Translate this page into:
Mucinous adenocarcinoma of urachus: A tailored approach
Address for correspondence: Dr. Karthik K. Prasad230 Ganitha Bharathi 12B Cross, 1A Main WCR Mahalakshmipuram, Bengaluru - 560 086, Karnataka, India. drkrishkarthik@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Vesical adenocarcinomas are uncommon, accounting for less than 2% of all malignant urinary bladder tumors. Of these, urachal adenocarcinoma represents a rare subset. We report a case of a urachal adenocarcinoma, highlighting its unique features and management. A 50-year-old female presented with hematuria and burning micturition. Computed tomography scan showed a mass arising from an outpouching in the apex of bladder, suggestive of urachal origin. Biopsy revealed moderately differentiated mucinous adenocarcinoma. Partial cystectomy with ileocystoplasty, excision of urachus along with umbilicus and pelvic lymph node dissection was done. Histopathology confirmed urachal mucinous adenocarcinoma. The pathogenesis of urachal adenocarcinoma is unknown. It is important to distinguish between urachal and non urachal adenocarcinoma as the former carry a better prognosis. Management of urachal adenocarcinoma involves complete eradication of the disease. Stage and margin status have been identified as the most important predictors of long-term survival.
Keywords
Mucinous adenocarcinoma
partial cystectomy
urachus
vesical adenocarcinoma
Introduction
Urachal adenocarcinoma was first reported by Begg in 19301 and there are fewer than 350 cases reported in literature. It accounts for 0.35–0.7% of all bladder tumors. Currently, there is no consensus on the diagnostic criteria. The location of the tumor does not result in early symptoms and precludes a timely clinical diagnosis. Appropriate imaging and pathological examination can contribute to the diagnosis. Surgery remains the treatment of choice, but the postoperative risk of recurrence remains high.2 The role of adjuvant therapy needs to be elucidated by prospective clinical trials.
Case Report
A 50-year–old female presented with hematuria, burning micturition, and dull aching, lower abdomen pain since 2 years. Ultrasound of abdomen and pelvis showed heterogeneous mass arising from anterior wall of bladder with specks of calcification. Cystoscopy showed well circumscribed solid tumor 5 × 4 cm arising from the dome of the bladder with normal adjacent bladder mucosa. Transurethral biopsy histology showed moderately differentiated mucinous adenocarcinoma. Computed tomography (CT) scan of KUB showed lobulated enhancing mass measuring 5.1 × 4.3 × 2.7 cm arising from the outpouching of dome of the bladder with no perivesical spread Figure 1a. Other pelvic organs were unremarkable. Urachal adenocarcinoma was suspected and planned for surgical intervention.
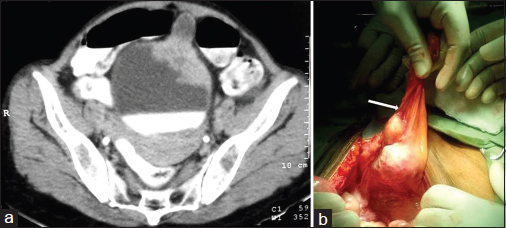
- (a) Computed tomography pelvis showing lobulated enhancing mass arising in an outpouching of bladder dome. (b) Tumor in bladder dome with urachus (arrow)
The patient underwent partial cystectomy, bladder augmentation with ileocystoplasty, bilateral pelvic lymph node dissection, and complete resection of urachus with umbilicus. Tumor was excised with adequate margins, which were reported negative on frozen section Figure 1b. Postoperatively patient recovered well with no urinary complaints.
Excised specimen revealed a grey white tumor arising from urachus infiltrating into bladder. Histopathological examination showed moderately differentiated mucinous adenocarcinoma infiltrating up to muscularis propria with lymph node metastasis (Stage III Mayo) Figure 2. Adjuvant radiotherapy was given. The patient is being followed-up with cystoscopy and imaging of chest, abdomen, and pelvis every 3 months.
