Translate this page into:
Estimation of tumor volume and its prognostic significance to study the biological behavior of carcinoma of cervix
Address for correspondence: Dr. Ketan GargA-279, First Floor, Shivalik, New Delhi - 110 017, India. ketan_nikhil@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective: The objective of this study was to assess a correlation between tumor volume, the spread and metastatic potential of the tumor.
Materials and Methods: A prospective study was done on 40 cases of carcinoma of cervix with stage IIb or less. The hysterectomy specimens alongwith the lymph nodes were sent to the histopathology department. Clinical details were taken from gynecology department. Hematoxylin and eosin slides were prepared and seen. Tumor volume was calculated by using the formula TV = π/6×Length×Width×Depth. Immunohistochemistry for Fibronectin and LN5 was also done.
Results: The median age of the patients in this group was 47.5 years, with a range of 30–80 years. The major histological type of carcinoma among 40 cases is squamous cell carcinoma (SCC) (in 90% of cases), and 10% had adenocarcinoma. Pathological staging of the carcinoma cervix showed stage Ib, IIa, IIb, and IVa (35%, 20%, 40%, and 5%). Tumor volume estimated on pathological specimens of 40 cases ranged from 230 cumm to 49,760 cumm with a mean of 14,844 cumm. 12 (30%) cases had tumor volume more than 15,000 cumm, 12 (30%) cases had tumor volume <5000 cumm and 16 (40%) cases had tumor volume between 5000 and 15,000 cumm. 17% of the tumors with tumor volume <5000 cumm showed lymph node metastases, whereas 67% (out of 12cases) of cases with tumor volume more than 15,000 cumm showed lymph node metastases. 67% of the tumors with tumor volume <5000 cumm showed 0/4 organs involvement, whereas all cases with tumor volume more than 15,000 cumm showed more than one organ involvement among vagina, uterus, parametrium or bladder/rectum. Fibronectin positivity was seen in 22 out of 44 cases (55%). Macrophages were seen surrounding the group of tumor cells by LN5 immunostaining.
Conclusion: Tumor volume can be considered as an independent prognostic factor to assess the spread of the tumor. Cases with tumor volume <5000 cumm show low risk in terms of parametrial involvement and lymph node metastasis and those with tumor volume more than 15,000 cumm showed more organ spread. Fibronectin positivity carries some importance in low-risk cases. For macrophages, further detailed study needs to be carried out.
Keywords
Carcinoma
fibronectin
tumor volume
Introduction
Carcinoma of cervix is the most common form of cancer in women in most developing countries. It affects women of middle age group. The lesion commences at the squamocolumnar junction in the transformation zone and spreads characteristically by direct extension to the vagina, corpus, parametrium, lower urinary tract, and uterosacral ligaments. Lymph node metastasis is also common, in a sequential fashion, and is related to the stage of the disease. Prognosis of cervical carcinoma is primarily determined by clinical stage (International Federation of Gynecology and Obstetrics [FIGO]) and presence or absence of nodal metastases. Few other prognostic indicators like tumor size, depth of invasion, vascular invasion, etc., are also taken into account. Keeping in view the biological behavior of the tumor, an attempt is made to study the tumor volume and the metastatic potential of the tumor in cases of carcinoma cervix. A study on the extracellular membrane (fibronectin) and macrophages (LN-5) as a part of tumor immunity has also been done.
Materials and Methods
A prospective study was done on 40 cases of carcinoma cervix to assess a correlation between tumor volume, the spread, and metastatic potential of the tumor. The study was done on material received in the tumor pathology laboratory from patients attending the gynecology department of Safdarjang Hospital. Clinical data were also received from the gynecology department itself. X-ray findings, cystoscopic findings (in selected cases), and per operative findings regarding the extent of the tumor was also recorded in all the patients. An informed consent for a radical hysterectomy was taken from all the patients. All the patients underwent radical hysterectomy with pelvic lymph node sampling with or without para-aortic lymph node sampling. The hysterectomy specimen and the lymph nodes were examined pathologically. For the preparation of histologic slides, specimens were fixed in formalin. The cut sections were dehydrated and paraffin embedded and the blocks so obtained were cut into very thin slices, placed in glass slides, and stained with hematoxylin and eosin.
