Translate this page into:
The diagnostic significance of breast incidentalomas detected on whole-body fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography
Address for correspondence: Dr. Shelly Sharma2164, Block B/2, Vasant Kunj, New Delhi - 110 070, India. raddocss@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective: The objective of this study was to establish the diagnostic significance of breast incidentalomas detected on whole-body fluorine-18 (18F) fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT).
Materials and Methods: We retrospectively analyzed the data of 3868 patients who underwent 18F FDG PET/CT at our institution, for the presence of hypermetabolic focus in the breasts. Patients with known breast cancer or with the previous history of breast cancer were excluded from the study. Ten out of remaining 3868 patients had abnormal focal uptake in the breast. We, therefore, enrolled these 10 patients with histopathology confirmation in this study.
Results: Among all 3868 patients, 10 (0.25%) patients demonstrated incidental focal uptake in breast parenchyma. All of these 10 patients were females. Histopathology examination confirmed malignancy in 8 out of 10 patients (80%), these included invasive ductal cancer in 4 patients, non-Hodgkin's lymphoma in 2 patients, and metastasis from rectal cancer and endometrial cancer, respectively, in 2 patients. Of the 10 patients, 2 (20%) had lesions that were confirmed to be benign. Both of these were proven to be fibroadenomas. The mean maximum standardized uptake value (SUVmax) on FDG-PET/CT scans was 1.35 ± 1.2 in the benign cases versus 3.8 ± 1.83 in the malignant cases. This difference was statistically insignificant (P = 0.056). All malignant lesions had SUVmax 2.0 or greater. The mean size differed significantly between the benign and malignant groups (2.55 ± 0.63 vs. 1.31 ± 0.44 cm) (P = 0.005) with benign lesions being bigger in size.
Conclusion: Unexpected focal areas of hypermetabolic activity discovered in the breast at the time of PET/CT are associated with a high likelihood of malignancy in as many as 80% of cases. Therefore, any suspicious activity discovered in the breast on PET/CT should be evaluated until a diagnosis is found.
Keywords
Breast cancer
breast incidentaloma
breast lymphoma
breast metastases
positron emission tomography/computed tomography
Introduction
Positron emission tomography (PET) with fluorine-18 (18F) fluorodeoxyglucose (FDG) is widely used in oncology for diagnosis and staging of tumors and for monitoring the therapeutic response. Apart from providing metabolic information, these images provide good anatomic details as well. The widespread use of PET/computed tomography (CT) has increased the level of detection of incidental hypermetabolic foci unrelated to the known malignancy. The increased uptake may be associated with physiological or benign processes or due to the presence of additional primary or secondary malignancies.1 The overall prevalence, by PET/CT, of incidental malignancies and premalignant pathology has been reported across literature to be 1.2–1.7%; the most common sites involved being colon, thyroid, lung, and breast.2,3,4 These incidentally detected foci showing increased FDG uptake on PET/CT can significantly impact patient outcome.
In women undergoing PET/CT for nonbreast malignancies, the incidence of unexpected increased 18F-FDG activity within the breast tissue ranged from 0.36% to 6.3% and malignancy in these incidental hypermetabolic breast lesions ranged from 37.5% to 83%.5,6,7,8 These studies demonstrated that incidental 18F-FDG–avid lesions in the breast have a high incidence of malignancy and, therefore, need to have an appropriate evaluation. However, there are no clear-cut guidelines on evaluation of these lesions and often pose a diagnostic dilemma.
In this study, we retrospectively reviewed all the cases with incidentally detected focal breast lesions on PET/CT, who underwent PET/CT scan for nonbreast malignancies. In addition to performing quantitative analysis of the FDG uptake in the form of maximum standardized uptake value (SUVmax), we also investigated whether noncontrast CT findings and mammography findings were helpful in characterizing these focal breast lesions.
Materials and Methods
Subjects
The study was performed in accordance with the regulations of the Institutional Review Board at our hospital, which approved this retrospective study and waived the requirement for patient informed consent. All patients who underwent 18F-FDG PET/CT scan between October 2012 and June 2013 at our institute were retrospectively analyzed. Patients with a known history of breast cancer and those with known breast lesions were excluded. Ten out of remaining 3868 patients had abnormal focal uptake in the breast. All these 10 patients had histopathology confirmation and were included in this study.
