Translate this page into:
Leiomyosarcoma of tongue: A case report and review of literature
Address for correspondence: Dr. Mranalini Verma, Department of Radiotherapy, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow - 226 014, Uttar Pradesh, India. shilpisinghal2003@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Leiomyosarcoma (LMS) of the tongue is an extremely rare mesenchymal tumor. Till now, we came across about 24 cases of tongue LMS reported in the literature. Here, we are presenting the case of a 50-year-old female with 4 months history of ulcerative growth on the tongue along with difficulty in swallowing and tongue movement who was diagnosed with LMS of the tongue on histopathology. He was managed with surgical excision followed by radiotherapy without any recurrence or metastasis after 6 months of follow-up.
Keywords
Carcinoma
leiomyosarcoma
tongue
Introduction
Leiomyosarcoma (LMS) is malignant neoplasm originating from smooth muscle account for 3–7% of soft tissue sarcomas which occurs frequently in uterine myometrium, gastrointestinal tract, retroperitoneum, skin, and subcutaneous tissue,1 but rare in the oral cavity because of paucity of smooth muscle in that site, but when present they are usually localized on the tongue, lips, and palate.2 It may arise as primary, radiation-associated, or metastatic tumor.3 Primary LMS of the tongue is an exceedingly rare. Here, we describe a case of LMS of the tongue in a 50-year-old female.
Case Report
We present the case of a 50-year-old female with an LMS of the tongue. She had reported to Oncosurgery Department with the complaint of ulcerative growth on the tongue along with difficulty in closing mouth and tongue movement for the last 4 months. She was tobacco-chewer for last 20 years with no other addiction history. She denies any exposure to chemicals, drugs, and sharp tooth. Her family history was also not significant. Her vital parameters were within normal range that she was conscious, alert, with blood pressure of 120/70 mm Hg, respiratory rate of 20/min, pulse rate of 110/min, and oxygen saturation of 92% on room air and her systemic evaluation was unremarkable. On local examination, she had a large ulcerative growth (size ∼ 5 cm × 5 cm) arising from the right anterolateral aspect of anterior tongue. Computed tomography scan imaging showed heterogeneously enhancing mass of size 4.5 cm × 3.5 cm × 5.4 cm on right anterolateral aspect of anterior tongue along with loss of fat interface between the mass and underlying intrinsic muscles of tongue Figure 1. Biopsy of mass lesion revealed a malignant epithelial neoplasm and immunohistochemistry (positive for alpha smooth muscle actin and desmin, and negative for cytokeratin and S-100) are suggestive of LMS. Then, she was hospitalized and underwent wide excision right side glossectomy with Type II modified radical neck dissection. The definitive histopathological diagnosis performed on surgical specimen revealed LMS of tongue with absence of neoplastic infiltration of surgical resection margin and all 14 lymph nodes; results of immunohistochemical study were positive for alpha-smooth muscle actin and desmin, negative for cytokeratin and S-100 protein further re-enforces the same diagnosis.
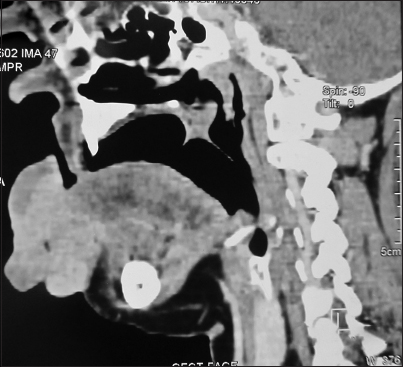
- Compute tomography scan showing heterogeneously enhancing mass of size 4.5 cm × 3.5 cm × 5.4 cm on right anterolateral aspect of anterior tongue along with loss of fat interface between mass and underlying intrinsic muscles of tongue
In view of tumor depth of 3 cm and tumor size more than 5 cm, patient was for postoperative radiotherapy with a dose of 60 Gy/30 fractions/6 weeks with X-6MV on a linear accelerator without concomitant chemotherapy.