Measurement of cervical tumor was done systematically. The specimen was cut longitudinally on the anterior surface from the fundus of the uterus to the external os of the cervix. The maximum limit of the grossly visible tumor was measured with a pair of calipers. Maximum horizontal and vertical distance was measured at three levels. Each specimen was cut into 4–12 sections. According to the size of the tumor mass, tissue was processed from each section. Cross-section slice was seen for depth of malignant infiltration. The surface area of each cross-section was calculated. The total volume (TV) of each section was calculated by multiplying the surface area by the thickness of each section. Finally, the total TV was calculated by adding the sectional volumes.
TV = π/6 × Length × Width × Depth.
Immunohistochemistry was done to detect fibronectin production by the tumor, and LN-5 to identify the macrophages in the inflammatory infiltrate in and around the tumor cells.
Results
A total of 40 patients attending the gynecology Department of Safdarjang Hospital within the diagnostic group of carcinoma cervix clinical stage less than or equal to IIb were included in the study group. The median age of the patients in this group was 47.5 years, with a range of 30–80 years Table 1 and Graph 1.
|
Age in years |
Number of patients (%) |
|---|---|
|
30-39 |
10 (25) |
|
40-49 |
14 (35) |
|
50-59 |
10 (25) |
|
60-69 |
4 (10) |
|
70-79 |
2 (5) |
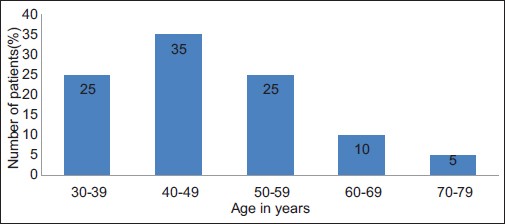
- Graph 1: Age distribution
Majority of the patients attained menarche after 12 years (85%). A total of 55% had attained menopause at the time of presentation. 65% of the patients had 1–5 children. There was a positive history of tobacco smoking in 24 patients of which 6 smoked themselves.
The most common complaint in these patients was bleeding per vaginum. Other complaints were discharge per vaginum, postcoital bleeding. Clinical reports of the 40 patients revealed that 22 of them had tumor size more than 3 cm in diameter. The various parameters studied were the diameter of the tumor, vaginal involvement, and parametrial involvement. Finally, clinical staging was evaluated depending on these parameters Table 2.
|
Parameters assessed |
Number of patients (%) |
|---|---|
|
Diameter of growth (cm) |
|
|
<3 |
18 (45) |
|
>3 |
22 (55) |
|
Vaginal involvement |
|
|
Yes |
16 (40) |
|
No |
24 (60) |
|
Parametrial involvement |
|
|
Yes unilateral |
4 (10) |
|
Yes bilateral |
6 (15) |
|
No |
30 (75) |
|
Final clinical staging |
|
|
Ib |
22 (55) |
|
IIa |
8 (20) |
|
IIb |
10 (25) |
Grossly, the tumor was seen restricted to the transition zone Figure 1, or a fungating tumor extending to the isthmus Figure 2, or an ulceroproliferative lesion extending to the vaginal cuff Figure 3. The major histological type of carcinoma among 40 cases is squamous cell carcinoma (SCC) (in 90% of cases) Figure 4, and 10% had adenocarcinoma Figure 5. Histopathological examination of the specimens revealed vaginal cuff involvement in 50% of cases. Parametrial and bladder involvement was also seen among few cases. Pathological staging of the carcinoma cervix showed stage Ib, IIa, IIb, and IVa (35%, 20%, 40%, and 5%) Table 3.

