Translate this page into:
Lymph Nodal Metastatic Pattern in Carcinoma Gallbladder with Multidetector Computed Tomography: An Institutional Experience
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective This work aimed to study the distribution of lymph nodal metastatic pattern in carcinoma gallbladder with multidetector computed tomography (CT).
Materials and Methods A retrospective observational study was conducted including 80 patients with carcinoma gallbladder who underwent triple-phase CT angiography or single-phase contrast-enhanced CT scan of the abdomen between January 2019 and November 2019.
Results In our study, 75 (93.7%) out of 80 cases showed metastasis to lymph nodes, with distribution as follows: periportal (69), peripancreatic (62), and aortocaval (47). The most common involved combination included all three lymph nodal groups (periportal, peripancreatic, and aortocaval), involving 40 (50%) cases. The combination of only periportal and peripancreatic lymph nodes was seen in 17 (21%) cases. Isolated periportal lymph nodes were seen in eight cases (10%) cases. The combination of only periportal and aortocaval lymph nodes was seen in four (5%) cases. Isolated peripancreatic lymph nodes were seen in three (3.7%) cases. The combination of periportal and aortocaval was seen in four (5%) cases followed by peripancreatic and aortocaval lymph nodes that was seen in two (2.5%) cases. Isolated aortocaval lymph nodes were seen in one (1.2%) case.
Conclusion Periportal lymph nodes were the single most commonly involved station followed by peripancreatic and aortocaval lymph nodes. The combination of periportal, peripancreatic, and aortocaval lymph nodes was seen most commonly. The second most commonly involved combination was found to be periportal and peripancreatic lymph nodes followed by isolated periportal lymph nodes.
Keywords
gallbladder cancer
lymph nodes
metastasis
periportal
peripancreatic
aortocaval
Introduction
Primary carcinoma of the gallbladder is the most common malignancy of the biliary tract1 and among the most common malignancy of the gastrointestinal tract.2 In western countries, gallbladder carcinoma has a peak incidence in the sixth and seventh decades of life and is three to five times more predominant in females.3 Recent data have shown a remarkable surge in the incidence of gallbladder cancer in the Indian subcontinent. The reported incidence in Northern India is 10 per 1,00,000, which is