Translate this page into:
A case of diffused large B-cell lymphoma in an elderly patient successfully treated with R-mini-CHOP
Corresponding author: Faisal Syarifuddin, Departement of Internal Medicine, Hematology-Medical Oncology Division, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia. faisals2711@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Syarifuddin F, Rajabto W, Billianti YD. A case of diffused large B-cell lymphoma in an elderly patient successfully treated with R-mini-CHOP. Asian J Oncol, 2024;10:10. doi: 10.25259/ASJO-2023-15 – (477)
Abstract
Diffuse large B-cell lymphoma (DLBCL) is a diverse group of B-cell lymphomas that vary in their clinical characteristics. Usually manifesting as a rapidly progressing or advanced condition, it is often curable even at advanced stages. The illness originates in extranodal and extramedullary tissues in 40% of patients. Patients over the age of 80 who have comorbidities or fragile conditions may be eligible for Rituximab and Reduced Dose CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) (R-mini-CHOP) chemoimmunotherapy. We report a 75-year-old woman with a tumor on the right side of the nose that covers the eye, so it is easy to fall out. The diagnosis of DLBCL (sinonasal) was made on the basis of computed tomography (CT) scan of the paranasal sinuses with contrast and immunohistochemical examination. Due to the age of the patient, who was included in the very elderly category with moderate frailty based on instrumental activities of daily living (IADLs), the patient was given R-mini-CHOP chemoimmunotherapy for six cycles, followed by radiation as much as 20 × 18 Gray (Gy) where the patient in the final evaluation stated complete response.
Keywords
Diffuse large B-cell lymphoma
Elderly
R-mini-CHOP
INTRODUCTION
Diffuse large B-cell lymphoma (DLBCL) is a diverse group of B-cell lymphoma that usually appears as a severe or advanced form of the illness. However, it can still be cured even at advanced stages. Approximately one-third of individuals have systemic symptoms, which may include constitutional B symptoms.[1]
The prevalence of DLBCL in the United States and England is estimated to be around seven cases per 100,000 individuals annually. The annual incidence rate in europe is around 4.92 cases per 100,000 individuals. Similar to the majority of other non-hodgkin lymphomas (NHLs), there is a higher proportion of males, with around 55% of cases occurring in men. The frequency of occurrence rises with advancing age; the midpoint age at which the condition is first seen is 64 years. Individuals diagnosed with DLBCL commonly exhibit a swiftly growing tumor that causes noticeable symptoms. The illness originates in extranodal and extramedullary tissues in 40% of patients. The stomach/gastrointestinal tract is the most frequent location for primary extranodal illness. However, the illness can manifest in almost any type of tissue, such as the testis, bone, thyroid, salivary glands, tonsil, skin, liver, breast, adrenals, kidneys, nasal cavity, ocular adnexa, paranasal sinuses, uterine cervix, vagina, and central nervous system.[2]
DLBCL patients at all stages are treated with systemic chemoimmunotherapy to cure the disease. Multiple trials have demonstrated that administering R-CHOP every 21 days has considerably improved response rates, progression-free survival (PFS), and overall survival (OS) as compared to CHOP alone in individuals who have not received treatment before. Patients over the age of 80 who have comorbidities or fragile conditions may be eligible for R-mini-CHOP chemoimmunotherapy.[3]
In this article, we report the case of DLBCL (sinonasal) in an elderly patient with moderate frailty successfully treated with R-mini-CHOP.
CASE REPORT
A 75-year-old female complained that her left nostril had been frequently blocked since september 2020, accompanied by frequent discharge of clear fluid and bleeding, which then stopped on its own. In october 2020, the patient went to an ear, nose, and throat (ENT) hospital after a computed tomography (CT) scan of the paranasal sinuses found a mass in the left side of the nasal cavity with a size of approximately 5 cm and was advised for surgery, but the patient refused. In december 2020, a tumor appeared on the right side of the nose; initially small, it grew bigger until it had been protruding since january 2021. So the patient decided to seek treatment at cipto mangunkusumo hospital. There were no complaints of fever or night sweats; the patient had lost 3 kg of weight in the last two months. Because the lump on the face was getting bigger, the patient could not see with the right eye; was often dizzy; and fell easily as she lacked balance. The patient also felt severe pain at the location of the lump on the face, so she slept more and had less appetite.