- Gross specimen showing cervical carcinoma restricted to the transition zone
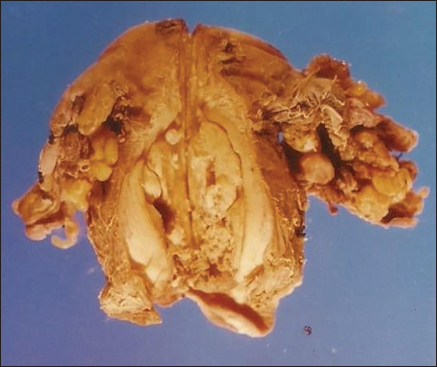
- Gross hysterectomy specimen showing fungating tumor extending to the isthmus

- Gross hysterectomy specimen showing ulceroproliferative lesion extending to the vaginal cuff
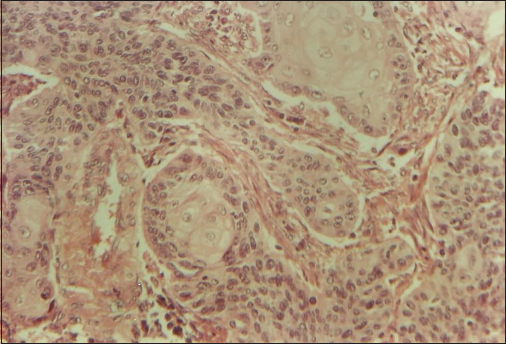
- H and E section showing well differentiated squamous cell carcinoma cervix
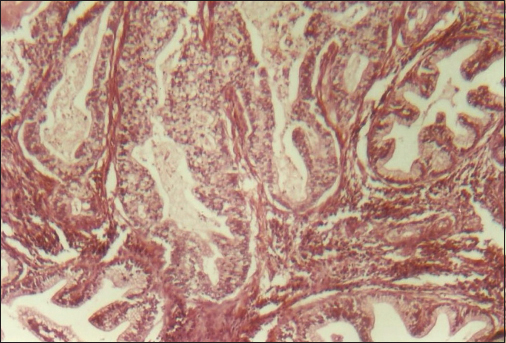
- H and E section showing adenocarcinoma cervix
|
Parameters assessed |
Number of patients (%) |
|---|---|
|
Vaginal involvement |
|
|
Yes |
20 (50) |
|
No |
20 (50) |
|
Parametrial involvement |
|
|
Yes unilateral |
6 (15) |
|
Yes bilateral |
10 (25) |
|
No |
24 (60) |
|
Bladder invasion |
|
|
Yes |
2 (5) |
|
No |
38 (90) |
|
Rectal invasion |
|
|
Yes |
0 (0) |
|
No |
40 (100) |
|
Final histopathological staging |
|
|
Ib |
14 (35) |
|
IIa |
8 (20) |
|
IIb |
16 (40) |
|
IVA |
2 (5) |
Different tumors with different staging have been seen to show different tumor volume. Both cases with IVa staging showed tumor volume more than 15,000 cumm Table 4.
|
Tumor volume (cumm) |
Ib |
IIa |
IIb |
IVa |
|---|---|---|---|---|
|
<5000 |
8 |
2 |
2 |
0 |
|
5000-10,000 |
0 |
4 |
2 |
0 |
|
10,000-15,000 |
4 |
0 |
6 |
0 |
|
>15,000 |
2 |
2 |
6 |
2 |
|
Total number of cases (%) |
14 (35) |
8 (20) |
16 (40) |
2 (5) |
Tumor extension into the uterus was observed in 20 specimens. Tumor deposits in the parametrial tissue Figure 6 and serosal aspect of the fallopian tube Figure 7 was seen in few cases. Tumor spread to pelvic lymph nodes was observed in 12 cases, obturator group being the most commonly involved Figure 8. Tumor volume estimated on pathological specimens of 40 cases ranged from 230 cumm to 49,760 cumm with a mean of 14,844 cumm.