higher than South India. Data from South India reported an incidence of around 2 to 3 per 1,00,000.4 Insidious onsets of symptoms make its early diagnosis difficult and are often confused with symptomatic cholelithiasis or chronic cholecystitis.2 Localized tumor in the gallbladder or limited infiltration of the adjacent segments of the liver (segments V and IV) is considered for surgical resection by localized liver segmentectomy and cholecystectomy.3
Adjacent organ or vessel invasion by the tumor, associated metastatic local lymph nodes away from the gallbladder, and distant metastasis are considered inoperable. Many patients of carcinoma gallbladder present with disseminated disease at the time of primary presentation, especially in lower socioeconomic strata. Such cases are considered unresectable because of direct extension into adjacent organs, local lymph node metastasis, or distant metastatic disease.
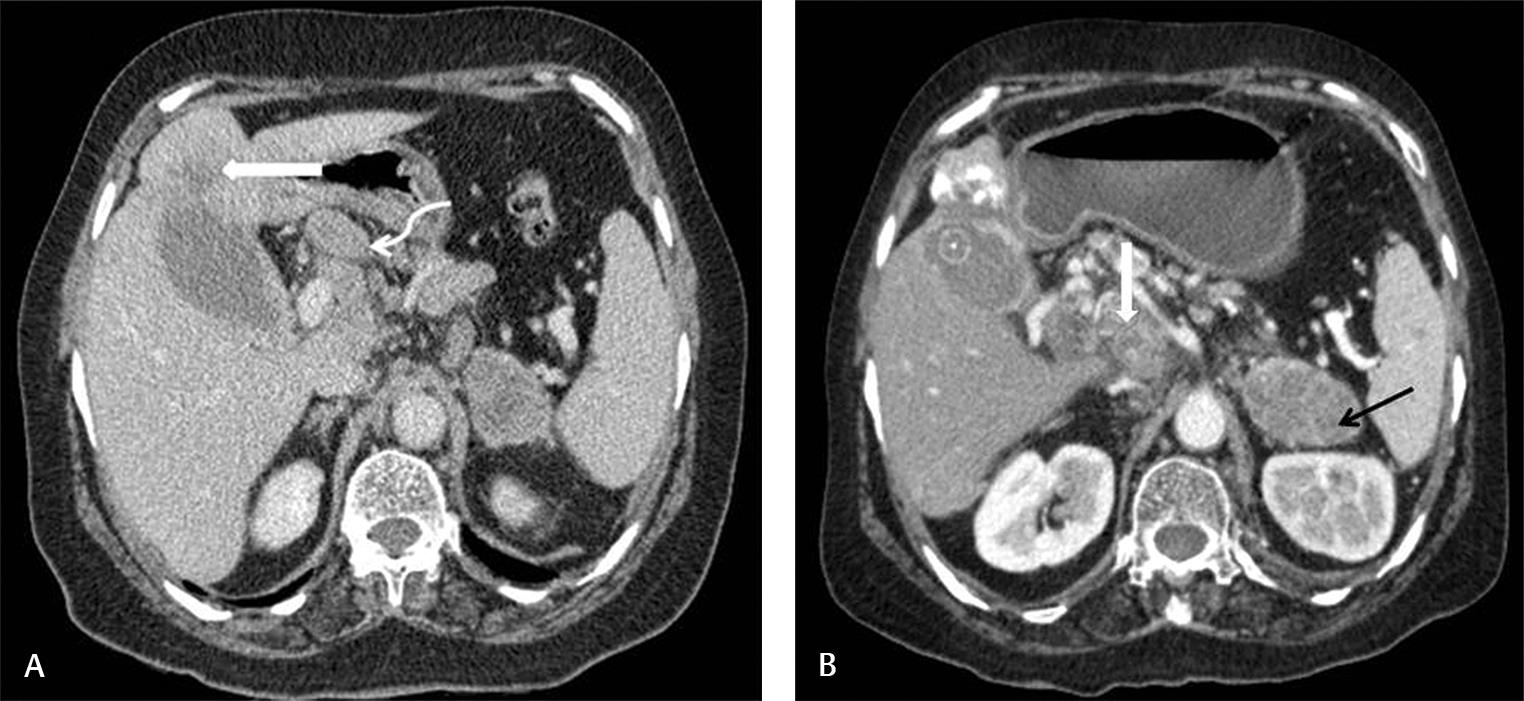
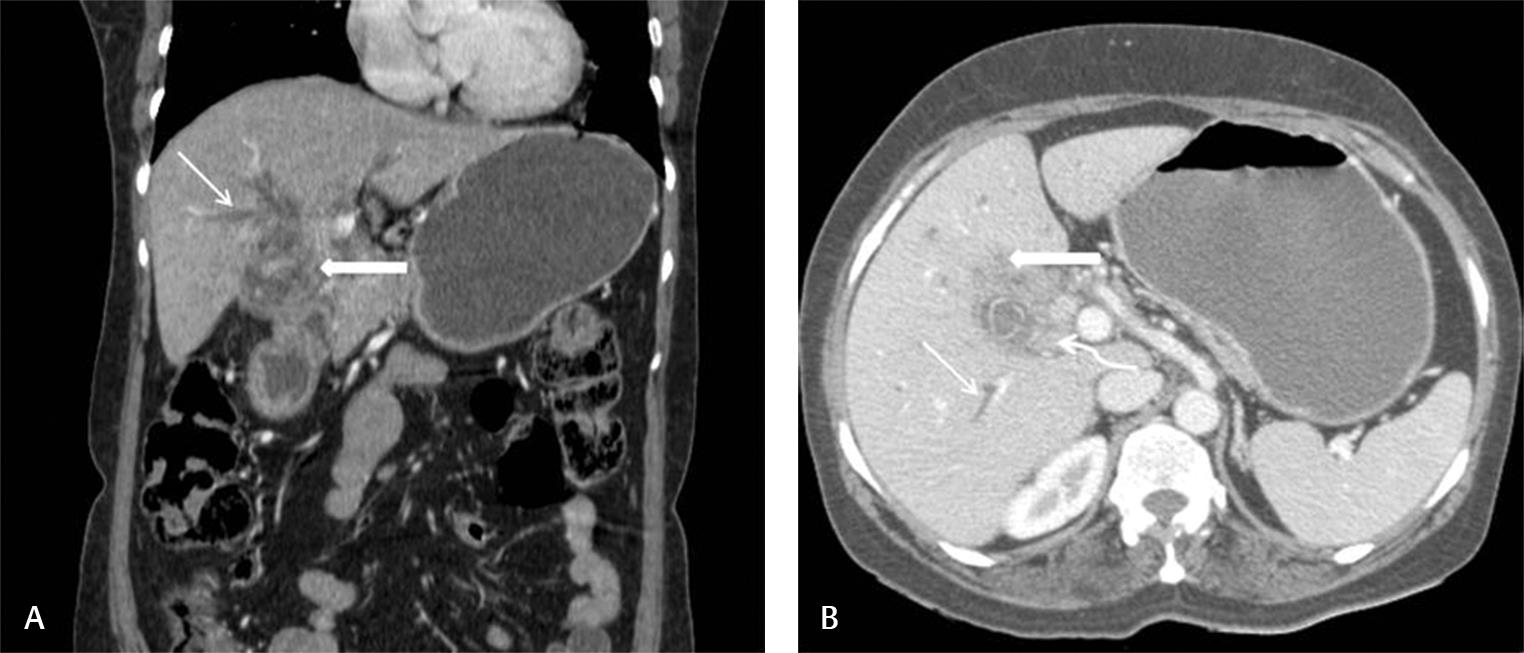
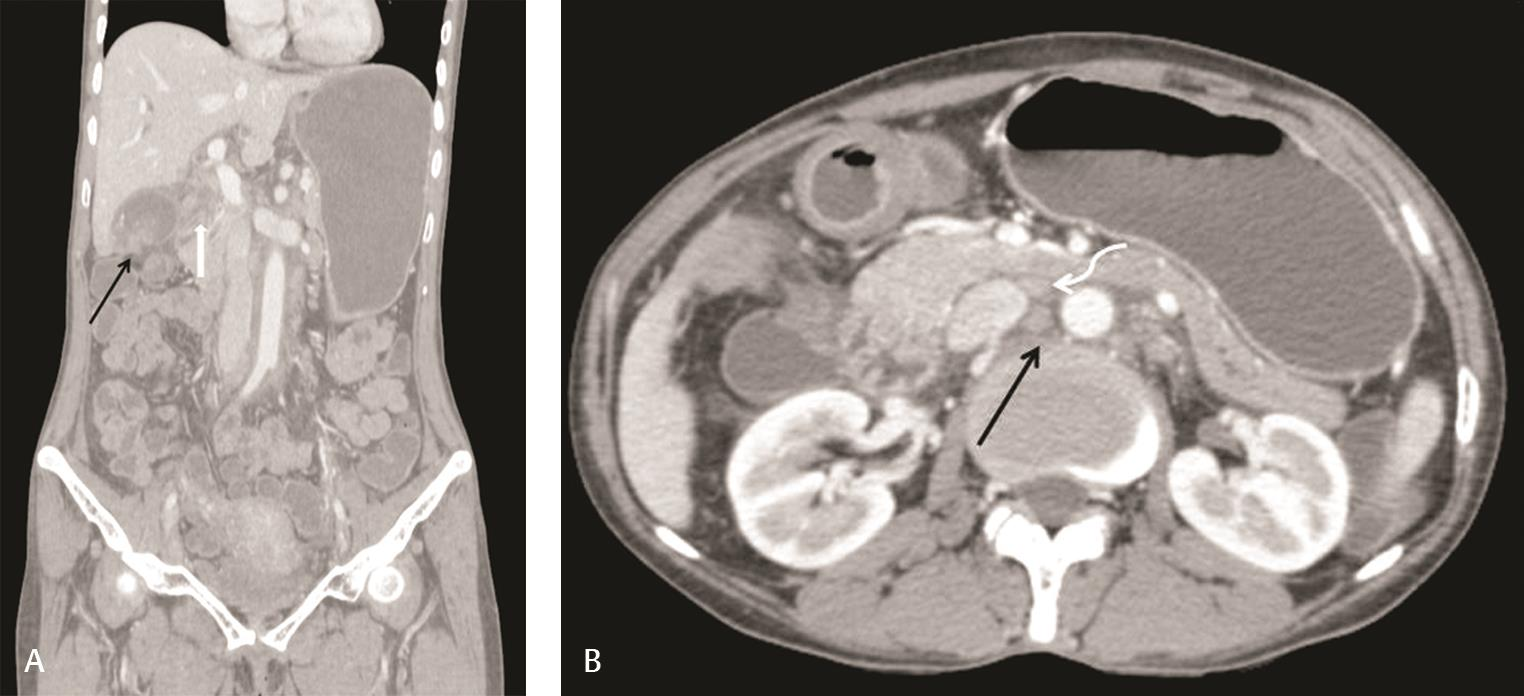
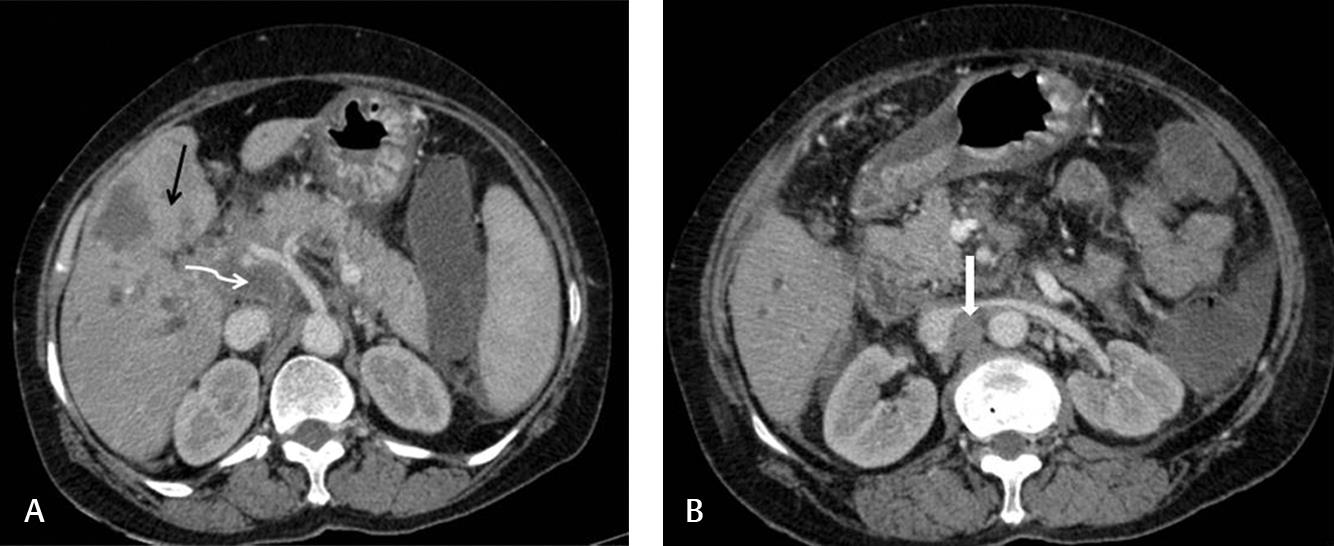
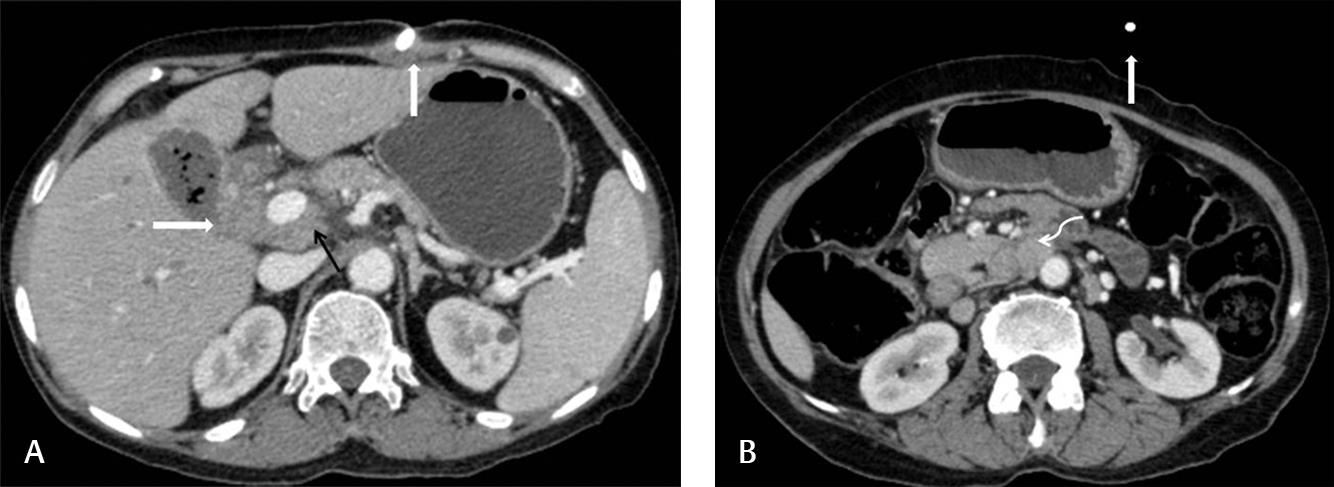
Lymphatic and hematogenous routes are common routes of spread. Liver involvement in gallbladder carcinoma is more likely through lymphatic spread rather than hematogenous dissemination.5,6 Periportal and peripancreatic lymphadenopathy can compress/invade common bile duct and cause dilatation of intrahepatic biliary radicles.7 This finding was confirmed in many cases with positive periportal, peripancreatic, and aortocaval lymph nodes (Figs. 1234). Distant visceral metastases, such as those in the stomach, duodenum, lung, bone, and pancreas, occurs likely through hematogenous dissemination. Distant metastases can also occasionally be seen in the bones and lungs (Fig. 3).1,2 However, direct invasion of other adjacent organs, including the colon, duodenum, stomach, common bile duct, abdominal wall, and diaphragm, is not considered distant metastasis but is classified as T3 or T4, depending on the extent of tumor.7
-
Fig. 1 A known case of gallbladder carcinoma. (A) Axial images show peripherally enhancing exophytic growth arising from the fundus and infiltrating into adjacent liver parenchyma (white arrow) with enlarged enhancing periportal lymph nodes (curved arrow). (B) Axial image shows conglomerated peripancreatic and aortocaval lymph nodes (vertical white arrow). Left adrenal gland metastasis is seen (black arrow).
