A Rare Case of Extraskeletal Primary Osteosarcoma of Breast: How We Managed
Address for correspondence Venkata Pradeep Babu Koyyala, MD, Department of Medical Oncology, Rajiv Gandhi Cancer Institute and Research Centre, Room: 2262, 2nd Floor C Block, Sector 5, Rohini, New Delhi 110085, India. pradeepbabu.koyyala@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary osteosarcoma arising in breast is a rare form of extra skeletal osteosarcoma, accounting for less than 1% of all breast cancers and 12.5% of sarcomas arising in breast. Fewer than 150 cases of primary osteosarcoma of breast have been reported in the medical literature in the last 50 years. It was reported to have worse outcome compared to typical skeletal osteosarcoma. Osteosarcoma of breast presents in elderly age group unlike skeletal osteosarcoma, which occurs in young people. Diagnosis is by histopathological examination of malignant osteoid and ruling out underlying skeletal involvement.
Keywords
osteosarcoma
breast
mammography
Introduction
Primary osteosarcoma arising in the breast is a rare form of extraskeletal osteosarcoma, accounting for less than 1% of all breast cancers and 12.5% of sarcomas arising in the breast. Fewer than 150 cases of primary osteosarcoma of breast have been reported in the medical literature in the past 50 years.1,2 It was reported to have worse outcome compared with typical skeletal osteosarcoma. Osteosarcoma of breast presents in older age group in sixth decade unlike skeletal osteosarcomas that occur in young people.3 Diagnosis is performed by histopathological examination of malignant osteoid and ruling out underlying skeletal involvement. In this letter, we report this rare case and management in our institute, as guidelines are not well defined in this scenario.
Case Report
A 54-year-old hypertensive, diabetic, postmenopausal woman presented to surgical oncology department with complaint of left breast lump for 6 months. Bilateral mammography showed well-defined mass lesion in upper outer quadrant left breast with BIRADS score 0. Fine-needle aspiration cytology (FNAC) was inconclusive. Ultrasonography (USG)–guided tru-cut biopsy from lesion showed proliferation of neoplastic cells, which were spindled, exhibiting marked nuclear atypia with metaplastic osteoid deposition and woven bone formation with differentials of metaplastic carcinoma and osteosarcoma of the left breast. Magnetic resonance imaging (MRI) mammography showed lobulated peripherally enhancing lesion in left outer central quadrant with thick nodular enhancement on lateral aspect, showing washout kinetics, measuring 2.9 (ap) × 3.3 (tr) × 3.0 (cc) cm, lying 1.6 cm away from overlying skin, 2.3 cm from chest wall, and 9.0 cm from nipple. Few sub-centimetric axillary lymph nodes were seen. No nipple invasion, skin involvement, and chest wall invasion were seen. No enlarged intramammary/internal mammary nodes were seen, and BIRADS score was 5. Whole-body positron emission tomography–computed tomography (PET-CT) showed metabolically active oval soft tissue density mass lesions in outer quadrant of the left breast with peripheral calcification along the lateral border likely to be probably mitotic. Metabolically inactive sub-centimeter–sized left axillary lymph nodes were observed. No metabolically active lesion was found anywhere else in the body.
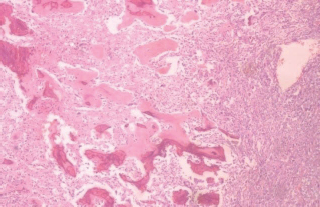
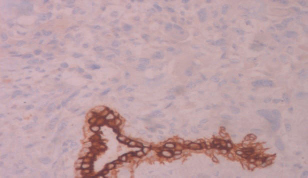
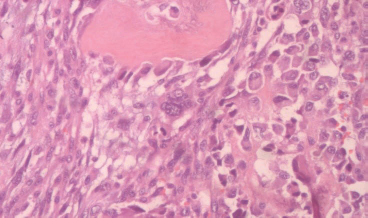
The patient was optimized for surgery. Wide local excision and axillary lymph node dissection was done. Postoperative period was uneventful. Final histopathological report showed partly circumscribed tumor composed of neoplastic cells arranged in solid sheets and cells with vesicular nuclei and conspicuous nucleoli. Marked nuclear atypia is seen. Mesenchymal differentiation is present in the form of lacy osteoid and bony trabeculae (Figs. 12). No necrosis, ductal carcinoma in situ (DCIS), and lobular carcinoma in situ (LCIS) were seen. Tumor did not infiltrate the overlying epidermis. No skeletal muscle was present in margins. All margins were free of tumor. The distance from closest margin was 0.9 cm (deep margin). No lymphovascular emboli and dermal lymphovascular emboli were identified. Twenty-nine axillary lymph nodes were dissected, and all were free of tumor. On IHC, the tumor was negative for pan cytokeratin and Cytokeratin 8/18. The final impression was osteosarcoma of the left breast with stage pt2n0.ER/PR/her2-nu-negative (Fig. 3).
-
Fig. 1 Proliferation of neoplastic spindle cells with extensive osteoid deposition (H&E ×10). H&E, hematoxylin and eosin.
-
Fig. 2 Spindle to epithelioid plump neoplastic cells with high-grade nuclear atypia, mitosis, and tumor giant cell (H&E ×40). H&E, hematoxylin and eosin.
-
Fig. 3 Cytokeratin (CK) highlights the entrapped normal duct while the tumor cells are negative (IHC stain ×20). IHC, immunohistochemistry.
The patient received 60 gray in 30 fractions radiotherapy by tangential fields on 6 mV LINAC. Adjuvant chemotherapy with ifosfamide, adriamycin, and cisplatin was given, and presently the patient is on regular follow-up.
Conflict of Interest
None declared.
References
- Primary breast sarcoma: clinicopathologic series from the Mayo Clinic and review of the literature. Br J Cancer. 2004;91(02):237-241. Review
- [Google Scholar]
- Primary osteogenic sarcoma of the breast: a clinicopathologic analysis of 50 cases. Am J Surg Pathol. 1998;22(08):925-933.
- [Google Scholar]