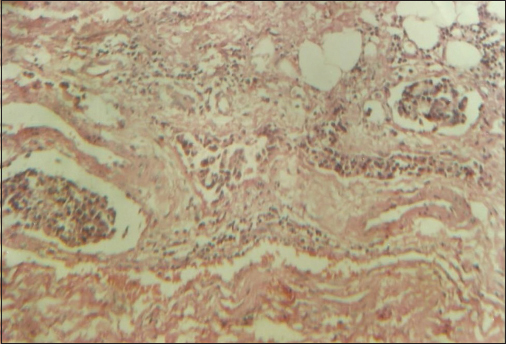
- H and E section showing tumor deposits in the parametrial tissue
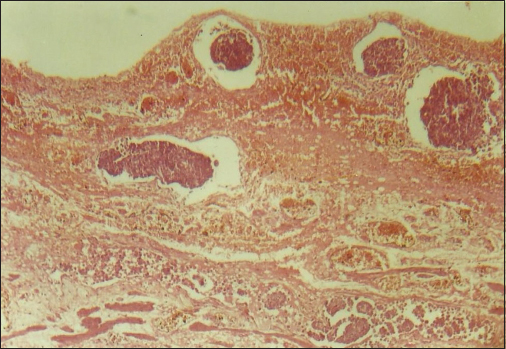
- H and E section showing tumor deposits in the serosal aspect of the fallopian tube
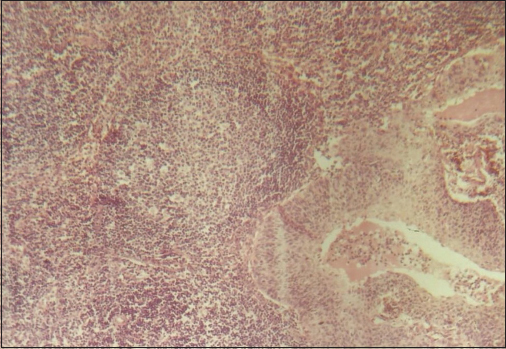
- H and E section showing tumor deposits in the lymph node
Correlation between tumor volume, lymph node metastasis, vaginal involvement, parametrial involvement, uterine extension of tumor, and tumor differentiation
12 (30%) cases had tumor volume more than 15,000 cumm, 12 (30%) cases had tumor volume < 5000 cumm, 16 (40%) cases had tumor volume between 5000 and 15,000 cumm Graph 2.
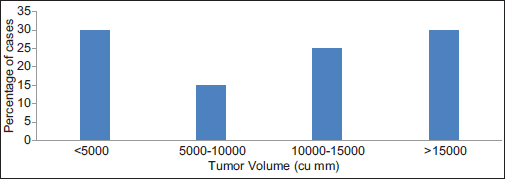
- Graph 2: Tumor volume in cases of carcinoma cervix
Among 12 of the tumors with tumor volume <5000 cumm, only 2 (17%) showed lymph node metastases, whereas 67% (out of 12 cases) of cases with tumor volume more than 15,000 cumm showed lymph node metastases. In between tumor volume ranges 5000–10,000 and 10,000–15,000 cumm, cases did not show any significant difference in lymph node metastasis Graph 3.
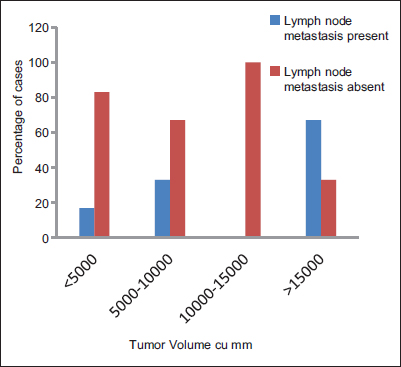
- Graph 3: Correlation of tumor volume with lymph node metastasis
Twenty (50%) cases showed vaginal involvement by the tumor. Among 12 of the tumors with tumor volume <5000 cumm, only 2 (17%) showed vaginal involvement, whereas all cases with tumor volume more than 15,000 cumm showed vaginal involvement. In between tumor volume ranges 5000–10,000 and 10,000–15,000 cumm, cases did not show any significant difference in vaginal involvement. Twenty (50%) cases showed the extension of tumor into the uterine corpus. Among 12 of the tumors with tumor volume <5000 cumm, only 4 (33%) showed uterine involvement, whereas 10 (83%) cases with tumor volume more than 15,000 cumm showed uterine involvement. In between tumor volume ranges 5000–10,000 and 10,000–15,000 cumm, cases did not show any significant difference in uterine involvement. Sixteen (40%) cases showed parametrial involvement. Among 12 of the tumors with tumor volume <5000 cumm, only 2 (17%) showed parametrial involvement, whereas all cases with tumor volume more than 15,000 cumm showed parametrial involvement. In between tumor volume ranges 5000– 10,000 and 10,000–15,000 cumm, cases did not show any significant difference in parametrial involvement Table 5.