PET/CT-standard procedures for patient preparation and PET/CT acquisition were followed. Patients were instructed to fast and not consume anything, except for water, for at least 4 h before the administration of 18F-FDG. Intravenous fluids containing dextrose were withheld for 4–6 h before tracer administration. Patients were administered 8–10 mCi of 18F-FDG intravenously provided blood glucose levels were <150 mg/dl. They were instructed to remain seated or recumbent after 18F-FDG administration to avoid muscular uptake.
Image acquisition was done using Biograph 40 LSO advanced PET/CT scanner (Siemens, Knoxville, TN, USA). The system consists of a 40-slice, spiral CT (Siemens Somatom Emotion) and is optimized for use in whole-body oncology. Data were obtained in three-dimensional mode, with attenuation correction calculated from co-registered CT images. The PET/CT scanner was subjected to daily quality control evaluation before the start of acquisition. Images were acquired 60 min after 18F-FDG administration from skull base to mid-thigh (a transmission scan using CT followed by 2 min per bed emission scan).
Image analysis
All 18F FDG PET/CT scan images were interpreted by two experienced nuclear medicine physicians and a radiologist. Because of the physiologic distribution of FDG, uptake areas were identified as abnormal if the accumulation of FDG was focal and greater than in the background breast tissue. FDG uptake was measured in a semi-quantitative manner as SUVmax corrected for body weight. The SUV is the decay-corrected ratio between the measured uptake in a region of interest, and the expected uptake if 18F-FDG were distributed evenly throughout the body. A circular region of interest was placed over the region of highest intensity in the breast lesion, and uptake was automatically quantified as SUVmax.
Ultrasound and mammography
An experienced radiologist later on performed a sonographic examination and the mammographic interpretation. All patients underwent breast sonography after PET/CT. Breast sonographic examination was performed with 7.5 MHz probe (Sonosite Micromaxx). Mammographic examinations were performed in 6/10 patients on full field digital mammography unit (Selenia, Hologic).
Results
Among all 3868 patients, 10 (0.25%) patients demonstrated incidental focal uptake in breast parenchyma. All of these 10 patients were females. None of these patients was a known case of carcinoma breast or any other breast pathology and were being evaluated for other malignancies. The mean age was 46 ± 7 (standard deviation [SD]) years in the group with benign lesions and 58.8 ± 14.8 (SD) years in the group with malignant lesions. This difference was statistically insignificant according to results of the Student's t-test (P = 0.1242). The mean SUVmax on FDG-PET/CT scans was 1.35 ± 1.2 in the benign cases versus 3.8 ± 1.83 in the malignant cases Figure 1. This difference was statistically insignificant (P = 0.056). All malignant lesions had SUVmax 2.0 or greater. The mean size differed significantly between the benign and malignant groups (2.55 ± 0.63 vs. 1.31 ± 0.44 cm) (P = 0.005) with benign lesions being bigger in size Table 1. Histopathological examination confirmed malignancy in 8 out of 10 patients (80%). Histopathological examination of specimens from these 8 patients revealed invasive ductal cancer in 4 patients, non-Hodgkin's lymphoma (NHL) in 2 patients, and metastasis from rectal cancer and endometrial cancer, respectively, in 2 patients. Of the 10 patients, 2 (20%) had lesions that were confirmed to be benign and follow-up FDG PET/CT, and sonography showed no change Figure 2. Both of these were proven to be fibroadenomas.
