Translate this page into:
Maxillary metastasis from carcinoma lung: An unusual presentation
Address for correspondence: Dr. Niharika Bisht, Department of Radiation Oncology, Malignant Disease treatment Centre, Command Hospital (SC), Wanowrie, Pune, Maharashtra, India. niharikabisht@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Lung cancer is one of the most common cancers in the world affecting both men and woman. Common site of metastasis includes liver, adrenals, bone, and brain. Metastasis to the maxilla is very rare with only a few cases being reported so far. Here, we present a case of a 32-year-old male where metastatic lesion was discovered before primary tumor.
Keywords
Non-small cell lung cancer
metastasis
mediastinal lymph node
Introduction
Metastatic tumors in the oral cavity are rare and account for around 1% of all oral malignancies.1,2 Common sources of metastasis to oral region are breast, lung, and kidney.3 These lesions can mimic dental infections and can hinder speech and nutrition. The case presented here was first symptomatic with facial swelling and then was detected to have metastatic lung cancer.
In such rare presentations, the role of a biopsy is unprecedented. The immunohistochemical (IHC) markers done in the above case characterized the primary tumor and aided in further management of the patient.
Case Report
A 32-year-old male reported to this hospital with swelling over his right cheek of 4-month duration. He did not have any known comorbidities and gave a history of tobacco chewing for the past 6 years (one or two pouches per day). On external examination, there was a diffuse swelling seen over the right maxilla, around 3 cm × 4 cm, from right commissure of mouth to 3 cm in front of right ear. Intraoral examination revealed well-defined solitary growth around 4 cm × 4 cm in the right maxillary gingiva buccal sulcus and alveolar region extending from mesial aspect of 14 to dental aspect of 17. It was firm in consistency and did not bleed on touch. History also revealed extraction of 16 followed by closure with buccally advanced flap, around 2 months ago. Contrast-enhanced computed tomography (CECT) of the face and neck was suggestive of a growth involving the upper gingiva buccal sulcus and the maxilla with bony destruction with no significant lymphadenopathy. Differential diagnosis of the swelling was carcinoma maxilla and cystic lesion of maxilla Figure 1.
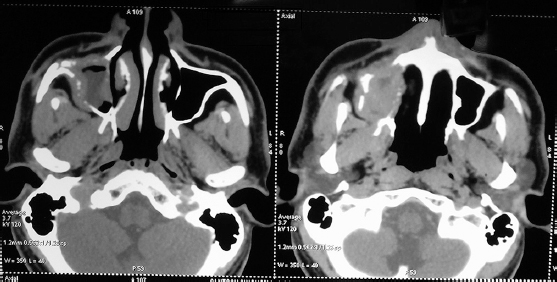
- Axial images of contrast-enhanced computed tomography of face showing soft-tissue lesion in right maxilla with bony destruction
Tru-cut biopsy of the lesion revealed predominantly benign spindle cell proliferation with few islands of atypical epithelial cells with vague ductal/glandular formation Figure 2. The tumor cells were positive for thyroid transcription factor-1 and cytokeratin (CK) 7 and negative for cluster of differentiation 99, CK20, and vimentin, suggestive of metastatic adenocarcinoma with most likely a lung primary Figure 3. The IHC was negative for anaplastic lymphoma kinase and epidermal growth factor receptor mutation analysis.
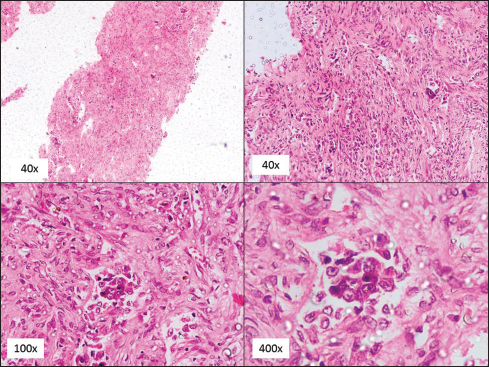
- Spindle cell proliferation with few islands of atypical epithelial cells with ductal/glandular formation
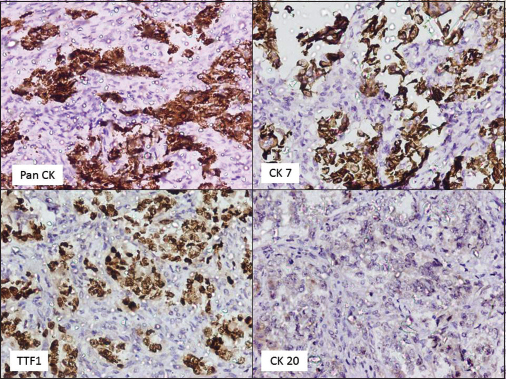
- Tumor cells positive for thyroid transcription factor-1 and cytokeratin 7 and negative for cluster of differentiation 99, cytokeratin 20, and vimentin
With this diagnosis, the patient underwent a CECT scan of the chest, abdomen, and pelvis. It revealed a well-defined heterogeneously enhancing mass in posterobasal segment of left lower lobe around 5.2 cm × 3.9 cm × 7.5 cm in size with mild pleural effusion of left side. Multiple heterogeneously enhancing mediastinal lymph nodes were seen with bilateral nodular opacities in both the lung fields. There were multiple ill-defined poorly delineated space-occupying lesions involving all segments of the liver. The impression was that of a lung primary with multiple liver metastasis and multiple lung nodules bilateral lungs Figures 45. However, an endobronchial biopsy from the lesion was inconclusive.