-
Fig. 2 A 55-year-old female presented with loss of appetite. (A) Coronal and (B) axial image triple-phase CT (computed tomography) scan reformatted images of the abdomen show thickening in gallbladder neck infiltrating into adjacent hepatic parenchyma, biliary confluence, and duodenum (thick white arrow). Enhancing periportal lymph nodes (curved white arrow) are seen. Mild dilatation of central intrahepatic biliary radicles is noted (thin white arrow).

-
Fig. 3 A 75-year-old female presented with painless progressive jaundice. (A) Coronal image of triple-phase CT (computed tomography) scan shows diffusely thickened gallbladder wall with asymmetric nodular enhancing soft tissue component infiltrating into the adjacent liver parenchyma (white arrowhead). Adjacent enlarged nonenhancing periportal lymph nodes are seen (white curved arrow), encasing the portal vein and causing mild compression. Compression of the common hepatic duct with bilobar intrahepatic biliary radicles dilatation is seen (black arrow). Numerous nodules of varying sizes are noted in the lungs (elbow arrow connector). (B) Axial image shows hepatic infiltration with numerous hepatic metastases in both lobes of the liver. (C) Axial image shows aortocaval lymph nodes (vertical white arrow).
-
Fig. 4 A 45-year-old female presented with jaundice. (A) Coronal triple-phase CT (computed tomography) scan reformatted image of the abdomen shows a heterogeneously enhancing periportal lymph nodal mass (white arrow) encasing the common hepatic duct. Mild central dilatation of intrahepatic biliary radicles is noted. Endophytic gallbladder mass is seen with surrounding fat stranding (black arrow). (B) Axial image shows multiple enlarged peripancreatic (black arrow) and aortocaval lymph nodes (curved road).
In this study, we will discuss the lymph nodal spread on multidetector computed tomography (MDCT) in cases of gallbladder carcinoma including its extent. These data will make an impact on the surgical evaluation and the management of these lesions. Lymph nodal involvement was commonly noted with MDCT as compared with ultrasound or magnetic resonance imaging (MRI). Our institution is a tertiary care center with predominant oncology patient load. According to our knowledge, there is no such study carried out in North India to study the distribution and incidence of lymph nodal metastasis in carcinoma of the gallbladder. Our study findings for lymph nodal metastasis on CT scan was corresponding to CT scan findings in a meta-analysis by de Savornin Lohman et al.8 Some studies8,9 have used a size criterion of >10 mm as a cutoff value of a diameter for labeling a lymph node positive. We have included size, heterogeneous enhancement, and necrotic lymph nodes as the criteria for lymph node involvement.10
Materials and Methods
An observational descriptive study was conducted including 80 patients with gallbladder carcinoma who underwent triple-phase CT angiography or contrast-enhanced CT scan of the abdomen between January 2019 and November 2019. All triple-phase CT examinations were performed on a 64-MDCT scanner (Extended Brilliance Workspace, Version 6.4, Philips Medical System), which worked at 64 mm × 1 mm collimation, with a minimum slice thickness of 0.625 mm. The machine operates at 120 kV and 320 mAs. The patients did not eat or drink for 4 to 6 hours. After nonenhanced liver images, CT angiography was performed after the intravenous (IV) administration of nonionic contrast material, that is, iodixanol (visipaque). The contrast medium and saline solution were injected with a MEDRAD power injector (Bayer HealthCare) at 3 mL/second through an 18-gauge plastic IV catheter placed in an antecubital vein in most of the cases. Contrast medium volumes varied between 100 and 150 mL at1.5 ml/kg. Water (∼2,000 mL) was administered to all patients as a nonopaque oral contrast agent. Dynamic images were obtained during the hepatic arterial, portal venous, and equilibrium phases. After injection of IV contrast material, the liver was scanned in arterial (scanning delay: 20–30 seconds), portal (scanning delay, 60–70 seconds), and equilibrium (scanning delay at 3 minutes) phases. Contrast-enhanced CT scan of the abdomen was performed using approximately 90 to 100 mL of contrast. Abdominal aorta was set as the region of interest for automatic triggering, with a required density of 160 HU for starting the scan in the arterial phase, and the portal venous phase was scanned after a delay of 60 seconds. Liver and gallbladder fossa were covered in delayed scans after 3 minutes. Single-phase CT scan was performed using 70 mL of contrast. Reconstruction of the transverse section data was with 0.625-mm-thick sections at 0.625-mm intervals. These obtained images were transferred to the workstation to construct coronal, sagittal, and curved multiplanar reformatted images.
CT scan images were processed and analyzed with multiplanar reformation at the available workstation. Patients were analyzed for lymph nodal site, enlarged size, heterogeneous enhancement pattern, or nonenhancing necrotic nodes. This study aims at observing and documenting the extent of lymph nodal involvement.