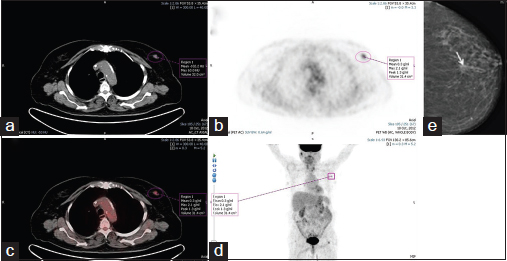
- A 75-year-old woman (patient 1 in Table 1) with infiltrating ductal carcinoma was being evaluated for carcinoma of the ovary. (a) Computed tomography portion of fluorodeoxyglucose positron emission tomography/computed tomography shows a soft tissue lesion (measures 1.7 cm × 1 cm) with irregular margins. (b) Axial positron emission tomography image shows focal area of increased metabolism (maximum standardized uptake value = 2.1) in the left breast, lateral to midline. (c) Positron emission tomography/computed tomography fused images and (d) positron emission tomography maximum intensity projection image. (e) Mammogram shows a soft tissue lesion (arrow) with spiculated margins corresponding to positron emission tomography/computed tomography abnormality
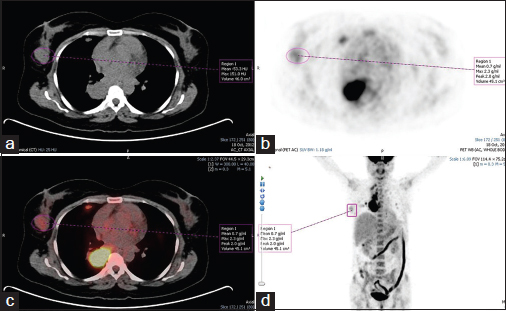
- A 41-year-old woman (patient 2 in Table 1) with right breast fibroadenoma was being evaluated for carcinoma of the lung. (a) Computed tomography portion of fluorodeoxyglucose positron emission tomography/computed tomography shows a soft tissue lesion (measures 3.0 cm × 1.6 cm) in the outer quadrant with well-defined margins. (b) Axial positron emission tomography image shows focal area of increased metabolism (maximum standardized uptake value = 2.3) in the right breast, outer quadrant. (c) Positron emission tomography/computed tomography fused image and (d) positron emission tomography-maximum intensity projection image
|
Underlying malignancy |
Age |
Size |
Breast lesion histopathology |
SUVmax |
|---|---|---|---|---|
|
Ovary |
75 |
1.7 |
Malignant |
2.0 |
|
Lung |
41 |
3 |
Benign |
2.2 |
|
NHL (DLBCL) |
50 |
1 |
Malignant |
3.1 |
|
Rectum |
29 |
0.9 |
Malignant |
3.3 |
|
Ovary |
64 |
1 |
Malignant |
2.8 |
|
NHL |
74 |
0.8 |
Malignant |
6.4 |
|
Endometrium |
66 |
1.4 |
Malignant |
6.6 |
|
Periampullary |
56 |
1.7 |
Malignant |
2 |
|
Multiple myeloma |
57 |
2 |
Malignant |
4.4 |
|
Gall bladder |
51 |
2.1 |
Benign |
0.5 |
SUV - Standardized uptake values; DLBCL - Diffuse large B-cell lymphoma; NHL - Non-Hodgkin's lymphoma
Breast nodules were detected in the noncontrast CT portion of PET/CT in 9/10 cases. Of these, only two cases had irregular margins indicating high suspicion of malignancy. Both these cases were confirmed to be malignant. Rest of the nodules had well-defined or lobulated margins. In 1/10 patients, the lesion was not detected on noncontrast CT portion and showed diffuse FDG uptake in the lower inner quadrant of right breast Figure 3. Mammography was not available in all cases. Out of eight patients with malignant lesions, mammograms were available in six patients. The lesions were detected on mammography in 4/6 patients. All of these patients had Breast Imaging-Reporting and Data System (BI-RADS) mammography Category IV or greater. In 2/6 patients, the lesions were not detected on mammography due to dense breast parenchyma Table 2.