|
Tumor volume (cumm) |
Number of cases (%) |
Number of cases with bladder/rectum involvement (%) |
Number of cases with vaginal involvement (%) |
Number of cases with uterine involvement (%) |
Number of cases with parametrial involvement (%) |
|---|---|---|---|---|---|
|
<5000 |
12 (30) |
0 (0) |
2 (17) |
4 (33) |
2 (17) |
|
5000-10,000 |
6 (15) |
2 (33) |
4 (67) |
4 (67) |
2 (33) |
|
10,000-15,000 |
10 (25) |
0 (0) |
2 (20) |
2 (20) |
4 (40) |
|
>15,000 |
12 (30) |
0 (0) |
12 (100) |
10 (83) |
12 (100) |
The involvement of various organs in cases of carcinoma cervix was assessed, and the cases involving multiple organs together in the same cases were assessed. No case showed the involvement of all four organs (uterus, vagina, parametrium, bladder/rectum) Table 6.
|
Tumor volume (cumm) |
Number of cases (%) |
0 out of 4 organs involvement |
1 out of 4 organs involvement |
2 out of 4 organs involvement |
3 out of 4 organs involvement |
|---|---|---|---|---|---|
|
<5000 |
12 (30) |
8 |
2 |
0 |
2 |
|
5000-10,000 |
6 (15) |
2 |
0 |
2 |
2 |
|
10,000-15,000 |
10 (25) |
4 |
6 |
0 |
0 |
|
>15,000 |
12 (30) |
0 |
0 |
2 |
10 |
There were eight cases which showed well differentiated SCC (WDSCC). All of them had tumor volume <5000 cumm. Twenty-eight cases had large cell nonkeratinizing SCC, out of which 4 had tumor volume <5000 cumm, 6 had 5000–10,000 cumm, 8 had 10,000–15,000 cumm, and 10 had more than 15,000 cumm of tumor volume. Four cases had adenocarcinoma, out of which two had tumor volume 10,000–15,000 cumm and the other two more than 15,000 cumm Graph 4.
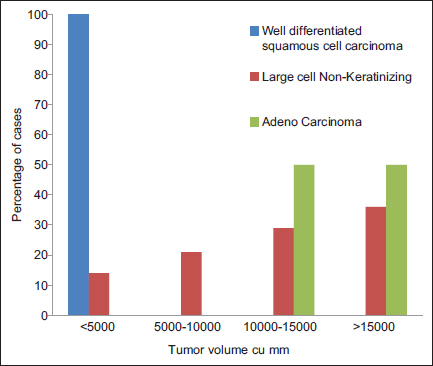
- Graph 4: Correlation of tumor volume with tumor differentiation
Fibronectin
Immunohistochemical staining was done to demonstrate fibronectin in tumors. Moderate intensity and diffuse positivity were observed in tumor cells in cases of WDSCC whereas stroma showed positivity in cases of large cell nonkeratinising types. The tumor cells in these cases showed mild focal or negative staining for fibronectin. Observations indicate that the fibronectin showed a positive correlation with the differentiation of the tumor.
Correlation of fibronectin positivity with tumor volume and lymph node metastasis
Fibronectin positivity within tumors was seen in 55% of cases Figure 9. Of these, only 18% showed metastasis to lymph nodes and 82% did not. Among 12 of the tumors with tumor volume <5000 cumm, 10 (83%) cases showed fibronectin positivity whereas only 2 (17%) out of 12 cases with tumor volume more than 15,000 cumm showed fibronectin positivity Graph 5.