Result
Among the 80 patients included in our study, there were 61 females and 19 males. The female-to-male ratio was 3.2:1. Their ages ranged from 40 to 90 years old (average: 50–60 years). Gallbladder carcinoma was the radiological diagnosis based on the MDCT findings in all the patients. Of the patients, 31.2% were between 50 and 60 years of age. Most (92.5%) of the patients were above 40 years of age. The spectrum of radiologic findings included focal or diffuse thickening of the gallbladder wall, a mass in the gallbladder fossa, and an intraluminal mass. In our study, among the total of 80 cases, lymph nodal metastasis was the most common and was seen in 75 (93.7%) cases, with distribution as follows: periportal (69), peripancreatic (62), and aortocaval (47).
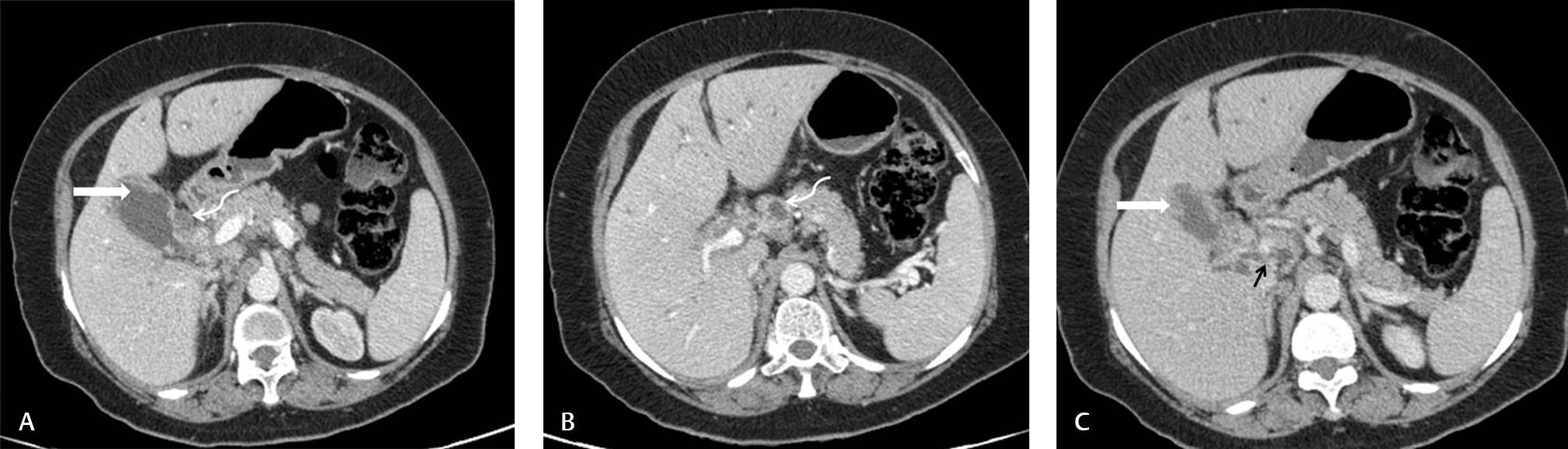
The most common involved combination included all three lymph nodal groups (periportal, peripancreatic, and aortocaval) in 40 (50%) cases (Figs. 1234). The combination of only periportal and peripancreatic lymph nodes was seen in 17 (21%) cases (Fig. 5). The combination of only periportal and aortocaval lymph nodes was seen in four (5%) cases (Fig. 6). The combination of only peripancreatic and aortocaval lymph nodes was seen in two (2.5%) cases (Fig. 7). Isolated periportal lymph nodes were seen in eight (10%) cases. Isolated peripancreatic lymph nodes were seen in three (3.7%) cases. Isolated aortocaval lymph nodes were seen in one (1.2%) cases.
-
Fig. 5 (A,C) Triple-phase angiographic images of a 65-year-old female presenting with weight loss show irregular heterogeneously enhancing thickening of the gallbladder fundus, neck, and body (horizontal white arrow). (B) Enlarged periportal lymph nodes (curved arrow) are seen, showing central necrosis. It is encasing the common bile duct, with mild dilatation of central intrahepatic biliary radicles. (C) Heterogeneously enhancing peripancreatic lymph nodes are annotated by a black arrow.
-
Fig. 6 (A) A 40-year-old female with large heterogeneous peripherally enhancing lesion in the gallbladder fossa (black arrow) infiltrating into the liver parenchyma and adjacent structures. Enlarged necrotic periportal lymph nodal mass (curved arrow) is infiltrating the common hepatic duct, with mild dilatation of biliary radicals. (B) Enlarged necrotic aortocaval lymph nodes (white vertical arrow).