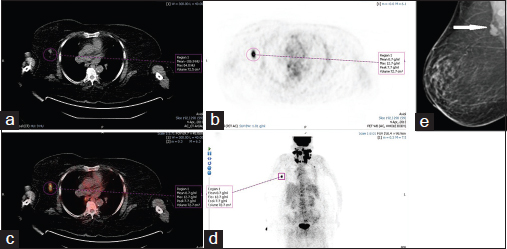
- A 74-year-old woman (patient 6 in Table 1) with non-Hodgkin's lymphoma breast was being evaluated for non-Hodgkin's lymphoma of head and neck region. (a) Computed tomography portion of fluorodeoxyglucose positron emission tomography/computed tomography shows a soft tissue lesion (measuring 0.8 cm) with regular margins. (b) Axial positron emission tomography image shows a hypermetabolic soft tissue nodule in right breast lower outer quadrant (maximum standardized uptake value = 12.7). (c) Fused positron emission tomography/computed tomography images and (d) positron emission tomography-maximum intensity projection image. (e) Mammogram shows heterogeneously dense breast parenchyma with axillary lymph nodes (arrow)
|
Breast lesion histopathology |
Detected on CT scan |
Margins on CT scan |
|---|---|---|
|
IDC |
Yes |
Irregular |
|
NHL |
Not detected |
- |
|
Metastatic |
Yes |
Smooth |
|
IDC |
Yes |
Irregular |
|
NHL |
Yes |
Regular |
|
Metastatic |
Yes |
Regular |
|
IDC |
Yes |
Lobulated |
|
IDC |
Yes |
Lobulated |
NHL - Non-Hodgkin's lymphoma; CT - Computed tomography; IDC - Invasive ductal carcinoma
Discussion
In this study, 10 (0.25%) subjects demonstrated incidental focal uptake in the breast at FDG PET/CT. All of these patients were females. Eight of the 10 patients in the study were found to have malignant lesions. Thus, the frequency of malignancy was 80%. Previously published reports have shown variable rates of malignancy in these incidental foci ranging between 37% and 83%.5,6,7,8 Our results matched with those reported by Korn et al. in a previously published similar study.7
In this study, we examined parameters that would be useful for differentiating the benign and malignant properties of incidentally identified FDG-avid foci in breasts. The malignant lesions were more common among older patients, but the difference between the two groups was not statistically significant (P = 0.12).
Second, all the malignant lesions had SUVmax 2.0 or greater and benign lesions showed low mean SUVmax. Similar studies in the past have found that SUVmax can assist in differentiating between benign and malignant lesions.8,9,10 Kang et al.8 reported statistically significant difference in malignancy rate between the groups with SUVmax >2.0 and <2.0. Our study did not find any statistical difference in SUVmax between benign and malignant lesions (P = 0.058), but mean SUVmax in malignant lesions was higher than in benign lesions.
Third, the malignant lesions were smaller in size than the benign lesions. The difference between the two was statistically significant (P = 0.005). Chae et al.10 in a similar study had found a statistically significant difference between the size of benign and malignant lesions with the diameter of malignant lesions being greater than that of benign lesions.
In this study, we excluded patients with previously known breast lesions and those with a history of breast cancer. Invasive ductal carcinoma (IDC) was the most common malignancy we encountered in this study (four of eight cases), and there were no cases of invasive lobular carcinoma. Invasive lobular carcinoma is reported to have a lower degree of FDG uptake than invasive ductal cancer and hence produces false negative results more often than IDCs at FDG PET/CT.11,12
In 2/8 cases, there was extranodal involvement of breast by NHL. The SUVmax was >2 in both these cases. Almost any organ can be affected by lymphoma, with the most common extranodal sites of involvement being the stomach, spleen, waldeyer ring, central nervous system, lung, bone, and skin.13 Breast lymphoma is a rare disease representing 0.04–0.5% of malignant breast tumors and is almost always of non-Hodgkin's type.14 The breast involvement by lymphoma can be subtle and may be overlooked during CT. PET/CT has evolved into an important imaging tool for evaluation of lymphomas, facilitating the detection of affected extranodal sites even when CT shows subtle or no obvious lesions.15
In 2/8 cases, there were metastases to the breast from known primary sites. Initially, these lesions were presumed to be primary breast malignancies; however, immunohistochemical studies confirmed them to be metastasis from rectal and endometrial cancer, respectively. Hematogenous spread of metastases to the breast is rare with the most common malignancies to metastasize to the breast being melanoma, sarcoma, and tumors of the lung and ovary.16,17 The differentiation between a primary breast cancer and a metastatic lesion on the basis of imaging characteristics can be difficult. Patients with metastatic disease to the breast usually present with one or more discrete, well-circumscribed nodules that may be similar to benign nodules. Internal calcifications are rare in metastatic nodules, except in the case of metastatic ovarian carcinoma, in which the calcifications represent psammoma bodies.16 In addition, spiculation is uncommon because of the absence of desmoplasia in these lesions.17 In both our cases, the lesions had smooth margins with no associated micro calcifications.
