Translate this page into:
Comparison of setup errors between two immobilization techniques for image-guided pelvic radiotherapy: Can an ankle fixator be used as an alternative to a thermoplastic mask for immobilization without compromising treatment?
Corresponding author: Dr. Alakananda Choudhury, Department of Radiotherapy, IPGME&R and SSKM Hospital, Kolkata, India. drachoudhury80427@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ghosh A K, Roy N, Chhatui B, Biswas J, Choudhury A, Chakraborty I, et al. Comparison of setup errors between two immobilization techniques for image-guided pelvic radiotherapy: Can an ankle fixator be used as an alternative to a thermoplastic mask for immobilization without compromising treatment? Asian J Oncol. 2024;10:3. doi: 10.25259/ASJO_30_2023
Abstract
Objectives
Pelvic malignancies have reported large setup variations, requiring good treatment positioning and immobilization. Various immobilization techniques have been reported in literature for pelvic malignancies. In this study, two different immobilization techniques have been compared for translational setup errors during radiation delivery.
Material and Methods
Kilovoltage cone-beam computed tomography (kV CBCT) scans were taken and 3D-3D matching was done during the first three days of radiation treatment; thereafter once a week, and as per requirement of the particular treatment. Data on translational shifts was tabulated from treatment record. The mean and standard deviation of all individual shifts were calculated using descriptive statistics. The means of the translational shifts of the two arms were compared using Mann–Whitney U test. The population’s systematic and random errors were calculated. Clinical target volume to planning target volume (CTV-PTV) margins were calculated using Van Herk’s method.
Results
A total of 855 cone-beam computed tomography (CBCT) scans were analyzed. The mean setup errors were not significantly different between two arms in all three translational axes. The CTV-PTV margins in the anteroposterior, superoinferior, and lateral directions are 0.59, 0.94, and 0.78 cm for the TPI arm and 0.84, 0.92, and 0.87 cm for the AFI arm. To have a uniform CTV-PTV margin in all directions, the minimum expansion required is 0.94 cm and 0.92 cm in the TPI and AFI arm, respectively.
Conclusion
An ankle fixator or similar lower leg immobilization technique can be used as an alternative to thermoplastic mask immobilization without compromising setup accuracy. This has the potential to reduce treatment cost per patient, by excluding the cost of thermoplastic mask.
Keywords
Immobilization
Setup errors
Pelvic radiotherapy
INTRODUCTION
Radiotherapy of solid tumors has moved from conventional two-dimensional (2D) techniques to conformal and intensity-modulated radiotherapy (IMRT) with image guidance.[1] IMRT leads to highly conformal dose delivery to target volume with rapid dose fall off beyond the target, which reduces dose to surrounding organs at risk (OAR).[2,3] However, it carries a higher chance of target miss, leading to treatment failure.[4] Target miss can occur due to errors during treatment preparation (positioning, immobilization, CT simulation), treatment execution (patient setup during radiation delivery), and internal organ motion during treatment.[5-7] To compensate for the above, a planning target volume (PTV) margin is added over the clinical target volume (CTV), and image verification is done during treatment delivery for highly conformal radiotherapy techniques.[8,9]
A large PTV margin leads to increased irradiation of surrounding OARs. Various methods are implemented to reduce the PTV margin without compromising target failure, like rigid immobilization with a thermoplastic mask, respiratory motion management, and image verification of patient setup during treatment delivery.[10] Image verification is usually done by onboard imaging (OBI) attachments on linear accelerator (LINAC) like kilovoltage/megavoltage (kV/MV) X-rays or Cone-beam Computed Tomography (CBCT).[11]
Pelvic malignancies have reported large setup variations, thus requiring good treatment preparations, including positioning and immobilization.[12,13] Various pelvic immobilization techniques have been reported in literature like thermoplastic mask, vacuum cushion, knee wedge, ankle fixator[13–16]. Our institution uses multiple techniques based on physician preference. Use of ankle fixator or knee wedge rather than thermoplastic mask reduces treatment cost and may decrease setup time, and thus, overall treatment time. In this study, we have compared two immobilization techniques for translational setup errors during radiation delivery- thermoplastic mask and ankle fix immobilization.
MATERIAL AND METHODS
Objectives
To compare translational mean setup errors produced by two immobilization techniques.
To compute CTV-PTV margins required for these techniques.