-
Fig. 7 Known case of carcinoma gallbladder shows (A) irregular enhancing wall thickening (horizontal arrow) infiltrating into the adjacent parenchyma. Enlarged peripancreatic lymph nodes are seen (black arrow). (B) Enlarged enhancing aortocaval lymph nodes are seen (curved arrow). Vertical white arrow shows the percutaneous transhepatic biliary drainage tube.
Associated consistent findings were cholelithiasis, biliary duct dilatation, invasion of the adjacent structures, and distant metastases of the liver and other organs.
Discussion
Many patients of carcinoma gallbladder present with disseminated disease at the time of primary presentation, especially in lower socioeconomic strata. Primary gallbladder carcinoma is the most common malignancy of the biliary tract.11,12 Surgical resection with clear margins is the most definitive treatment, whenever possible. However, most of the cases at our institute were in the unresectable category with enlarged/necrotic locoregional lymph nodes or distant metastasis. The reformatted images in sagittal and coronal were very beneficial in this study in assessing the extension of lymphatic spread. Whenever possible, radical resection is attempted, including lymph node dissection, extrahepatic bile duct, and liver bed resection.13,14 Precise three-dimensional reconstruction of MDCT helps detect direct infiltration, aids in detailed presurgical anatomical evaluation, and contributes in postsurgical follow-up and evaluation for recurrent or residual disease. Most commonly seen routes of dissemination are direct invasion of the liver, lymphatic, and hematogenous. Approximately 50% of patients have nodal metastases at diagnosis according to Hussain et al. Even though hepatic invasion or hepatic metastasis has been reported in as many as 30 to 80% of cases of gallbladder carcinoma, lymphatic spread of gallbladder carcinoma to the liver is faster than hematogenous dissemination according to Hussain et al.1 This was consistent with our study. Apart from characterizing different enhancement patterns of primary growth, CT also rules out other inflammatory pathologies. Metastatic lymph nodal status predicts survival. Kanthan et al suggested effective lymph node dissection to be the most valuable procedure for improving survival and that involvement of the peripancreatic nodes is indicative of a worse outcome.10
In 2012, Shirai et al compared various lymph nodal involvement studies in carcinoma gallbladder. According to it, Endo et al (2006) suggested that the number of positive nodes better predicts postsurgical prognosis. A major problem in the early diagnosis of gallbladder carcinoma is the fact that it is asymptomatic, and if it is symptomatic, its symptoms overlap with other benign biliary tract diseases. Another study of Negi et al15 suggested lymph node ratio to be a better predictor rather than location or number alone. They gave the reasoning that in en bloc resection procedure, it is difficult to determine the location of lymph node.16,17 The meta-analysis by de Savornin Lohman et al evaluated the diagnostic accuracy of five studies and revealed uncertainty regarding the optimal imaging strategy for the preoperative detection of lymph nodal metastasis in carcinoma gallbladder. Routine imaging by CT is followed for preoperative staging. Additional MRI is advised only in case of inconclusive CT results. Both CT and MRI demonstrate varying sensitivity. However, for the detection of lymph nodal metastasis of size < 10 mm, imaging is unreliable because in their study all false-negative lymph nodes were <10 mm in size.8 In correspondence to Mitchell et al, we included lymph nodes that were either enlarged in size (>1 cm), heterogeneous intensity (indicating central necrosis), or altered morphology.11
Pilgrim et al emphasized on the significance of preoperative scanning. Enlarged nodes before any surgery are more ominous for malignancy. Local nodal disease on postoperative scanning is particularly difficult to characterize after cholecystectomy for unexpected carcinoma gallbladder, as differentiating malignant nodal involvement from inflammation is not possible on imaging. Para-aortic nodal involvement is, however, much less likely to be attributable to the postoperative state in this context.12 Nakagawara et al in 2014 studied the artery supplying pericholedochal lymph nodes with an embryological approach. They suggested that in cases with normal hepatic arterial branching, the lymphadenopathy observed was compatible with lymph nodes along a regressed embryonic right hepatic artery, and emphasized the importance of dissection along its course.17 Lymphatic spread of gallbladder carcinoma occurs to lymph nodes around the cystic duct, common bile duct, and pancreaticoduodenal region. Carcinoma gallbladder spreads directly into the adjacent liver segments (IV and V), duodenum, colon, anterior abdominal wall, and common hepatic duct. Biliary obstruction and upstream biliary radicles dilatation due to lymph nodal metastasis or direct invasion at porta is a common finding. Other possible routes of spread include venous intraductal and perineural. Oikarinen et al suggested that in gallbladder carcinoma, quadrate lobe protrusion because of lymph node enlargement is specific.9,18,19