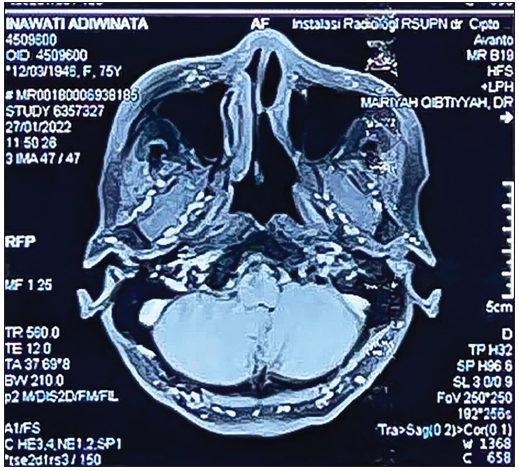
On physical examination, there was a mass on the face covering the right orbit and maxillary region; the mass covered the bridge of the nose, dorsum nasi to ala nasi dextra; it was seen that the right anterior nares were closed. On the CT scan of the paranasal sinuses with contrast [Figure 1], a malignant mass of the left nasal cavity with the largest dimension of 10 × 6.8 × 4.3 cm differential diagnosis (DD) of squamous cell carcinoma was found. A biopsy of the sinonasal mass was found histologically consistent with a malignant tumor DD: non-Hodgkin’s malignant lymphoma. Immunohistochemistry [Figure 2] matches non-Hodgkin’s lymphoma, diffuse, large cell, and CD20+. Thorax photos did not show radiological abnormalities in the heart and lungs, abdominal ultrasound showed no signs of metastases in the liver and spleen, and no ultrasound abnormalities in the visualized intra-abdominal organs. Bone marrow biopsy revealed normocellular bone marrow and no lymphoma cell infiltration was found. Echocardiography revealed global normokinetic, suitable valve, ejection fraction (EF) 74%, and mild diastolic dysfunction. The complete peripheral blood count and routine chemistry were within normal limits.
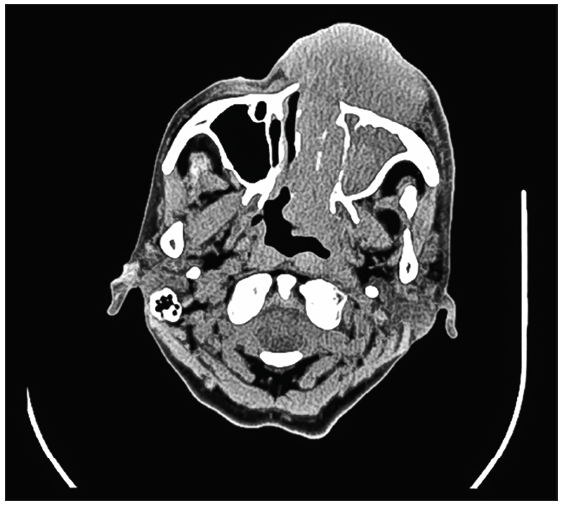
- CT scan of the paranasal sinuses with contrast before R-Mini-CHOP chemoimmunotherapy. CT: Computed tomography, R-mini-CHOP: Rituximab and Reduced Dose CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone).