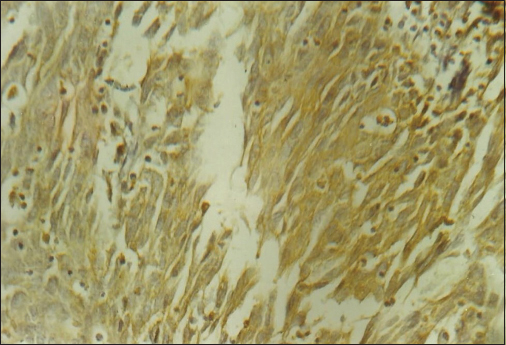
- Diffuse fibronectin positivity within the tumor cells
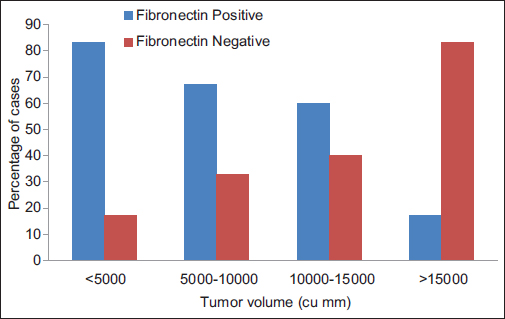
- Graph 5: Correlation of tumor volume with fibronectin positivity
LN5
Immunohistochemical staining using LN5 was done to demonstrate macrophages in tumor infiltrate. One interesting feature in this study is that the macrophages were seen surrounding the groups of tumor cells Figure 10, but their entering into the tumor cell groups is very less, whereas macrophages were seen freely entering into the layers of dysplastic squamous epithelium.
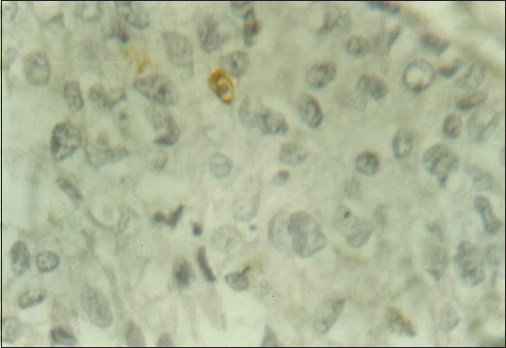
- High power view showing macrophages in close proximity to tumor cells (LN5 immunohistochemistry)
Discussion
Carcinoma of the uterine cervix has been one of the commonest causes of cancer deaths. Unlike other tumors, it can be detected early. The treatment modality is determined by the stage of the disease at the time of diagnosis. Hence, it is highly essential to stage these patients accurately to advise the best treatment to increase their survival. FIGO staging system is effective in predicting the outcome of the disease. However, the disparate prognosis has been observed in patients with tumors in the same stage. Many investigators tried studying various parameters to clear this discrepancy such as pelvic lymph node metastasis,1 tumor size,2 cervical stroma invasion,3 the presence of lymph-vascular space invasion,4 histologic subtype,5 parametrial invasion,6 and corpus invasion7 and each was reported to have prognostic value. Fuller et al.8 found out that after satisfying for nodal metastasis, the size of the primary tumor, the depth of invasion into the cervix and the histologic grade were associated with an increased risk of recurrence. However, it is more appropriate to select factors with independent prognostic significance. Burghardt and Holzer9 claim that bulk or volume of tumor is important in the assessment of prognosis. With this background knowledge, it was planned to study the significance of tumor volume as an independent prognostic factor.