Discussion
LMS is an uncommon malignant mesenchymal neoplasm originating from smooth muscle. It occurs frequently in the gastrointestinal tract and female genital tract.1 Due to paucity of smooth muscle in head and neck region, only 3–7% of LMS cases occur in head and neck region.1 However, when present in head and neck region, they are usually localized on the tongue, lips, and palate.2 The cause of LMS is still uncertain, although association with trauma, estrogen therapy, ionizing radiation, and Epstein–Barr virus has been documented in the literature.4
Clinically, LMS often presents as a rapidly growing, painless, discrete mass firmly adherent to surrounding soft tissue.4 LMS become large by the time diagnosis is confirmed because of very few associated symptoms.4 Due to nonspecific clinical presentation, diagnosis of LMS is based primarily on pathologic criteria. Immunohistochemistry or electron microscopy must be carried out to achieve more specific differential diagnosis.5,6 The histological criteria include the presence of pleomorphism, bizarre cell forms, pattern of interlacing bundles of smooth muscle cells, and high mitotic rate.7 Immunohistochemical study of LMS was consistently positive for alpha smooth muscle actin, vimentin, desmin, and negative for S-100 protein and cytokeratins.8,9
The only effective treatment is complete resection with sufficient tumor-free borders and postoperative radiotherapy when necessary.10 Radical neck dissection is needed in cases with lymphadenopathy. However, there is insufficient evidence to support the efficacy of radiotherapy and chemotherapy. Till now, only one case was reported who was treated with radiotherapy alone because of surgically inoperable condition.9 In this case, no local recurrence or distant metastasis was reported after 1.5 years of follow-up. In another two cases, radiotherapy at a dosage of 65 Gy/28 fractions/3 months was used after surgical excision.9,11 Chemotherapy was recommended in cases with inoperable and metastatic disease.12 A combination of ifosfamide and doxorubicin was used in one case.7 However, further research is needed to document the efficacy of adjuvant therapy in LMS of tongue. Prognosis of tongue LMS is good if clear surgical margin is achieved after excision.
Till now, we only know of 34 cases reported (including our patient’s case) of primary LMS of the tongue with four cases from India11,13,14 including one of the authors Table 1. Review of 34 cases revealed that there were 18 males and 16 females with an age range from 1 year to 97 years with no predilection for any specific age group. The sites of tumor lesions in the tongue include the tip, the lateral border, and the base. In 93% (24/26) patients, excision is the main treatment.
|
Year |
Location |
Age (years)/sex |
Treatment |
|---|---|---|---|
|
188415 |
Tongue |
33/male |
- |
|
19051 |
Tongue |
44/male |
- |
|
193817 |
Tongue |
50/male |
- |
|
193817 |
Base of tongue |
29/female |
- |
|
194418 |
Base of tongue |
32/male |
- |
|
196219 |
Tip of tongue |
1/male |
Excision |
|
196520 |
Tip of tongue |
43/male |
- |
|
196921 |
Dorsum of tongue |
11/female |
Excision |
|
197022 |
Tip of tongue |
54/male |
Excision |
|
198623 |
Base of tongue |
2.5/male |
Excision and chemotherapy |
|
199324 |
Margin of tongue |
48/female |
Excision |
|
19949 |
Base of tongue |
70/male |
Radiation therapy |
|
199425 |
Tip of tongue |
60/male |
Excision |
|
19958 |
Lateral border of tongue |
80/female |
Patient refused treatment |
|
199613 |
Base of tongue |
22/male |
Excision |
|
199816 |
Lateral border of tongue |
57/male |
Excision and radiotherapy |
|
200026 |
Tongue |
15/female |
Excision and chemotherapy |
|
200027 |
Lateral border of tongue |
67/male |
Excision |
|
199929 |
Margin of tongue |
42/male |
- |
|
200328 |
Lateral border of tongue |
62/female |
Excision |
|
200529 |
Tip of tongue |
67/male |
Excision |
|
200530 |
Lateral border of tongue |
32/male |
Excision and chemotherapy |
|
200631 |
Lateral border of tongue |
57/female |
Excision |
|
200632 |
Tip of tongue |
54/female |
Excision |
|
200633 |
Lateral border of tongue |
52/female |
Excision |
|
200710 |
Tongue |
79/female |
Excision |
|
200734 |
Tongue |
97/female |
Excision |
|
200834 |
Lateral border of tongue |
46/female |
Excision |
|
201035 |
Lateral border of tongue |
55/male |
Excision |
|
201414 |
Lateral border of tongue |
35/male |
Excision |
|
20121 |
Base of tongue |
77/male |
Excision |
|
20127 |
Tongue |
54/female |
Chemotherapy |
|
201411 |
Base of tongue |
38/female |
Excision and radiotherapy |
|
2015 |
Tongue (our case) |
50/female |
Excision |
This case report highlights that although LMS of the tongue is a rare mesenchymal tumor, we should be familiar with this unusual lesions because early diagnosis and aggressive management are the mainstay of therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Leiomyosarcoma of the base of the tongue and free edge of the epiglottis: A case report. J Med Case Rep. 2012;6:400.