The noncontrast CT portion of PET/CT detected 9/10 lesions. The characteristic imaging features of malignancy were present in only 2/8 malignant lesions. Six of these eight patients with confirmed malignancy underwent concomitant mammography, and mass lesions were detected in four of these six cases. All of these four patients had mammography BI-RADS Category IV or higher. Thus, we did not find these modalities helpful in characterizing these lesions into benign or malignant categories.
However, all the lesions (10/10) were identified on ultrasound which was also used as a guide for tissue sampling. The specificity of mammography was found to be lower than that of sonography; the reason for this can be dense breast parenchyma and also the smaller size of these lesions.18 Ultrasound is an easily available modality and can be used as an adjunct to PET/CT for evaluation and characterization of these lesions.
Our study revealed that incidental focal breast uptake of SUVmax 2.0 or greater is significant and requires further evaluation. However, the need for further workup should be determined by clinical judgment and extent of primary disease. Beatty et al.2 prospectively acquired a database of patients with a known malignancy that underwent PET/CT for staging or serial imaging. They concluded that incidental PET/CT findings should be investigated when the results will impact treatment.
The limitations of this study are its retrospective nature and a small study group.
Conclusion
Unexpected focal areas of hypermetabolic activity discovered in the breast at the time of PET/CT are associated with a high likelihood of malignancy in as many as 80% of cases. Therefore, any suspicious activity discovered in the breast on PET/CT should be evaluated until a diagnosis is found.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- AJR teaching file: Incidental breast cancer detected with 18F-FDG PET/CT. AJR Am J Roentgenol. 2011;196(06):WS83-5. Suppl:
- [Google Scholar]
- Incidental PET/CT findings in the cancer patient: How should they be managed? Surgery. 2009;146:274-81.
- [Google Scholar]
- Detection of unexpected additional primary malignancies with PET/CT. J Nucl Med. 2005;46:752-7.
- [Google Scholar]
- Detection of clinically unexpected malignant and premalignant tumors with whole-body FDG PET: Histopathologic comparison. Radiology. 2004;230:417-22.
- [Google Scholar]
- The predictive value of incidental PET/CT findings suspicious for breast cancer in women with non-breast malignancies. Am J Surg. 2009;198:495-9.
- [Google Scholar]
- Unexpected foci of 18F-FDG uptake in the breast detected by PET/CT: Incidence and clinical significance. Eur J Nucl Med Mol Imaging. 2009;36:1558-64.
- [Google Scholar]
- Unexpected focal hypermetabolic activity in the breast: Significance in patients undergoing 18F-FDG PET/CT. AJR Am J Roentgenol. 2006;187:81-5.
- [Google Scholar]
- Clinical significance of incidental finding of focal activity in the breast at 18F-FDG PET/CT. AJR Am J Roentgenol. 2011;197:341-7.
- [Google Scholar]
- The role of the breast radiologist in evaluation of breast incidentalomas detected on 18-fludeoxyglucose positron emission tomography/CT. Br J Radiol. 2013;86:20130034.
- [Google Scholar]
- Analysis of incidental focal hypermetabolic uptake in the breast as detected by 18F-FDG PET/CT: Clinical significance and differential diagnosis. Acta Radiol. 2012;53:530-5.
- [Google Scholar]
- F-18 fluorodeoxyglucose-positron emission tomography imaging for primary breast cancer and loco-regional staging. Radiol Clin North Am. 2007;45:645-57. vi.
- [Google Scholar]
- FDG uptake in breast cancer: Correlation with biological and clinical prognostic parameters. Eur J Nucl Med Mol Imaging. 2002;29:1317-23.
- [Google Scholar]
- FDG PET/CT of extranodal involvement in non-Hodgkin lymphoma and Hodgkin disease. Radiographics. 2010;30:269-91.
- [Google Scholar]
- Primary lymphoma of the breast involving both axillae with bilateral breast carcinoma. World J Surg Oncol. 2008;6:52.
- [Google Scholar]
- Occult cancer in women with dense breasts: Detection with screening US – Diagnostic yield and tumor characteristics. Radiology. 1998;207:191-9.
- [Google Scholar]







