low-signal-intensity in T1-weighted and high-signal-intensity in T2-weighted and short-tau inversion recovery (STIR) sequences, and heterogeneously enhanced after injection of gadolinium, measuring 117 × 78 × 103 mm (Fig. 1).
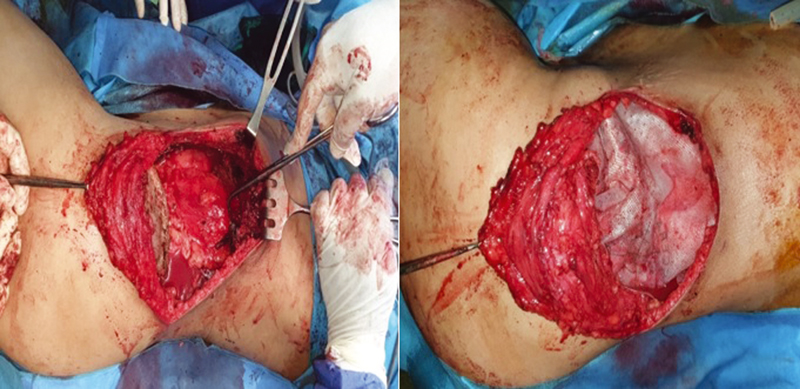
A biopsy was then performed and was consistent with an aggressive fibromatosis. She underwent under general anesthesia and in right lateral decubitus, a full-thickness excision of the tumor with a 3-cm wide margins of healthy tissue down to the peritoneum. The tumor was adherent to the left iliac crest, part of which was resected (Fig. 2).
-
Fig. 2 Peroperative view of the excision showing the adherence of the tumor to the left iliac crest (left) and peroperative view showing reconstruction of musculo-fascial defect using a dual-sided polypropylene mesh (right).
Musculo-fascial defect was closed by suturing a dual-sided polypropylene mesh to the excision edges of the anterior abdominal wall musculature (Fig. 2).
Skin was closed in the usual manner. Evolution was uneventful after a follow-up of 12 months with no evidence of recurrence.
Discussion
Aggressive fibromatosis is a benign and uncommon soft tissue tumor with an approximative incidence of 2 to 4 patients per million individuals.1 They account for 0.03% of all tumors and 3% of soft tissue tumors.2 It occurs more often in women, with a twofold female predominance according to Phillips et al.3
Aggressive fibromatosis is usually found in young adults between puberty and 40 years,4 mainly in young fertile women due to hormonal influences particularly during pregnancy,5 or in patients with previous history of trauma or surgical scars.6
These tumors are divided into three groups: extra-abdominal, abdominal, and intraperitoneal, of which the anterior abdominal wall is the site of predilection with an incidence of 50%.5
It is a locally aggressive fibroblastic proliferation arising in musculoaponeurotic structures. Unlike fibrosarcoma, it never metastasizes. It has, however, a high risk of recurrence, hence its classification with malignant soft tissue neoplasms, comprising fewer than 4%.7
Macfarlane was the first to describe the pathology in 1832,8 but the designation “desmoid” was given only in 1838 by Muller, relating to the Greek word “Desmos” which means “band” or “tendon.”9
X-rays are either normal or they show an amorphous soft tissue density mass. Ultrasound typically reveals a hypoechoic, lobulated, or infiltrative mass. CT scan shows enhancing soft tissue mass iso- or hypodense to surrounding muscle. MRI is the diagnostic method of choice, allowing tumor evaluation both before and after resection. It provides not only a superior soft tissue resolution compared with other radiological techniques, but also a better assessment of local structures involvement such as vessels, nerves, viscera, and bones. On MRI, the mass is ovoid or irregular and crosses fascial compartments. Aggressive fibromatosis lesions are commonly homogeneously isointense on T1-weighted sequences, heterogeneously hyperintense on T2-weighted and STIR sequences, and enhance after gadolinium injection. Bands of low signal are usually seen on all sequences.10
It should be noted that histological confirmation is required for final diagnosis. Aggressive fibromatosis is characterized by long sweeping fascicles of differentiated fibroblastic cells with ill-defined cytoplasmic borders. The lesion is typically surrounded by compressed atrophic muscle fibers. Microscopic tumor infiltration beyond margins is often seen which explains recurrences after surgical excision.11
The main differential diagnosis of desmoid tumors is malignant soft tissue sarcoma. On MRI, malignant soft tissue sarcomas typically form a pseudocapsule and respect fascial boundaries. Also, they can outstrip their blood supply resulting in central necrosis. On the other hand, aggressive fibromatosis crosses fascial boundaries and does not show central necrosis, which helps differentiate the two lesions.10 However, histological confirmation is mandatory for the final diagnosis of both conditions.