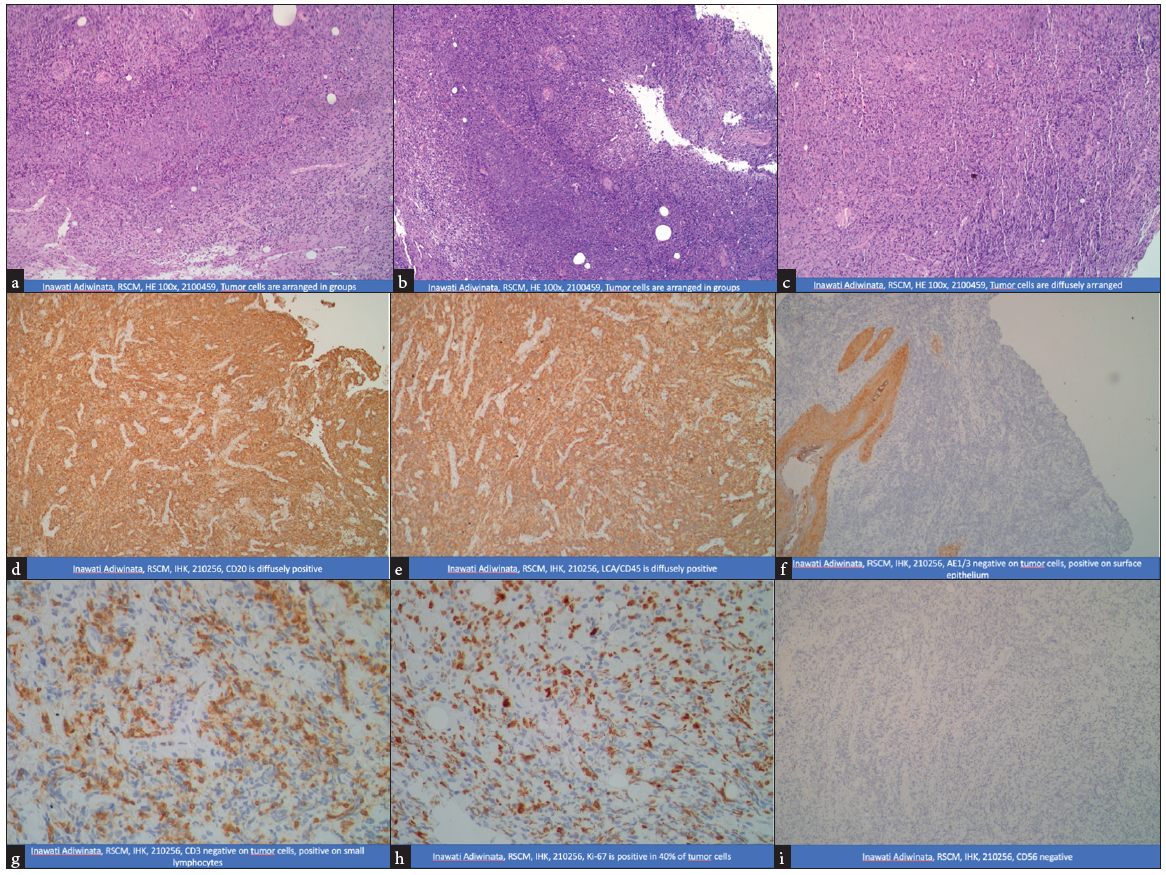
- Immunohistochemistry. RSCM: Rumah sakit ciptomangunkusumo (Ciptomangunkusumo Hospital), HE: Hematoxylin and eosin stain, IHK: Imunohistokimia (Immunohistochemistry), CD: Cluster of differentiation, LCA: Leukocyte common antigen.
The patient was diagnosed as DLBCL (Sinonasal) stage IE (Ann Arbor) with an international prognostic index (IPI) score of 1. Based on IADLs, the patient was categorized as having moderate frailty; so immunochemotherapy was chosen with the R-mini-CHOP regimen. After undergoing the third cycle of R-mini-CHOP chemoimmunotherapy, a physical examination found a mass in the maxillary right covering the dorsum nasi and the lateral region of the ala nasi dextra with a size of 4 × 2 cm, nares anterior dextra passage (+), and mass (‒). Contrast paranasal sinus CT scan [Figure 3] found mass size reduced by > 50% and partial response impression based on the lugano classification.