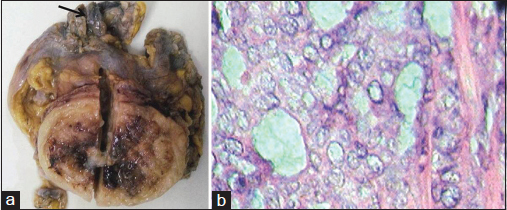
- (a) Partial cystectomy specimen with urachus (arrow) showing grey white glistening tumor invading the bladder cavity. (b) Tumor cells in glandular pattern with abundant extracellular mucin H and E ×400
Discussion
The urachus, or median umbilical ligament, is a midline tubular structure that extends from the anterior dome of the bladder toward the umbilicus. Urachal adenocarcinomas are rare tumors representing 0.01% of all bladder cancers, and 10% of all vesical adenocarcinoma. Although pathogenesis of urachal adenocarcinoma is unknown, intestinal metaplasia of the urachal epithelium is the favoured predisposing factor.
Most cases of urachal adenocarcinoma occur in the fifth and sixth decades of life with slight male preponderance. Hematuria is the most common symptom (71%), followed by pain and irritative symptoms (42%), mucosuria (25%), and umbilical discharge (2%).
Criteria to classify a tumor as urachal in origin were initially established by Wheeler and Hill, were modified by Johnson et al., who proposed the following criteria: (1) Tumor in the bladder dome, (2) a sharp demarcation between the tumor and the surface epithelium, and (3) exclusion of primary adenocarcinoma located elsewhere that has spread secondarily to the bladder.3
Ninety percent of urachal carcinomas arise in the juxtabladder portion of the urachus and extend toward umbilicus, invading the space of Retzius and inferiorly through the bladder wall. Ultrasonography allows localization of the tumor and detection of highly echogenic calcifications and solid components of the tumor in the anterior abdominal wall. On CT urachal carcinoma may be solid, cystic, or a combination of the two. Calcification occurs in 50%–70% of cases and may be punctate, or curvilinear and peripheral. Calcifications in a midline supra bladder mass are considered nearly diagnostic for urachal carcinoma. CT is not accurate in identifying microscopic invasion of fat and bladder wall.4
Grossly, the tumor exhibits a glistening appearance, reflecting its mucinous content. Urachal adenocarcinomas are subdivided into mucinous, enteric, signet ring-cell, and mixed types. Mucinous carcinomas are characterized by pools or lakes of extracellular mucin with single cells or nests of columnar or signet ring-cells floating in it. The cells stain for CK20, CEA and Leu-M1 and variably for CK7 and beta catenin. Although urachal adenocarcinoma has been staged using the TNM, Sheldon or Mayo staging systems, the Mayo system is preferred due to its simplicity.5
Differentiating urachal from non urachal adenocarcinoma and metastatic adenocarcinoma is important as urachal tumors have a better outcome.6 Immunohistochemistry does not unequivocally help in this distinction.
Treatment consists of radical or partial cystectomy with pelvic lymph node dissection, en bloc urachal resection with umbilicus. Laparoscopic partial cystectomy with lymphadenectomy has been reported as an alternative treatment but long-term follow-up is required in order to determine the effect of this treatment. The role of radiation and chemotherapy in the management of urachal carcinoma are unclear and must be individualized. Overall five year survival rate has been reported to range from 35% to 63%.7
Conclusion
Urachal carcinoma is a rare malignant tumor with characteristic clinico-radiological features. It is important to diagnose and differentiate urachal from non urachal adenocarcinoma due to the differences in management and outcome. Although there are no prospective clinical trials reported to date, large single institution reports suggest surgical resection with a partial cystectomy and en bloc resection of the urachal ligament with umbilicus as the treatment of choice in the setting of localized disease. The stage, margins and lymph node status have been identified as important predictors of long-term survival.8
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Options for diagnosis and treatment of urachal carcinoma. Asia Pac J Clin Oncol. 2013;9:117-22.
- [Google Scholar]
- Surgical and chemotherapeutic experience regarding a urachal carcinoma with repeated relapse: Case report and literature review. World J Surg Oncol. 2013;11:170.
- [Google Scholar]
- Primary adenocarcinoma of the urinary bladder. A clinicopathologic analysis of 72 casesCancer. 1991;67:2165-72.
- [Google Scholar]
- Urachal carcinoma: Clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer. 2006;107:712-20.
- [Google Scholar]
- Urachal adenocarcinoma: A clinician's guide for treatment. Semin Oncol. 2012;39:619-24.
- [Google Scholar]