Radical tumor resection with free margins is recommended as first-line therapy and is principal determinant of outcome. However, the optimal treatment strategy is still uncertain. Patients with aggressive fibromatosis are treated by resection alone when negative margins can be achieved. As these tumors arise from the anterior abdominal wall musculature and reach the peritoneal layer, and to avoid hernia, radical resection should be followed by reconstruction of the defects using synthetic material. Skin is, however, spared of any extension, and is usually closed by approaching wound edges.6
Nonsurgical methods of treatment such as radiotherapy, hormonotherapy, and chemotherapy are more recently described in the literature, and can be considered for treating recurrent aggressive fibromatosis whenever they are unresectable.5,12
Radiotherapy in the treatment of aggressive fibromatosis can lead to long-term control, although it should be avoided in patients with abdominopelvine localization, as the risk of higher grade complications is substantial.13
Local control after surgery implies that tumor is completely removed with no evidence of recurrence after long-term follow-up, whereas stabilization or regression sign local control after radiotherapy or chemotherapy. According to a retrospective case series of 174 patients receiving a complete excision with free margins, local recurrence rate after 10 years was of 58%.4
Horsley et al highlighted the main factors that may predict recurrence; age and gender, tumor volume, and location. Note that 83% of patients under 30 years, 58% of females, 100% of tumors larger than 300 mL, and 67% of patients with lower limb presentation recurred.14
Conclusion
Management of aggressive fibromatosis remains a challenge for surgeons, however feasible. We suggest through this case report and in light of results reported in the literature that, complete excision of the tumor followed by reconstruction of abdominal wall defect is the first choice of treatment but not the unique one, as nonsurgical treatments such as radiotherapy, chemotherapy, and hormonotherapy have been recently used.
Acknowledgments
None.
Conflict of Interest
None declared.
References
- Individualizing management of aggressive fibromatoses. Int J Radiat Oncol Biol Phys. 1998;40(03):637-645.
- [Google Scholar]
- IARC and Lyon: Desmoid-Type Fibromatosis in WHO Classification of Tumors of Soft Tissue and Bone 2013. p. :72-73.
- [Google Scholar]
- Aggressive fibromatosis of the abdominal wall, limbs and limb girdles. Br J Surg. 2004;91(12):1624-1629.
- [Google Scholar]
- Outcome of surgery for primary and recurrent desmoid-type fibromatosis. A retrospective case series of 174 patients. Ann Med Surg (Lond). 2017;17:14-19.
- [Google Scholar]
- Surgical management of large desmoid tumour of the anterior abdominal wall. Asian J Surg. 2008;31(02):90-95.
- [Google Scholar]
- Abdominal wall reconstruction after desmoid type fibromatosis radical resection: case series from a single institution and review of the literature. Int J Surg Case Rep. 2017;33:167-172.
- [Google Scholar]
- Clinical Reports of the Surgical Practice of the Glasgow Royal Infirmary In: D Robertson Glasgow. 1832.
- [Google Scholar]
- Uber den feineran Bau and die For-man der Krankhauten Geschwulste In: Berlin G Reimer. 1838.
- [Google Scholar]
- Aggressive fibromatosis: MRI features with pathologic correlation. AJR Am J Roentgenol. 2006;186(01):247-254.
- [Google Scholar]
- Les tumeurs desmoïdes de la paroi abdominale: quelle stratégie chirurgicale? (A propos de deux cas)
- Desmoid-type fibromatosis in children. Clinical features, treatment response, and long-term follow-up. Medicina (B Aires). 2020;80(05):495-504.
- [Google Scholar]
- Radiotherapy in the treatment of aggressive fibromatosis: experience from a single institution. Radiat Oncol. 2020;15(01):143.
- [Google Scholar]
- Fibromatosis: a review of the risk factors for recurrence and outcomes. Acta Orthop Belg. 2020;86:55-60. (S1):
- [Google Scholar]







