Translate this page into:
Digital Mapping of a Massive Skull-Base Ameloblastoma with Intracranial Extension, Resection, and Reconstruction Using 3D Templates and Molds: Descriptive Case Report and Review
Address for correspondence Akash Menon, MDS, BDS, Department of Surgical Oncology, Balco Medical Centre, Naya Raipur, Chhattisgarh, India – 493661drakashmenon@gmail.comakashmenon17@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Radical surgery is the mainstay for the treatment of recurrent ameloblastomas; however, it leads to large, complex defects. In this case report, we present an innovative technique of digitally aided resection and reconstruction. A massive histologically confirmed acanthomatous ameloblastoma of the skull-base was digitally mapped with the help of three-dimensional (3D) computed tomography and a custom resection template was fabricated. Digital resection of the skull-base tumor with intracranial extension was done virtually and the resultant defect was reconstructed to create an anatomical replica of the contralateral unaffected side. The tumor was successfully resected with adequate margins guided by the resection template to avoid injury to adjacent vital structures. Subsequent reconstruction was performed by first adapting polymethyl methacrylate bone cement into a series of custom-made 3D molds. Once set, this bone cement served as a reconstructive implant to bridge the ablative defect. The implant offered a precise fit and was secured to healthy adjacent bone using titanium microplates. We present a 6-month follow-up of the case with satisfactory aesthetic results. 3D printing technology has the potential to revolutionize the arena of craniofacial resection with excellent cosmesis and no donor site morbidity if applied appropriately as described here.
Keywords
skull-base tumor
ameloblastoma
virtual surgical planning
3D printing
cranial reconstruction
odontogenic tumor
Introduction
Reconstruction of a large skull and facial bone defects is one of the most demanding challenges for craniofacial surgeons. Reconstruction of craniofacial bones with hard tissue have good clinical outcomes with a documented success rate.1 However, various alloplastic materials have been employed for the same with varying results.2 Synthetic materials not only avoid donor site morbidity and scars but also decrease hospital stay, lower expenses, and is of a known composition with predictable results.1 With the help of three-dimensional (3D) printing technology, in this case a resection template was fabricated using polyether ether ketone (PEEK) and a series of molds were made using polylactic acid (PLA). These PLA molds were used to construct bone cement implants ex vivo (DePuy CMW 1 Gentamicin Bone Cement, DePuy Synthes, Indiana, United States) that were secured to the defect margins.