Patient Selection
This is a retrospective cohort study. All patients visiting the outpatient department (OPD) from 2018 to 2021 with biopsy-proven pelvic malignancy, were selected for the study, provided they met the inclusion and exclusion criteria. Patients with diagnosed carcinoma of the cervix, bladder, rectum, prostate, endometrium were selected for the study. Those with carcinoma of anal canal, bone or soft tissue sarcoma, any immobilization done in the prone position, immobilization techniques other than the aforementioned, and any palliative intent radiotherapy-were excluded. Ethical clearance had been obtained from the Institutional Ethics Committee.
Protocol of Positioning and Immobilization
All patients were simulated in the supine position using one of the immobilization techniques based on physician preference. Carbon fiber base plate with extension, appropriate headrest, armrest, and hand grip pole was common to all patients, who were divided into two arms:
Thermoplastic mask immobilization (TPI) - 4 clamp thermoplastic mask was used for immobilization.
Ankle fix immobilization (AFI) - No thermoplastic mask used. An ankle fix was used, which would immobilize the legs and ankle, maintaining separation between lower limbs [Figures 1 and 2].

- Ankle fixation device

- Lateral view showing patient setup with ankle fixation device for pelvic immobilization
CT Simulation and Treatment Planning
CT scans were taken using protocols for individual subsite. Intravenous contrast material (Iohexol), at 1ml/kg, with a maximum dose of 70 mg, was used on provision of informed consent. Scans were taken from 10 cm above the umbilicus to mid-thigh using a Philips Brilliance Big bore CT simulator (Varian Medical Systems, Palo Alto, California). Simulation scans were verified by radiation oncologist and physicist. if any rotational component was found, repeat scans were taken.
Scans were transferred to Eclipse treatment planning system (Varian Medical Systems, Palo Alto, California); contouring was done using appropriate guidelines for a specific subsite. Treatment planning was done mostly by 3DCRT (3-dimensional conformal radiotherapy) or IMRT technique.
Patient Setup and Image Verification
Our institute has a Varian Truebeam Linear Accelerator equipped with a couch, capable of 6 degrees of movement (Translational: vertical, longitudinal, lateral; Rotational: roll, pitch, rotation). This can correct setup errors in six dimensions.
KV CBCT is most commonly used for setup verification and image-guided radiotherapy (IGRT) for pelvic subsites at our institute.
On the treatment day, the patient is set up on LINAC couch with the same immobilization method(s) as prepared during simulation by matching skin/thermoplastic mask tattoos with external room lasers. Translational shifts are applied to match treatment with machine isocenter. KV CBCT is taken using pelvis imaging protocol with standard reconstruction. Translational setup error is calculated by registration of reconstructed and planned CT data sets using bony anatomy; rotational errors are not implemented for setup correction, according to institutional protocol.
KV CBCT scans are taken, and 3D-3D matching is done before radiation delivery, on the first three days of treatment; thereafter, once a week, and, as and when required.
Data Collection and Statistical Analysis
Data on patient particulars and immobilization techniques were collected from patient records. Data on translational shift was tabulated from treatment records. According to convention, lateral, longitudinal, and vertical shifts have been denoted as X, Y, Z shifts respectively. The mean and standard deviation of all individual shifts were calculated using descriptive statistics. Means of translational shifts of two arms were compared using Mann Whitney U test. Population systematic and random errors were calculated according to the literature of the Royal College of Radiologists, Institute of Physics and Engineering in Medicine, Society and College of Radiographers’ “On target: ensuring geometric accuracy in radiotherapy.”
Systematic Error
Individual patient mean setup error- Sum of setup error for one translational error for each verification image divided by number of images for that patient.
Population mean setup error- Overall mean for one translational error for the whole patient group; ideally should be 0.
Population Systematic error (Σ)- Standard deviation of individual mean setup errors about the overall population mean error.
Random Error
Individual random error- Standard deviation of setup errors around the individual mean error.
Population random error (σ)- Mean of individual random errors.