In this study, the tumor volume is compared with lymph node metastasis, parametrial extension, vaginal and uterine corpus involvement. It is evident from the present study that the tumor volume correlates well with lymph node metastasis, parametrial extension, vaginal, and uterine corpus involvement. Tumor volume on fresh specimens was estimated according to Dargent et al.10 According to several investigators, lymph node involvement was considered to be one of the prognostic factors in cervical carcinoma.11,12 Hence, a correlation was made between lymph node metastasis and tumor volume, to see if any importance can be given to tumor volume as an independent prognostic factor in cases of carcinoma cervix. The observations of our study indicate that the tumor shows lymph node metastasis as the tumor volume increases. There is a clear-cut difference between the number of cases with lymph node metastasis grouped under <5000 cumm tumor volume and those with more than 15,000 cumm tumor volume. Because cases are few in number, a detailed distinction of various groups of lymph nodes could not be made. However, in general, there is a similarity between the observations of this study and the study done by Dargent et al.10 Similar correlation was also observed by Baltzer and Koepcke.13 Burghardt and Pickel14 have used the tumor area rather than the tumor volume to correlate with lymph node metastasis and found that it was significant. However, still it is felt that the estimation of the tumor volume will be more appropriate to find the risk cases.
Bleker et al.15 showed the importance of detection of parametrial involvement to stage and plan the treatment of carcinoma of cervix. He showed the significance of parametrial involvement in stage Ib and IIa cases. Hence, in this study, correlation was made between parametrial involvement by the tumor and the tumor volume. In accordance with Burghardt and Pickel,14 in the present study parametrial involvement was observed with an increasing trend in tumors as they increase in volume. There is a clear-cut difference between the number of cases with parametrial involvement grouped under <5000 cumm tumor volume and those with more than 15,000 cumm tumor volume. The smallest tumor volume with parametrial involvement was 3670 cumm. In some of the cases, parametrial involvement was observed microscopically as small tumor deposits in the parametrial tissue around the small vasculature, although they were negative for the tumor involvement on gross examination. This indicates that the tumor involves the parametrium not only by direct spread but also by lymphatic route.
Extension of cervical cancer in the uterine body was associated with a higher incidence of peritoneal carcinomatosis and distant metastasis resulting in decrease survival rates by a factor of 10–20%.7 This finding was observed by Grimard et al.16 who studied tumors belonging to stage Ib. Noguchi et al.17 reported uterine body invasion in 7.8% of stage Ib patients, 25.5% of stage IIa patients and 38.2% of stage IIb patients, indicating increasing incidence of uterine involvement as the stage of disease increases. The observation of the present study was quite in accordance with those of Noguchi. In this study, 43% of stage Ib patients, 50% of cases in stage IIa and 62.5% of stage IIb patients showed uterine involvement. Similar findings were observed with vaginal involvement also. A good correlation was also observed between the tumor volume and histological type of tumor. All the WDSCC had tumor volume <5000 cumm whereas 80% of moderately differentiated and 89% of poorly differentiated carcinomas had tumor volume more than 5000 cumm. All the adenocarcinomas showed tumor volume more than 10,000 cumm. This supports the findings observed by others.18
Fibronectin
Fibronectin has a widespread distribution in vivo and exists in two forms, either in plasma or tissue.19 The antibody used in this study was specific to tissue fibronectin. Kannan et al.20 found that there is a direct correlation between expression of fibronectin and stage of tumor progression. According to the present study and study made by several other investigators10,14 tumor volume was considered to be a significant prognostic indicator, hence correlation was made between fibronectin positivity within the tumor and tumor volume. Though there was not much difference in fibronectin positivity among the tumors with volume from 5000 to 15,000 cumm, yet a significant difference can be observed among tumors with tumor volume <5000 cumm and more than 15,000 cumm. As lymph node metastasis was also considered as a significant prognostic factor in cases of carcinoma of cervix by several investigators,11,12 this was correlated with fibronectin positivity. Observations in the study showed that the fibronectin positivity in the tumors carries more weightage as a prognostic indicator rather than the absence of fibronectin. In conclusion, this study shows that the presence of fibronectin in the tumor can be taken as a prognostic factor. Fibronectin also showed a negative correlation with tumor differentiation.
LN5 (macrophages)
LN-5 a monoclonal antibody which reacts with both normal tissue macrophages and benign neoplasms has been used to identify the presence of macrophages within and around the tumor. Macrophages were seen infiltrating freely into the dysplastic cervical epithelium, whereas they were seen occasionally infiltrating into the groups of tumor cells and lying in close proximity to them, although there were many of them lying surrounding these clusters. This may indicate that there is some inhibition offered to the macrophages by these tumor cells.