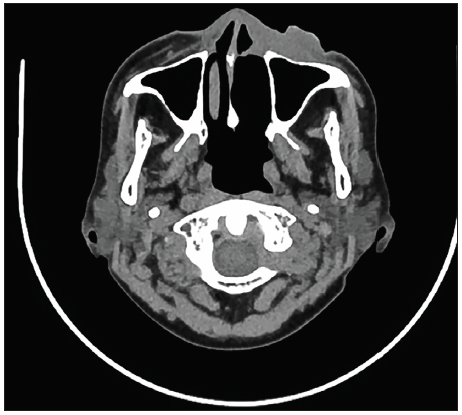
- CT scan of the paranasal sinuses with contrast after undergoing the third cycle of R-mini-CHOP chemoimmunotherapy. R-mini-CHOP: Rituximab and Reduced Dose CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone), CT: Computed tomography.
Due to the good response to therapy, chemoimmunotherapy with R-mini-CHOP was continued until the sixth cycle. Then an evaluation was carried out with a positron emission tomography (PET)-CT scan and laboratory. The evaluation results of the physical examination found a mass in the maxillary right covering the lateral region of the ala nasi dextra measuring 2 × 1.2 cm, nares anterior right passage (+), and mass (‒). PET-CT scan [Figure 4] no longer found a lymphoma mass in the nasal cavity, but found nonmetabolic residual lymphoma in the subcutaneous fat of the left maxilla medial in a part of the left nasal. On hematological examination, complete peripheral blood was obtained, and routine chemistry was within normal limits. Still, an increased lactate dehydrogenase (LDH) level was found, namely 281 U/L (125–220). Therapy was continued with local external radiation therapy of 20 × 1.8 Gray (Gy). On physical examination after completing 20 cycles of radiation, there was no mass in the maxillary dextra; with the results of a nasopharyngeal magnetic resonance imaging (MRI) post-radiation evaluation [Figure 5], it was found that there was still a thickening of the cutis/subcutis in the left maxillary region to the left side of the nose due to inflammation; so then it was categorized as complete remission (based on the lugano classification). On hematological examination, complete peripheral blood count, routine chemistry, and LDH were within normal limits.
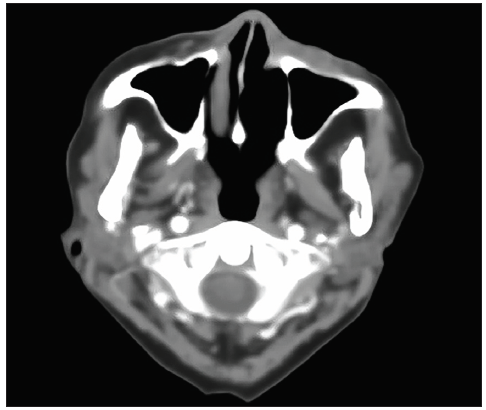
- PET-CT scan after finishing the sixth cycle of R-mini-CHOP chemoimmunotherapy. PET-CT: Positron emission tomography-computerized tomography, R-mini-CHOP: Rituximab and Reduced Dose CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone).
- Nasopharyngeal MRI with contrast after 20 cycles of radiation. MRI: Magnetic resonance imaging.