There are several recipes for calculation of CTV-PTV margins: for our study, Van Herk’s method has been considered; according to which, PTV margin= 2.5 Σ + 0.7 σ, where Σ and σ are population systematic and random errors respectively.[5]
Results
The basic characteristics of patients, immobilization, and the treatment technique has been described in Table 1. Most patients were treated with 3DCRT (54.9%) followed by IMRT (42.7%). Carcinoma cervix was the most commonly treated malignancy in the study population (45.1%). A total of 82 patients were included, 35 in TPI and 47 in AFI arm.
| Characteristics | n = 82 | |
|---|---|---|
| Median age | 58 years (Minimum 30, maximum 89 years) | |
| Sex | Male | 37 (45.1%) |
| Female | 45 (54.9%) | |
| Primary site | Cervix | 37 (45.1%) |
| Prostate | 19 (23.2%) | |
| Rectum | 14 (17.1%) | |
| Bladder | 6 (7.3%) | |
| Endometrium | 6 (7.3%) | |
| Radiation technique used | 3DCRT | 45 (54.9%) |
| IMRT | 35 (42.7%) | |
| VMAT | 2 (2.4%) | |
| Immobilization | 4-clamp thermoplastic mask | 35 (42.7%) |
| Ankle fixator with no mask | 47 (57.3%) | |
| Total number of scans taken | 855 | |
3DCRT: 3-dimensional conformal radiotherapy, IMRT: Intensity modulated radiotherapy, VMAT: volumetric modulated arc therapy
855 CBCT scans were analyzed. Average setup error for an individual patient is shown in Figure 3. Mean setup errors were 0.031 ± 0.23 cm, 0.079 ± 0.26 cm, 0.021 ± 0.20 cm in lateral (X), longitudinal (Y), vertical (Z) directions respectively [Table 2]. The corresponding population systematic errors (Σ) and random errors (σ) were 0.226, 0.257, 0.201 cm and 0.401, 0.419, 0.407 cm respectively. Overall calculated CTV-PTV margins: 0.78 cm in antero-posterior direction, 0.93 cm in supero- inferior direction, and 0.85 cm in lateral direction. To create a uniform CTV-PTV margin, at least 0.93 cm of margin is required all around the CTV.
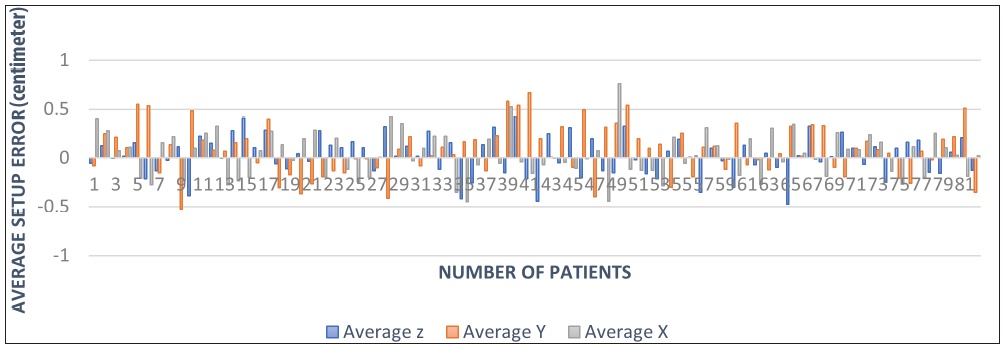
- Distribution of average translational errors for individual patients.
| Translational axis | Mean error (cm) | Standard deviation (cm) | Population Systematic error (Σ) | Population Random error (σ) | CTV-PTV margins (cm) |
|---|---|---|---|---|---|
| Vertical (Z) | 0.0214 | 0.2006 cm | 0.2006 | 0.4071 | 0.78 |
| Longitudinal (Y) | 0.0792 | 0.2576 cm | 0.2576 | 0.4188 | 0.93 |
| Lateral (X) | 0.0313 | 0.2265 cm | 0.2265 | 0.4014 | 0.85 |
CTV: Clinical Target Volume, PTV: Planning Target Volume
Mean setup errors were not significantly different between the arms in all three translational axes, as compared by Mann Whitney U test (p = 0.729, 0.097, 0.548 for X, Y, Z shifts respectively) [Table 3]. Systematic, random errors and CTV-PTV margins for individual translation shifts between two arms have been tabulated in Table 3. The margins for TPI arm in antero-posterior, supero-inferior, lateral directions were 0.59, 0.94, 0.78 cm respectively. Corresponding margins for AFI arm were 0.84, 0.92, 0.87 cm respectively. To have a uniform CTV-PTV margin in all directions, minimum expansion required is: 0.94 cm and 0.92cm in TPI and AFI arm respectively.