Conclusion
Tumor volume can be considered as an independent prognostic factor to assess the spread of the tumor. Cases with tumor volume <5000 cumm show low risk in terms of parametrial involvement and lymph node metastasis and those with tumor volume more than 15,000 cumm are definitely going to behave badly. Second, fibronectin positivity of tumor carries some importance in identifying the low-risk cases. A detailed study on macrophages in neoplasia needs to be carried out to observe whether their presence in the inflammatory infiltrate has positive or negative effect in the tumor spread.
Finally, it can be concluded from the present study that the tumor volume assessment, detection of fibronectin in carcinoma of cervix would give a clear idea regarding the behavior of tumor in vivo. A brief attempt on detection of macrophages in these tumors is just to get an insight into the immunological aspect of these tumors so that further study in aspect can be planned to see whether tumor immunology is related with tumor progression or regression.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The prognostic significance of number of positive nodes in cervical carcinoma stages IB, IIA, and IIB. Cancer. 1990;65:1923-7.
- [Google Scholar]
- Prognostic factors and operative treatment of stages IB to IIB cervical cancer. Am J Obstet Gynecol. 1987;156:988-96.
- [Google Scholar]
- Identification of histopathologic risk groups in stage IB squamous cell carcinoma of the cervix. Obstet Gynecol. 1985;66:569-74.
- [Google Scholar]
- Does adenocarcinoma of uterine cervix have a worse prognosis than squamous carcinoma when treated by radiotherapy? Gynecol Oncol. 1989;33:23-6.
- [Google Scholar]
- Prognostic significance of the depth of invasion relating to nodal metastases, parametrial extension, and cell types. A study of 628 cases with Stage IB, IIA, and IIB cervical carcinomaCancer. 1984;54:3035-42.
- [Google Scholar]
- Endometrial extension of carcinoma of the uterine cervix: A prognostic factor that may modify staging. Cancer. 1981;48:170-80.
- [Google Scholar]
- Lymph node metastases from carcinoma of the cervix, stages IB and IIA: Implications for prognosis and treatment. Gynecol Oncol. 1982;13:165-74.
- [Google Scholar]
- Diagnosis and treatment of microinvasive carcinoma of the cervix uteri. Obstet Gynecol. 1977;49:641-53.
- [Google Scholar]
- V factor (tumor volume) and T factor (FIGO classification) in the assessment of cervix cancer prognosis: The risk of lymph node spread. Gynecol Oncol. 1985;22:15-22.
- [Google Scholar]
- Pelvic lymphnodectomy following radiation in cervical carcinoma. Am J Obstet Gynecol. 1964;88:932-43.
- [Google Scholar]
- The prognostic significance of the size of the largest nodes in metastatic carcinoma from the uterine cervix. Gynecol Oncol. 1984;19:187-93.
- [Google Scholar]
- Tumor size and lymph node metastases in squamous cell carcinoma of the uterine cervix. Arch Gynecol. 1979;227:271-8.
- [Google Scholar]
- Local spread and lymph node involvement in cervical cancer. Obstet Gynecol. 1978;52:138-45.
- [Google Scholar]
- The significance of microscopic involvement of the parametrium and/or pelvic lymph nodes in cervical cancer stages IB and IIA. Gynecol Oncol. 1983;16:56-62.
- [Google Scholar]
- Prognostic significance of endometrial extension in carcinoma of the cervix. Gynecol Oncol. 1988;31:301-9.
- [Google Scholar]
- Uterine body invasion of carcinoma of the uterine cervix as seen from surgical specimens. Gynecol Oncol. 1988;30:173-82.
- [Google Scholar]
- Primary adenocarcinoma of the uterine cervix. A clinical studyCancer. 1983;52:942-7.
- [Google Scholar]
- Alterations in expression of basement membrane proteins during tumour progression in oral mucosa. Histopathology. 1994;24:531-7.
- [Google Scholar]