DISCUSSION
NHL is a heterogeneous group of lymphoproliferative malignancies that is much more difficult to predict than Hodgkin’s lymphoma and has a much greater predilection for extranodal spread. Non-Hodgkin’s lymphoma can be located in several parts of the head and neck region, including Waldeyer’s ring, oral mucosa, salivary glands, paranasal sinuses, laryngeal tissue, and bone structures. Non-Hodgkin lymphoma is the second most prevalent malignancy in the head and neck region behind the squamous cell carcinoma. Primary sinonasal lymphoma is an uncommon form of NHL, accounting for around 1% of all head and neck malignancies. It is often diagnosed in individuals with a median age of 67.8 years. The sinonasal tract is linked with two subtypes: DLBCL and extranodal natural killer/T-cell lymphoma (ENKTL), nasal type.[4,5]
DLBCL is a B-cell lymphoma that is aggressive but has the potential to be cured. Various treatment strategies are determined by the pathological diagnosis of lymphoma. The first-line treatment for B-cell extranodal lymphoma is the CHOP chemotherapy regimen, which includes cyclophosphamide, doxorubicin, vincristine, and prednisolone. Combining rituximab with chemotherapy significantly improves the prognosis of patients with DLBCL due to the emergence of immunochemotherapy. Rituximab improved complete response (CR), PFS, and event-free survival (EFS).[1,2]
Multiple phase 3 trials have shown the efficacy of R-CHOP immunochemotherapy in treating advanced DLBCL. In the MInT study, patients aged 18–60 years, who received six cycles of R-CHOP treatment, had a six-year OS rate of 90% and a PFS rate of 80%.[6] R-CHOP-21 was associated with 81% two-year OS and 75% two-year PFS in patients ≥ 21 years of age.[7] Similar results were reported for patients ≥ 60 years; The three-year OS was 67% and the three-year PFS was 53%.[8] Eight cycles of R-CHOP in adults aged 60–80 were associated with a 44% ten-year OS and 37% ten-year PFS.[9]
In patients aged over 80 years in frail conditions with comorbidities or with limited cardiac function, it is advisable to use a chemotherapy regimen to reduce toxicity that exacerbates comorbidities. There is no suitable chemoimmunotherapy regimen, but one of the following regimens may be considered as an option for this condition:
-
R-GCVP (Rituximab, Gemcitabine, Cyclophosphamide, Vincristine, Prednisolone)
-
R-mini-CHOP (CHOP dose reduced by conventional Rituximab dose)
-
R-CEOP (Rituximab, Cyclophosphamide, Etoposide, Vincristine, Prednisone)
The therapeutic approach for DLBCL in older people varies somewhat due to age-related loss in organ function. A significant number of older individuals have many comorbidities that decrease their ability to withstand medical treatment. Multiple researchers have shown that the outcomes of conventional treatment in older individuals are similar to those in younger individuals. Therefore, it is not suitable to decrease the dosage of chemotherapy or choose for palliative care merely based on the patient’s age. Comprehensive geriatric assessment (CGA) is regarded as a potent instrument for evaluating a patient’s capacity to endure therapy and forecasting the likelihood of death and illness in patients with solid malignancies. While several researchers have indicated the efficacy of CGA and its impact on patients with DLBCL, these results still require additional verification.[11] Tuci et al.[12,13] and Marchesi et al.[14] reported that curative treatment failed to improve the outcome for patients classified as “unfit” by the CGA compared with palliative treatment. However, other reports reveal better results for a curative treatment than a palliative treatment.[11]
In this case, a 75-year-old female patient presented with a diagnosis of DLBCL (sinonasal) stage IE (Ann Arbor) and low intermediate risk (IPI score) with moderate frailty. As she falls within the category of very elderly,[15] a lump on the face causes the right eye to be unable to see. Hence, it is easy to lose balance and fall easily. Based on the IADLs, the patient is categorized as having moderate frailty. Based on the age category that is very elderly with moderate frailty, the choice of therapy that we choose for older adults who cannot tolerate the standard dose of R-CHOP-21 is treatment with R-mini-CHOP (rituximab 375 mg/m2, cyclophosphamide 400 mg/m2, doxorubicin 25 mg/m2, vincristine 1 mg on day 1 of each cycle, 40 mg/m2 prednisone on days 1–5).[16] R-mini-CHOP immunochemotherapy in this patient was given six times. The PET scan evaluation results only found nonmetabolic residual lymphoma in the subcutaneous fat maxillary left medial to a part of the left nasal; so it was categorized as a partial response (based on the Lugano classification). Therapy was continued with local external radiation therapy of 20 × 1.8 Gy. On physical examination after completing 20 cycles of radiation, there was no mass in the maxillary dextra; with the results of a nasopharyngeal MRI post-radiation evaluation, it was found that there was still a thickening of the cutis/subcutis in the left maxillary region to the left side of the nose due to inflammation; hence it was categorized as complete remission (based on the Lugano classification). On hematological examination, complete peripheral blood count, routine chemistry, and LDH were within normal limits.