| TPI arm | AFI arm | P value | ||
|---|---|---|---|---|
| Vertical (Z) | Mean error (cm) | 0.0339 | 0.0176 | 0.548 |
| Σ | 0.1515 | 0.2140 | ||
| σ | 0.3044 | 0.4380 | ||
| CTV-PTV margin (cm) | 0.59 | 0.84 | ||
| Longitudinal (Y) | Mean error (cm) | -0.0090 | 0.1058 | 0.097 |
| Σ | 0.2473 | 0.2576 | ||
| σ | 0.4742 | 0.4021 | ||
| CTV-PTV margin (cm) | 0.94 | 0.92 | ||
| Lateral(X) | Mean error | 0.0425 | 0.0280 | 0.729 |
| Σ | 0.2100 | 0.2328 | ||
| σ | 0.3619 | 0.4134 | ||
| CTV-PTV margin (cm) | 0.78 | 0.87 | ||
| Maximum PTV margin in all directions | 0.94 cm | 0.92 cm | ||
TPI: thermoplastic mask immobilization, AFI: Ankle fix immobilization, Σ: population systematic error, σ: population random error, CTV: Clinical Target Volume, PTV: Planning target volume, All bold values in the above table indicate the CTV-to-PTV margin (in centimeter), which is of interest in this study.
TPI arm had significantly more longitudinal setup errors greater than 0.5 cm (38.5% vs. 27.9%, p 0.003), while, AFI arm had significantly more vertical setup errors, with values greater than 0.5 cm [Figure 4].
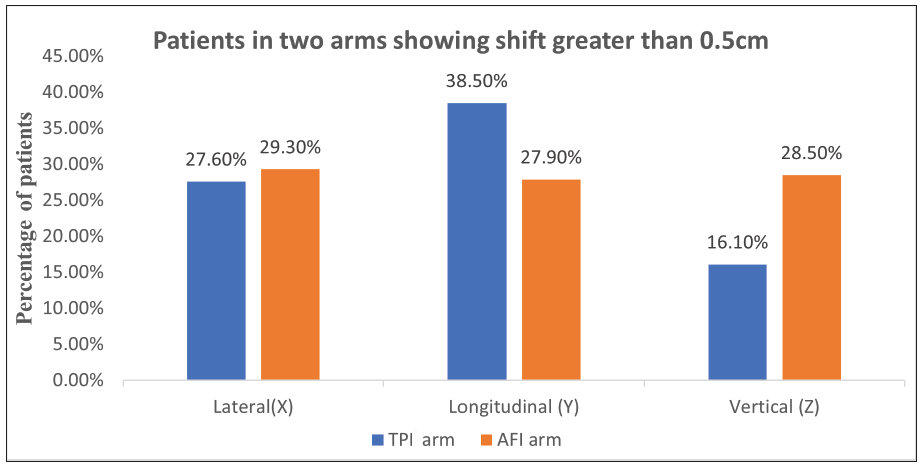
- Clustered column chart showing the distribution of patients in arms with a shift of greater than 0.5 cm. TPI: Thermoplastic mask immobilization, AFI: Ankle fix immobilization
The trend of overall CTV-PTV margins have decreased from 2018–2021 with symmetrical CTV-PTV margins; and were calculated to be 1.07, 0.93, 0.76 cm in 2018, 2019, and 2021 respectively (2020 not considered as very few patients had been treated here during early part of the COVID pandemic) [Table 4].
| Year of treatment | Systematic errors (Σ) | Random errors (σ) | CTV-PTV margins (cm) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| X | Y | Z | X | Y | Z | X | Y | Z | |
| 2018 | 0.23 | 0.30 | 0.25 | 0.16 | 0.47 | 0.49 | 0.7 | 1.07 | 0.97 |
| 2019 | 0.23 | 0.26 | 0.20 | 0.16 | 0.40 | 0.46 | 0.7 | 0.93 | 0.82 |
| 2021 | 0.20 | 0.19 | 0.16 | 0.16 | 0.40 | 0.28 | 0.61 | 0.76 | 0.62 |
CTV: Clinical target volume, PTV: Planning target volume.