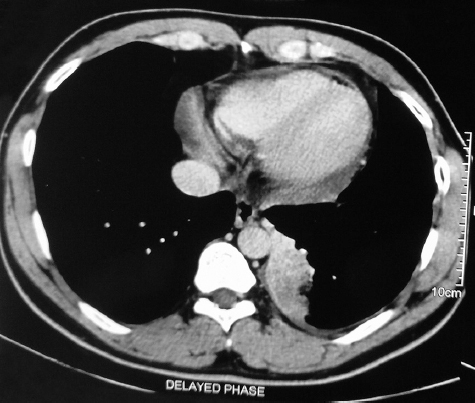
- Well-defined heterogeneously enhancing mass in posterobasal segment of left lower lobe around 5.2 cm × 3.9 cm × 7.5 cm in size with mild pleural effusion
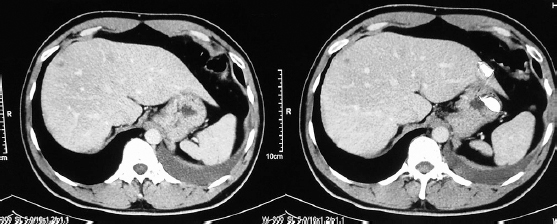
- Multiple ill-defined poorly delineated space-occupying lesions involving all segments of liver
In view of an imaging suggestive of a metastatic lung cancer with biopsy from maxilla confirming metastatic adenocarcinoma, the patient was given a diagnosis of metastatic lung cancer. He was started on palliative chemotherapy with Pemetrexed and Carboplatin (4 cycles) and was treated with palliative radiotherapy (30 Gy/10#) to the maxillary swelling. He showed partial response to radiotherapy and is presently planned for further chemotherapy.
Discussion
Metastasis to the maxilla from primary lung cancer is rare with only a handful of cases being reported so far. Hirshberg et al. reviewed 673 cases of oral metastasis, out of which 112 cases were metastasized from the lung, of which 58 were noted in the jawbones and 54 in the oral mucosa.4 Age ranged from 47 to 84 years (median of 59 years) with slight predisposition toward the male gender.5 It has been seen with all histopathologies of lung cancer. The primary tumor is usually detected before the patient becomes symptomatic with other symptoms, unlike this case.6 In this case, the patient presented with a metastatic site, with an asymptomatic primary.
In case of gingival metastasis, clinical distinction becomes difficult between benign and malignant lesion.7 A rapidly growing gingival mass has a broad differential diagnosis including odontogenic infection, cysts, pyogenic granuloma, and benign tumors. The patient will be symptomatic with local pain, swelling, difficulty in swallowing, and bleeding.2 In case of rapid progression of symptoms along with ulceration and discharge, malignancy should be high on the cards.8
Pathogenesis of oral metastasis is unclear, but thought to be a multistage process in which cells detach themselves from the primary tumor and transported by lymphatic or blood vessels. In oral soft tissues, chronically inflamed mucosa, especially gingiva, has a rich capillary network, which can trap the malignant cells and cause metastasis.8 The primary tumor causing metastases to oral cavity is variable depending on the pattern of colonization in the oral cavity. Lung cancer in males and breast cancer in females remain leading causes.4
The challenge with oral metastasis is late presentation of the primary tumor with multiple sites of metastasis. Hence, prognosis remains dismal. They are treated with systemic chemotherapy and palliative radiotherapy. The average overall survival of metastatic lung cancer is between 4 and 5 months and 1 year, with maximum survival noted for 5 years.9
Conclusion
Oral soft-tissue metastasis in a case of lung cancer is uncommon. Moreover, in this case, the patient presented with an oral swelling which led to the diagnosis of his primary lung cancer. Detailed clinical examination and a thorough histopathological correlation hold the key to diagnosis and management of these patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Metastatic oral soft-tissue lesions: An incidental finding in four cases. South Asian J Cancer. 2013;2:146.
- [Google Scholar]
- Metastasis to oral cavity – A report of two cases and review of literature. Indian J Med Paediatr Oncol. 2005;26:43-6.
- [Google Scholar]
- Metastasis of lung adenocarcinoma to the mandible: Report of a case. J Oral Maxillofac Pathol. 2013;17:253-6.
- [Google Scholar]
- Metastatic tumours to the oral cavity – Pathogenesis and analysis of 673 cases. Oral Oncol. 2008;44:743-52.
- [Google Scholar]
- Metastatic tumours to the oral cavity: A survival study with a special focus on gingival metastases. J Clin Periodontol. 2009;36:488-92.
- [Google Scholar]
- Metastatic lung adenocarcinoma to the mandibular gingiva Case report and review of the literature. Hellenic Archives of Oral & Maxillofacial Surgery. 2012;1:55-61.
- [Google Scholar]
- Gingival metastasis of a bronchogenic adenocarcinoma: Report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e25-8.
- [Google Scholar]