There is limited research data regarding treating elderly DLBCL patients, whereby R-mini-CHOP can cure some patients. A multicenter study reported outcomes after six cycles of R-mini-CHOP in 150 patients > 80 years of age with DLBCL (75% stage III or IV). Obtained OS and two-year PFS are 59 and 47, respectively.[17]
CONCLUSION
We report a case of diffused large B-cell lymphoma in an elderly patient with moderate frailty. The therapeutic approach uses chemoimmunotherapy and radiation, with chemoimmunotherapy using the R-mini-CHOP regimen for six cycles followed by 20 × 1.8 Gy of radiation with the results of a complete remission (CR) evaluation.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Diffuse large B-cell lymphoma. 2022. [accessed 2024 May 21]. https://www.dynamed.com/condition/diffuse-large-b-cell-lymphoma.
- Epidemiology, clinical manifestations, pathologic features, and diagnosis of diffuse large B cell lymphoma. 2022. [accessed 2024 May 21]. https://www.uptodate.com/contents/epidemiology-clinical-manifestations-pathologic-features-and-diagnosis-of-diffuse-large-b-cell-lymphoma?
- How I treat elderly patients with diffuse large B-cell lymphoma. Blood. 2010;116:5103-10.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathologic study of non-Hodgkin lymphoma in sinonasal and hard palate regions in 15 Japanese cases. ORL J Otorhinolaryngol Relat Spec. 2005;67:23-9.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative population based analysis of sinonasal diffuse large B-cell and extranodal NK/T-cell lymphomas. Laryngoscope. 2015;125:1077-83.
- [CrossRef] [PubMed] [Google Scholar]
- CHOP-like chemotherapy with or without rituximab in young patients with good-prognosis diffuse large-B-cell lymphoma: 6-year results of an open-label randomised study of the mab thera international trial (MInT) Group. Lancet Oncol. 2011;12:1013.
- [CrossRef] [PubMed] [Google Scholar]
- Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: A phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet. 2013;381:1817.
- [CrossRef] [PubMed] [Google Scholar]
- Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol. 2006;24:3121.
- [CrossRef] [PubMed] [Google Scholar]
- CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:235.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of aggressive non-Hodgkin’s lymphoma in frail patients: Cardiac comorbidities and advanced age. Future Oncol. 2019;5:1197-205.
- [CrossRef] [PubMed] [Google Scholar]
- Can frailty screening tools predict completion of chemotherapy and chemotherapy toxicity in patients with thoracic malignancy? Journal of Geriatric Oncology.. 2020;914:1-3.
- [CrossRef] [Google Scholar]
- A comprehensive geriatric assessment is more effective than clinical judgment to identify elderly diffuse large cell lymphoma patients who benefit from aggressive therapy. Cancer. 2009;115:4547-53.
- [CrossRef] [PubMed] [Google Scholar]
- Comprehensive geriatric assessment is an essential tool to support treatment decisions in elderly patients with diffuse large B-cell lymphoma: a prospective multicenter evaluation in 173 patients by the Lymphoma Italian Foundation (FIL) Leuk Lymphoma. 2015;56:921-6.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective study on 73 elderly patients (≥75 yr) with aggressive B-cell non Hodgkin lymphoma: clinical significance of treatment intensity and comprehensive geriatric assessment. J Geriatr Oncol. 2013;4:242-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diffuse large B-cell lymphoma in adults aged 75 years and older: a single institution analysis of cause-specific survival and prognostic factors. Therapeutic Advances in Hematology. 2015;4(6):349-53.
- [CrossRef] [PubMed] [Google Scholar]
- Attenuated immunochemotherapy regimen (R-miniCHOP) in elderly patients older than 80 years with diffuse large B-cell lymphoma: a multicentre, single-arm, phase 2 trial. Lancet Oncol 2011.. 2011;12(5):460.
- [CrossRef] [Google Scholar]
- Initial treatment of advanced stage diffuse large B cell lymphoma [Internet]. 2022. Available from: https://www.uptodate.com/contents/initial-treatment-of-advanced-stage-diffuse-large-b-cell-lymphoma?