Kalra et al emphasized the role of CT scan as a modality in picking up diagnosis, especially with the help of three-dimensional reformatted images.9 We had similar observation in our study. Furlan et al reported an accuracy of up to 84% in determining local extent of primary gallbladder carcinoma and 85% in delineating lymphadenopathy, distant metastases, and hepatic and vascular invasion.20 Complete preoperative evaluation has a pivot role in successful surgery.21 Lin et al suggested that the depth of the primary tumor strongly determined the frequency of involvement of lymph nodes and affected postprocedural survival rate. The study emphasized on achieving a negative surgical margin of 2 cm from the tumor.22 Hepatectomy and pancreaticoduodenectomy combined is a common indication when there is direct duodenal or pancreatic invasion and peripancreatic lymph node involvement. Positive lymph nodes are not absolute contraindications for pancreaticoduodenectomy for gallbladder cancers. This procedure provides the greatest number of dissected lymph nodes.9
Conclusion
We conclude that lymph nodes are one of the most common sites in the route of spread of gallbladder carcinoma. The mean age was between 50 and 60 years, and females were affected more commonly. In our study, most of the patients were lymph node positive during the scan. The combination of all three lymph nodal group was the most commonly involved combination (periportal, peripancreatic, and aortocaval) seen in 40 (50%) cases. The second most commonly involved group was found to be periportal and peripancreatic lymph nodes in 17 (21%) cases. The next commonly involved combination of only periportal and aortocaval lymph nodes was seen in four (5%) cases. The combination of only peripancreatic and aortocaval lymph nodes was seen in two (2.5%) cases. Biliary obstruction is a common finding owing to either lymph nodal compression or direct infiltration of the common hepatic duct/common bile duct. CT scan helps not only in picking up gallbladder masses but also in evaluating its extension and documenting lymph nodal involvement. It also has a mainstay in preoperative planning and comparative reevaluation.9
Conflict of Interest
None declared.
References
- AIRP best cases in radiologic-pathologic correlation: gallbladder carcinoma with direct invasion of the liver. Radiographics. 2013;33(01):103-108.
- [Google Scholar]
- Role of multidetector computed tomography (MDCT) in diagnosis and staging of gall bladder carcinoma. Egyptian J Radiol Nucl Med. 2013;44(01):1-7.
- [Google Scholar]
- Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg. 2000;232(04):557-569.
- [Google Scholar]
- Global epidemiological trends and variations in the burden of gallbladder cancer. J Surg Oncol. 2017;115(05):580-590.
- [Google Scholar]
- Gallbladder wall thickening: MR imaging and pathologic correlation with emphasis on layered pattern. Eur Radiol. 2005;15(04):694-701.
- [Google Scholar]
- Diffuse gallbladder wall thickening: differential diagnosis. Am J Roentgenol. 2007;188(02):495-501.
- [Google Scholar]
- The diagnostic accuracy of CT and MRI for the detection of lymph node metastases in gallbladder cancer: a systematic review and meta-analysis. Eur J Radiol. 2019;110:156-162.
- [Google Scholar]
- MDCT in the staging of gallbladder carcinoma. Am J Roentgenol. 2006;186(03):758-762.
- [Google Scholar]
- Features suggestive of gallbladder malignancy: analysis of T1, T2, and T3 tumors on cross-sectional imaging. J Comput Assist Tomogr. 2014;38(02):235-241.
- [Google Scholar]
- An often overlooked diagnosis: imaging features of gallbladder cancer. J Am Coll Surg. 2013;216(02):333-339.
- [Google Scholar]
- Long-term survival of a recurrent gallbladder carcinoma patient with lymph node and peritoneal metastases after multidisciplinary treatments: a case report. Surg Case Rep. 2016;2(01):12.
- [Google Scholar]
- Carcinoma of the gallbladder: imaging features with surgical correlation. Am J Roentgenol. 1997;169(03):781-785.
- [Google Scholar]
- Lymph nodal involvement as prognostic factor in gallbladder cancer: location, count or ratio? J Gastrointest Surg. 2011;15:1017-1025.
- [Google Scholar]
- Assessment of lymph node status in gallbladder cancer: location, number, or ratio of positive nodes. World J Surg Oncol. 2012;10(01):87.
- [Google Scholar]
- Lymph node spread of gallbladder cancer from the perspective of embryologically-based anatomy and significance of the lymphatic basin along the embryonic right hepatic artery. Mol Clin Oncol. 2014;2(06):963-967.
- [Google Scholar]
- Diagnostic imaging of carcinomas of the gallbladder and the bile ducts. Acta Radiol. 2006;47(04):345-358.
- [Google Scholar]
- Gallbladder carcinoma: radiologic-pathologic correlation. Radiographics. 2001;21(02):295-314, 549–555.
- [Google Scholar]
- Gallbladder carcinoma update: multimodality imaging evaluation, staging, and treatment options. Am J Roentgenol. 2008;191(05):1440-1447.
- [Google Scholar]
- Metastasis of primary gallbladder carcinoma in lymph node and liver. World J Gastroenterol. 2005;11(05):748-751.
- [Google Scholar]








