Translate this page into:
Radio-pathological correlation of mycosis fungoides
Address for correspondence: Dr. Reddy Ravikanth, Department of Radiology, Malabar Medical College, Kozhikode - 673 315, Kerala, India. ravikanthreddy06@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Dear Sir,
A 52-year-old male presented to the dermatology department on account of itching for 3 years and mild hypoanesthesia of the skin for 5 years in the region of the gluteal cleft and right thigh anteriorly. Viral screens for HIV I and II, Hepatitis B surface Ag, and Hepatitis C virus antibodies were also negative. Contrast computed tomography (CT) demonstrated tumorous nodular thickening of skin and subcutaneous fat of the gluteal cleft Figure 1a and anterior right thigh Figure 1b. On laboratory investigations, her hemoglobin was 7.5 g%, total leukocyte count was 8500/mm3, and platelet count was 240,000/mm3. Peripheral smear showed no atypical cells. There was no involvement of the bone marrow. FNAC of the skin lesions revealed features compatible with non-Hodgkin's lymphoma. Skin biopsy showed diffuse lymphoid infiltrate involving the full thickness of epidermis and extending to the subcutaneous dermis, more around the perivascular spaces Figure 2a. These lymphoid cells were atypical and large with convoluted nuclei. Histopathological diagnosis of mycosis fungoides-tumor stage was made. Immunohistochemistry showed CD3 Figure 2b, CD4, and leukocyte common antigen positivity. He was diagnosed in the early stages, stage 1B (T2 N0 M0 B0) according to the modified tumor-node-metastasis-blood classification. The patient was placed on topical glucocorticoids and commenced on eight courses of IV cyclophosphamide 750 mg/m2, IV epirubicin 25 mg/m2, and prednisolone tablets 40 mg/m2 daily for 5 days. Each course was given in 21-day intervals. He completed all courses of chemotherapy and did well, evidenced by disappearance of symptoms except for the dyspigmentation on the skin which is still resolving.
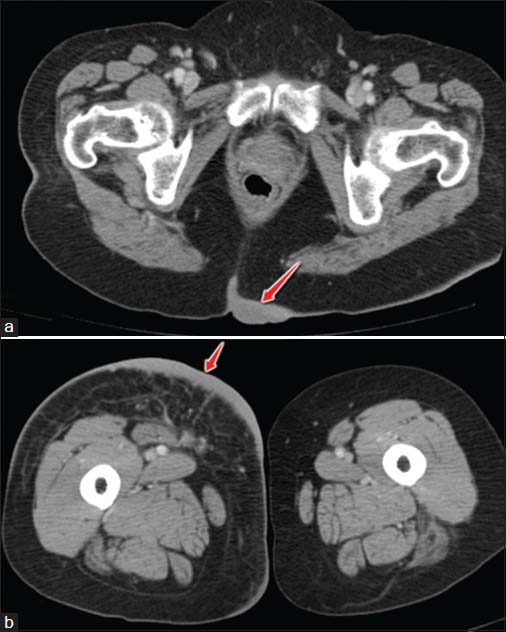
- (a) Axial contrast-enhanced computed tomography image showing tumorous nodular thickening of the skin and subcutaneous fat at the region of gluteal cleft (arrow). (b) Axial contrast-enhanced computed tomography image showing tumorous nodular thickening of the skin and subcutaneous fat of anteromedial right proximal thigh (arrow) extending posteriorly
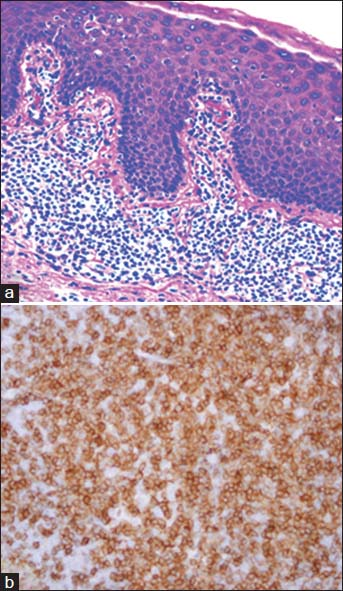
- (a): Histopathology of the skin biopsy showing epidermotropism with a dense band-like dermal infiltrate (H and E, ×200). (b) Immunohistochemistry image of the skin biopsy showing positivity for CD3 (×400)
Mycosis fungoides is a T-cell lymphoma and an uncommon form of extranodal NHL occurring most commonly in elderly men.1 Mycosis fungoides is the most common form of cutaneous T-cell lymphoma (CTCL);2 presents with chronic eczema; can progress to widespread visceral involvement; has a high recurrence rate with survival depending on the presence of nodal and systemic involvement; with low fludeoxyglucose (FDG) uptake. T-cell lymphomas are the most common (65% of cases), and B-cell lymphomas account for the remainder.3 Histopathology remains the reference standard for the diagnosis of skin malignancies. CTCL is usually polymorphous clinically, whereas cutaneous B-cell lymphoma is monomorphous. Imaging modalities such as CT, magnetic resonance imaging, and 18F-FDG positron emission tomography/CT are commonly used for staging, preoperative planning, and posttreatment assessment. Imaging findings can narrow down the differential diagnosis and elucidate their metastatic pattern.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The histological spectrum of early mycosis fungoides: A study of 58 Saudi Arab patients. Oman Med J. 2012;27:134-9.
- [Google Scholar]
- From inflammation to neoplasia: Mycosis fungoides evolves from reactive inflammatory conditions (lymphoid infiltrates) transforming into neoplastic plaques and tumors. Arch Dermatol. 2001;137:949-52.
- [Google Scholar]
- Early mycosis fungoides vs. inflammatory mimics: How reliable is histology? Indian J Dermatol Venereol Leprol. 2008;74:462-6.
- [Google Scholar]