DISCUSSION
Immobilization for irradiation of pelvic malignancies has been a matter of debate, and many trials have tried to find an optimal immobilization that would improve reproducibility.[12-15] Cost effectiveness is also important, especially in centers depending on state funds for patient treatment. Major problems with pelvic immobilization and setup include: significant mobility at hip joint, regular realignment if skin marks are placed, variable rectal and bladder filling, and significant pelvic rotation.[14,16]
Although the use of thermoplastic mask negates the problem of skin mark alignments, the device is difficult to reuse. Thus, a new mask is required for every patient. In contrast, using simpler devices like ankle fixator requires placement of skin tattoos, and can be reused. Therefore, such a device per treatment room, can be used to treat all patients requiring pelvic irradiation, eventually reducing cost by reducing the wastage of thermoplastic masks.
In this study, 4-clamp thermoplastic mask and ankle fix immobilization, have been compared for setup errors and CTV-PTV margins. No significant difference has been reported between mean setup errors using the above mentioned techniques, with similar symmetrical CTV-PTV expansion. Setup errors of pelvic radiotherapy for various immobilization techniques [Table 5] have been reported in the literature.[12,14,17,18] Two studies have compared thermoplastic mask immobilization with non-rigid versus no immobilization like ankle fixator and vacuum bag.[12,14] Anand et al. reported no difference in mean errors between the thermoplastic mask and knee wedge, with similar CTV-PTV expansion.[14] Udayshankar et al.[12] reported no immobilization (use of leg separator) to be most reproducible, with a symmetrical CTV-PTV margin of 0.47 cm. Systematic and random errors were lowest with no immobilization, while random error was highest using thermoplastic masks. Patni et al. reported a CTV-PTV expansion of 1.03 cm for thermoplastic mask/skin marking, which was comparable to this study.[17] However, a study comparing three immobilization devices for prostate radiotherapy, reported thermoplastic mask to have the most reproducible immobilization with minimum setup errors compared to alpha cradle or leg cushion.[19]
| Systematic error (Σ) | Random error (σ) | CTV-PTV margin | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ML(X) | SI(Y) | AP(Z) | ML(X) | SI(Y) | AP(Z) | ML(X) | SI(Y) | AP(Z) | ||
| Anand et al.[14] | ORFIT | 0.24 | 0.48 | 0.27 | 0.31 | 0.60 | 0.4 | 0.91 | 1.45 | 1.23 |
| Knee wedge | 0.26 | 0.48 | 0.37 | 0.38 | 0.37 | 0.45 | 0.81 | 1.62 | 0.95 | |
| Udayshankar et al.[12] | Thermoplastic Mask | 0.169 | 0.257 | 0.169 | 0.401 | 0.415 | 0.209 | 0.703 | 0.932 | 0.568 |
| Vacuum bag | 0.255 | 0.156 | 0.484 | 0.392 | 0.273 | 0.257 | 0.911 | 0.581 | 1.39 | |
| Leg separator | 0.13 | 0.139 | 0.141 | 0.189 | 0.175 | 0.151 | 0.456 | 0.469 | 0.459 | |
| Patni et al.[17] | Thermoplastic mask/skin mark | 0.19 | 0.35 | 0.20 | 0.13 | 0.23 | 0.12 | 0.57 | 1.03 | 0.58 |
| Present study | TPI arm | 0.21 | 0.25 | 0.15 | 0.36 | 0.47 | 0.30 | 0.78 | 0.94 | 0.59 |
| AFI arm | 0.23 | 0.26 | 0.21 | 0.41 | 0.40 | 0.44 | 0.87 | 0.92 | 0.84 | |
All measurements in cm, rounded to 2 or 3 decimals. CTV: Clinical target volume, PTV: Planning target volume Patients in two arms showing shift greater than 0.5 cm, ML: medio-lateral (direction), SI: supero-inferior (direction), AP: antero-posterior (direction), ORFIT: brand name for thermoplastic mask immobilization device, TPI : Thermoplastic mask Immobilization, AFI: Ankle Fix Immobilization.