- [Google Scholar]
- Oral leiomyoma in retromolar trigone. A case reportMed Oral Patol Oral Cir Bucal. 2007;12:E53-5.
- [Google Scholar]
- Leiomyosarcomas of the oral cavity: Report of a radiation-associated and a metastatic case. Oral Maxillofac Surg. 2012;16:227-32.
- [Google Scholar]
- Leiomyosarcomas of the oral cavity. Report of four cases and review of the literatureJ Craniomaxillofac Surg. 1993;21:342-7.
- [Google Scholar]
- Leiomyosarcoma of the external soft tissues. A clinicopathologic, immunohistochemical, and electron microscopic studyCancer. 1986;57:2077-88.
- [Google Scholar]
- Poorly differentiated leiomyosarcoma of the maxillary sinus: A histological, immunohistochemical and ultra-structural study. J Clin Electron Microsc. 1987;20:219-27.
- [Google Scholar]
- Leiomyosarcoma of the tongue with multiple metastases: A case report and review of literature. J Oral Maxillofac Surg. 2012;70:1745-50.
- [Google Scholar]
- Leiomyosarcoma of the tongue: A case report. J Oral Maxillofac Surg. 1995;53:M698-701.
- [Google Scholar]
- Leiomyosarcoma of the base of the tongue treated with radiotherapy: A case report. Eur J Cancer B Oral Oncol. 1994;30B:351-5.
- [Google Scholar]
- Primary oral leiomyosarcoma: A clinico-pathologic study and analysis of prognostic factors. Int J Oral Maxillofac Surg. 2007;36:409-16.
- [Google Scholar]
- Leiomyosarcoma of the base of tongue. Indian J Otolaryngol Head Neck Surg. 1996;48:235-7.
- [Google Scholar]
- Primary leiomyosarcoma of tongue: A rare neoplasm. J Evol Med Dent Sci. 2014;3:473-8.
- [Google Scholar]
- Leiomyosarcomas in childhood: A clinical and pathologic study of 10 cases. Pediatr Pathol. 1986;6:181-97.
- [Google Scholar]
- Leiomyosarcomas of the oral cavity: An unusual topographic subset easily mistaken for nonmesenchymal tumours. Histopathology. 2000;36:210-20.
- [Google Scholar]
- Primary intraoral leiomyosarcoma of the tongue: An immunohistochemical study and review of the literature. Oral Oncol. 2000;36:519-24.
- [Google Scholar]
- Metastatic leiomyosarcoma to the tongue. Otolaryngol Head Neck Surg. 2003;128:601-2.
- [Google Scholar]
- Leiomyosarcoma of the tongue: A case report. Clin J Oral Maxillofac Surg. 2006;17:109-16.
- [Google Scholar]
- A peculiar site of leiomyosarcoma: The tongue tip – Report of a case. Int J Oral Maxillofac Surg. 2006;35:469-71.
- [Google Scholar]
- Primary leiomyosarcoma of the oral tongue: Magnetic resonance and ultrasonography findings with histopathologic correlation. Acta Radiol. 2006;47:514-7.
- [Google Scholar]
- Leiomyosarcoma of the tongue: A case report. Br J Oral Maxillofac Surg. 2008;46:e69-70.
- [Google Scholar]
- A primary leiomyosarcoma of the lateral border of the tongue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e31-3.
- [Google Scholar]