Case Report
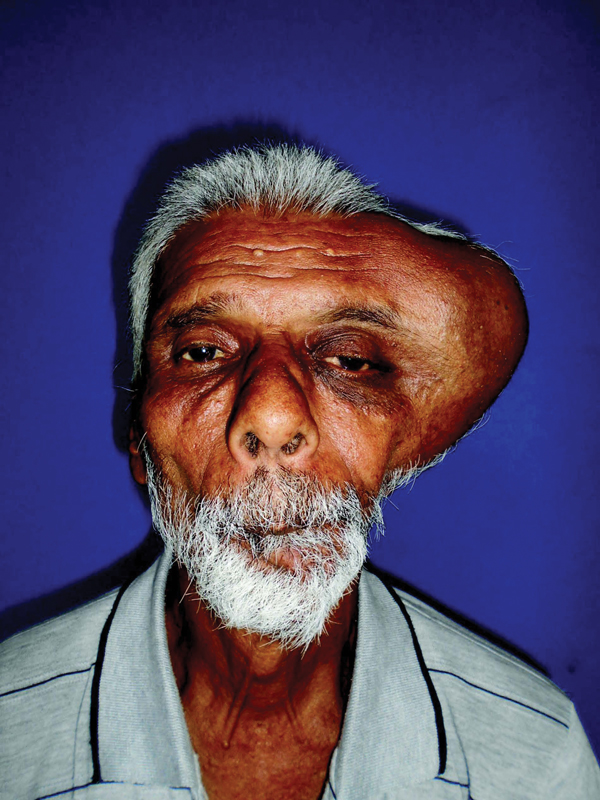
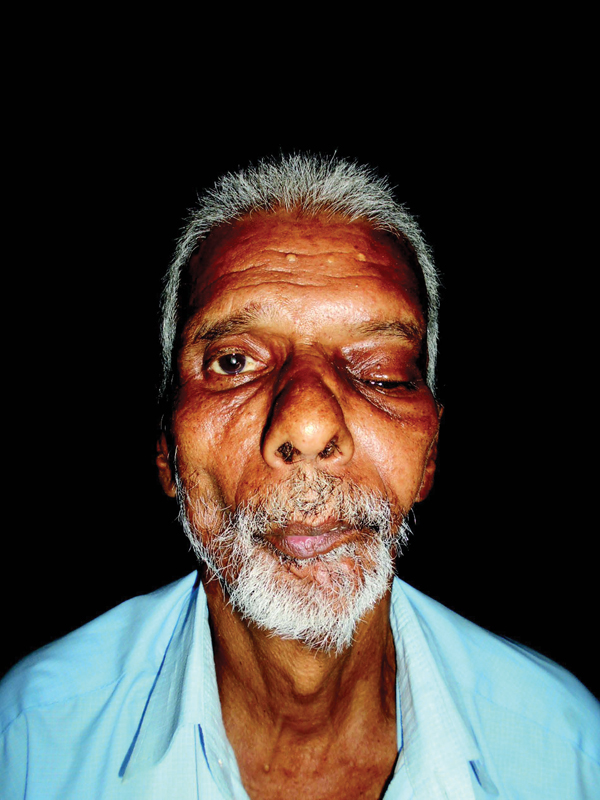
A 65-year-old male patient reported to the department of craniofacial surgery complaining of a swelling on the left side of his face for the last 2 years (Fig. 1). During anamnesis, the patient reported having already undergone four surgeries in the region due to recurrence of a similar lesion. Clinically, the patient had gross facial asymmetry on the left side due to a single diffuse swelling over the left frontotemporoparietal region measuring 10 × 11 × 11 cm that extended inferiorly up to the level of the maxillary buttress and superiorly till the level of the parietal bone, 5 cm lateral to the sagittal suture. Anteriorly, the lesion extended till the lateral border of the supraorbital rim, involving the lateral orbital rim and the zygoma. Laterally, the mass had formed a bulge with stretching of the pericranial soft tissue. Superomedially, the lesion had invaginated into the left orbit causing proptosis and inferior displacement of the globe with complete loss of vision. Posteriorly, the lesion extended up to the preauricular region displacing the tragus. The edges appeared indistinct and the skin over the swelling appeared glossy with Peau-D̀Orange changes. On palpation, the swelling was nontender but firm in consistency.
-
Fig. 1 Preoperative frontal view photograph.
Computed tomographic (CT) findings were reported as a large multiloculated cystic lesion with thick enhancing walls, thick/thin septations, and having a solid component in the left masticator space. It had extensions into the temporoparietal region with extensive erosion of the zygoma, the zygomatic arch, and the frontal, parietal, and squamous temporal bones. It had minimal involvement of the petrous temporal bone in the region of the auditory meatus. The lateral wall of the left orbit was eroded with displacement of the globe. The intracranial extension showed an extra-axial mass in the frontotemporoparietal region that resulted in the displacement of the adjacent neuroparenchyma, which caused a mass effect with midline shift.
A preliminary biopsy was suggestive of recurrent acanthomatous ameloblastoma.
Routine blood investigations and radiographs were done to rule out systemic diseases and metastasis. Patient was scheduled to undergo a radical resection of the lesion, and after deliberation over reconstructive options, it was decided that a custom-made implant would be used to restore the resultant defect.