Our study has shown a significantly higher individual setup error of >0.5 cm in supero-inferior (Y) direction in TPI arm (38.5%) and antero-posterior direction in AFI arm (28.5%). This probably has influenced the CTV-PTV expansion in TPI arm in supero-inferior direction, which is largest among 6 reported CTV-PTV expansion in this study (0.94 cm). Saini et al. and White et al. have reported maximum individual setup errors in supero-inferior direction of 23.38% and 23.6% respectively, with the use of 4-clamp pelvic thermoplastic mask, similar to our study.[15,20] Maximum CTV-PTV expansion in this study was in supero-inferior direction in both arms, similar to many studies, that have reported a maximum CTV-PTV expansion in the superoinferior direction, ranging between 0.83–1.62 cm.[14,15,17,20]
This study has several limitations: small sample size, small number of CBCT scans ,and only inter-fractional deviations being evaluated. Separate reports comparing immobilization techniques for individual sites of pelvic malignancy, are required, to validate the above findings. However, from the above results, it may be concluded that an ankle fixator or similar lower leg immobilization technique can be used as an alternative to thermoplastic mask immobilization, without compromising setup accuracy.
CONCLUSION
An ankle fixator or similar lower leg immobilization technique can be used as an alternative to thermoplastic mask immobilization without compromising setup accuracy. This has the potential to reduce treatment costs per patient by excluding the cost of thermoplastic masks.
Acknowledgement
The authors would like to thank all the Department of Radiotherapy, Medical College and Hospital, Kolkata staff.
Ethical approval
The research/study approved by the Institutional Review Board at Medical College and Hospital, Kolkata, number MC/KOL/IEC/NON-SPON/1534/09/2022, dated 26/09/2022.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial Support and Sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Advances in Radiation Therapy: Conventional to 3D, to IMRT, to 4D, and beyond. CA Cancer J Clin. 2005;55:117-34.
- [CrossRef] [PubMed] [Google Scholar]
- Intensity-modulated radiotherapy—what is it? Cancer Imaging. 2004;4:68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Volumetric modulated arc therapy: a review of current literature and clinical use in practice. Br J Radiol. 2011;84:967-96.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Precautions in the use of intensity-modulated radiation therapy. Technol Cancer Res Treat. 2005;4:203-10.
- [CrossRef] [PubMed] [Google Scholar]
- Errors and margins in radiotherapy. Semin Radiat Oncol. 2004;14:52-64.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of patient preparation strategies to manage internal organ motion during radiotherapy in the pelvis. J Radiother Pract. 2020;19:182-9.
- [CrossRef] [Google Scholar]
- Evaluation of setup errors in conformal radiotherapy for pelvic tumours: Case of the Regional Center of Oncology, Agadir. Radiat Med Prot. 2020;1:99-102.
- [CrossRef] [Google Scholar]
- Définition des volumes en radiothérapie externe : rapports ICRU 50 et 62. Cancer/Radiothérapie. 2001;5:472-8.
- [CrossRef] [Google Scholar]
- Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report. Radiother Oncol. 2002;64:75-83.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction of margins in external beam radiotherapy. J Med Phys Assoc Med Phys India. 2008;33:41-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Image Guidance in Radiation Therapy: Techniques and Applications. Radiol Res Pract. 2014;2014:705604.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Immobilization versus no immobilization for pelvic external beam radiotherapy. Rep Pract Oncol Radiother. 2018;23:233-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A comparison between two different immobilization devices for radiation therapy treatment of pelvic cancer using VMAT. J Med Imaging Radiat Sci. 2021;52:238-47.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of thermoplastic masks and knee wedge as immobilization devices for image-guided pelvic radiation therapy using Cone Beam Computed Tomography. Indian J Cancer. 2020;57:182.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison between four immobilization systems for pelvic radiation therapy using CBCT and paired kilovoltage portals based image-guided radiotherapy. J Cancer Res Ther. 2014;10:932-6.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of four patient immobilization devices in the treatment of prostate cancer patients with three dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 1996;34:213-9.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of three-dimensional setup errors in image-guided pelvic radiotherapy for uterine and cervical cancer using kilovoltage cone-beam computed tomography and its effect on planning target volume margins. [accessed 2022 Sep 13]. https://www.cancerjournal.net/article.asp?issn=0973-1482;year=2017;volume=13;issue=1;spage=131;epage=136;aulast=Patni.
- [Google Scholar]
- Estimation of setup uncertainty using planar and MVCT imaging for gynecologic malignancies. Int J Radiat Oncol Biol Phys. 2008;71:1511-7.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective comparison of three systems of patient immobilization for prostate radiotherapy. Int J Radiat Oncol. 2000;48:657-65.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of two systems of patient immobilization for prostate radiotherapy. Radiat Oncol Lond Engl. 2014;9:29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