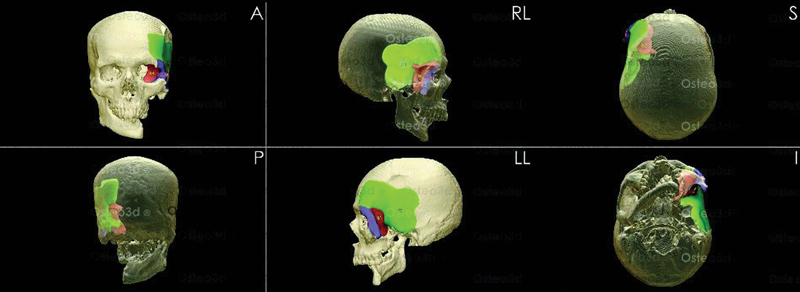
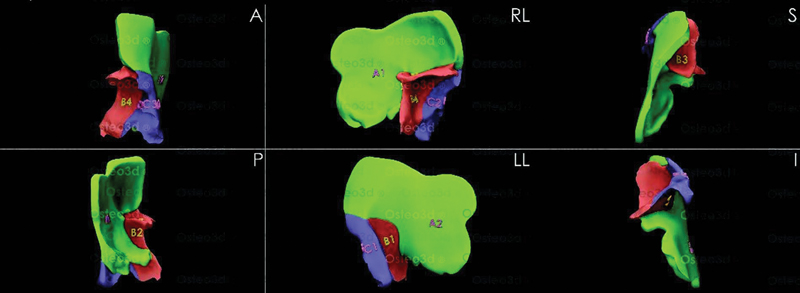
The DICOM files of the CT scan were shared with Osteo3d, a company specializing in patient-specific solutions through digital integration (Osteo3d, Bangalore, India. www.osteo3d.com). The tumor was mapped in detail and digital 3D models were created. The resection areas were marked ensuring safe margins (1 cm in the petrous temporal bone and 1.5 cm in the other areas) and a resection template was fabricated using PEEK. After digitally resecting the tumor on the computer model, a mirror image from the contralateral side (accounting for the corresponding thickness of bone) was used to customize an anatomically accurate replica to bridge the defect (Fig. 2). Considering the inherent undercuts and overhangs of the facial bones, the inner and outer contours of the digital reconstruction were used to make a series of molds by 3D printing using PLA (Fig. 3). The reconstruction pattern was divided into three sections with separate molds for each. These molds were used for shaping the bone cement to fit the ablative defect.
-
Fig. 2 Virtually planned reconstruction of defect.
-
Fig. 3 Digitally aided fabrication of three-dimensional molds.
A temporoparietal hemicoronal incision was used to elevate a pericranial flap. The resection template (Fig. 4) was placed around the tumor once exposed and the bone was osteotomized with a reciprocating saw. “En bloc” resection was performed with margins as per the template. The part of dura matter that was infiltrated by the lesion was carefully excised. The lesion around the globe was excised by creating a plane around the extraocular muscles and preserving the optic nerve.
-
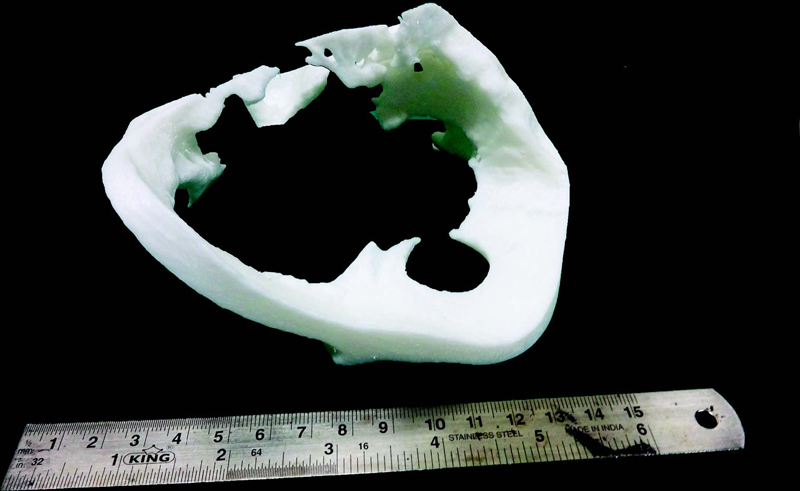
Fig. 4 Custom-made resection template.
The dural defect was repaired using fascia lata to obtain a watertight seal. Reconstruction of the resultant defect was done by shaping the bone cement using the PLA molds (Fig. 5). The inner surfaces of the molds were coated with a separating medium and the bone cement was mixed until it reached the “dough stage.” Then the cement was divided into three parts and kneaded into the molds that were closed tight and locked. Once the final setting strength had been achieved, the molds were tapped open. The complex sections of cement were checked for defects. The various fragments (the roof, floor, and lateral wall of the orbit; the squamous temporal and parietal bones; and the zygomatic arch) were noted to correctly fit the defect and were stabilized with microplates to the bony margins and to each other.

-
Fig. 5 Three-dimensional molds for bone cement implant fabrication.
The patient is currently on regular follow-up and presented for his 6-month follow-up recently (Fig. 6). In the postoperative period, left eyelid ptosis and restricted extraocular eye movements were noted. However, the patient's vision showed a surprising improvement and at present has a vision score of 6/24.
-
Fig. 6 Postoperative frontal view photograph.
Discussion
The recurrence of an ameloblastoma may be attributed to inadequate excision and/or the spread of residual tumor fragments into adjacent bone.3 In our patient, the multiple recurrences (4 times) are easy to explain as the tumor cells might have spread to the frontotemporal region through the retraction of masticatory muscles in the region.
Ameloblastomas, although benign, are relentlessly infiltrative.4 Radical surgical excision is the most appropriate treatment for recurrent ameloblastoma.5 Since the margins of the tumor in our patient were abutting the brain and other vital structures, we restricted our margins to 1.5 cm (1 cm in the petrous temporal bone), clearly demarcated within the resection template. Hearing, balance, and the facial movements remained unaffected in the postoperative period. The most surprising feature was recovery of the vision; however, in the presence of complete ptosis and ophthalmoplegia, this is of limited value.
3D printing technology has been a subject of great interest to reconstructive surgeons since it was first demonstrated in 1986. Its popularity stems from its unique ability to recreate complex anatomical structures with high precision.6
Using digital mapping to plan the excision helped us navigate through areas with potential risk of damage to crucial structures and the use of a resection template allowed accurate transfer of digitally planned resection into the surgical setting.
As the postresection defect was large and complex, involving multiple craniofacial bones, direct shaping of an implant would have been difficult. A custom-made bone cement implant helped us overcome this challenge. The bone cement was adapted in the mold, ex vivo to avoid tissue damage due to its exothermic setting reaction. The mold was designed to have self-retaining locking system that ensured precise form to the bone cement implant without the need for intraoperative manipulation.
An ideal cranial reconstructive material must be durable and have a low host rejection rate.7 Bone cement fulfils these criteria while also being more economical and having less stress-shielding effect than titanium.8
Conclusion
Reconstruction in cases of large craniofacial defects is always challenging. Using 3D printing technology for the creation of patient-specific reconstruction tools, it is possible to achieve excellent results while minimizing cost, time, intraoperative manipulation, and hardware failure. This case proved that using bone cement for reconstruction of craniofacial defects with the help of PEEK resection template and PLA molds is a convenient technique with numerous advantages.
Conflict of Interest
None declared.
References
- Novel composite implant in craniofacial bone reconstruction. Eur Arch Otorhinolaryngol. 2012;269(02):623-628.
- [Google Scholar]
- Reconstruction of large cranial defect with alloplastic material (bone cement-cold cure polymethyl-methacrylate resin) J Maxillofac Oral Surg. 2010;9(02):191-194.
- [Google Scholar]
- Ameloblastoma of the acanthomatous and plexiform type in the mandible presenting as a unilocular radiolucency. Indian J Oral Sci. 2015;6(01):34.
- [Google Scholar]
- A histologic variant of ameloblastoma: the acanthomatous type. Méd Buccale Chir Buccale. 2016;22(01):55-57.
- [Google Scholar]
- Acanthomatous ameloblastoma: a clinical rarity. J Indian Acad Oral Med Radiol. 2014;26(02):200.
- [Google Scholar]
- Three-dimensional printing in maxillofacial surgery: hype versus reality. J Tissue Eng. 2018;9:2041731418770909.
- [Google Scholar]
- Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus. 2009;26(06):E10.
- [Google Scholar]
- Cranioplasty and craniofacial reconstruction: a review of implant material, manufacturing method and infection risk. Appl Sci (Basel). 2017;7(03):276.
- [Google Scholar]







