Translate this page into:
Chylothorax: The Unusual Suspect
Address for correspondence Anusha C. Madhusoodan, MBBS, MD, Department of Respiratory Medicine, Jawaharlal Nehru Medical College, KAHER University, Belagavi, Karnataka 590010, India. cmanusha@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A chylothorax results when the lymphatic duct becomes disrupted. It is an uncommon and poorly described complication of both Hodgkin’s and non-Hodgkin’s lymphomas of any histological type and grade. A 62-year-old female presented with dyspnea on exertion and dry cough for 15 days. Chest radiograph showed left-sided effusion. Pleural fluid reports were suggestive of chylothorax. Fluid was drained and CT thorax was performed which revealed multiple supra- and infradiaphragmatic lymphadenopathy. Left supraclavicular lymph node biopsy revealed chronic inflammation. Immunohistochemistry of the same sample was reported as non-Hodgkin’s lymphoma of follicular type grade I/III (2008). Positron emission tomography-computed tomography (PET-CT) showed hypermetabolic areas in supra- and infradiaphragmatic lymph nodes and also in multiple bones (with surrounding regions encasement). Patient has received two cycles of chemotherapy with Bendamustine and Rituximab. She is on regular follow-up with the oncologist and doing fine.
Keywords
chylothorax
follicular
lymphatics
non-Hodgkin’s lymphoma
Introduction
A chylothorax is formed when the thoracic duct is disrupted and chyle enters the pleural space. The drainage from the thoracic duct is called chyle. Chyle appears grossly as a milky, opalescent fluid. A chylothorax results when the lymphatic duct becomes disrupted.1 It is an uncommon and poorly described complication of both Hodgkin’s (HL) and non-Hodgkin’s lymphomas (NHL) of any histological type and grade. However, only 12% of pleural effusion cases in NHL may be chylous.2 Chylothorax in patients with lymphoma has a poor prognosis mainly due to severe nutritional deficiencies and wasting.3
Case Presentation
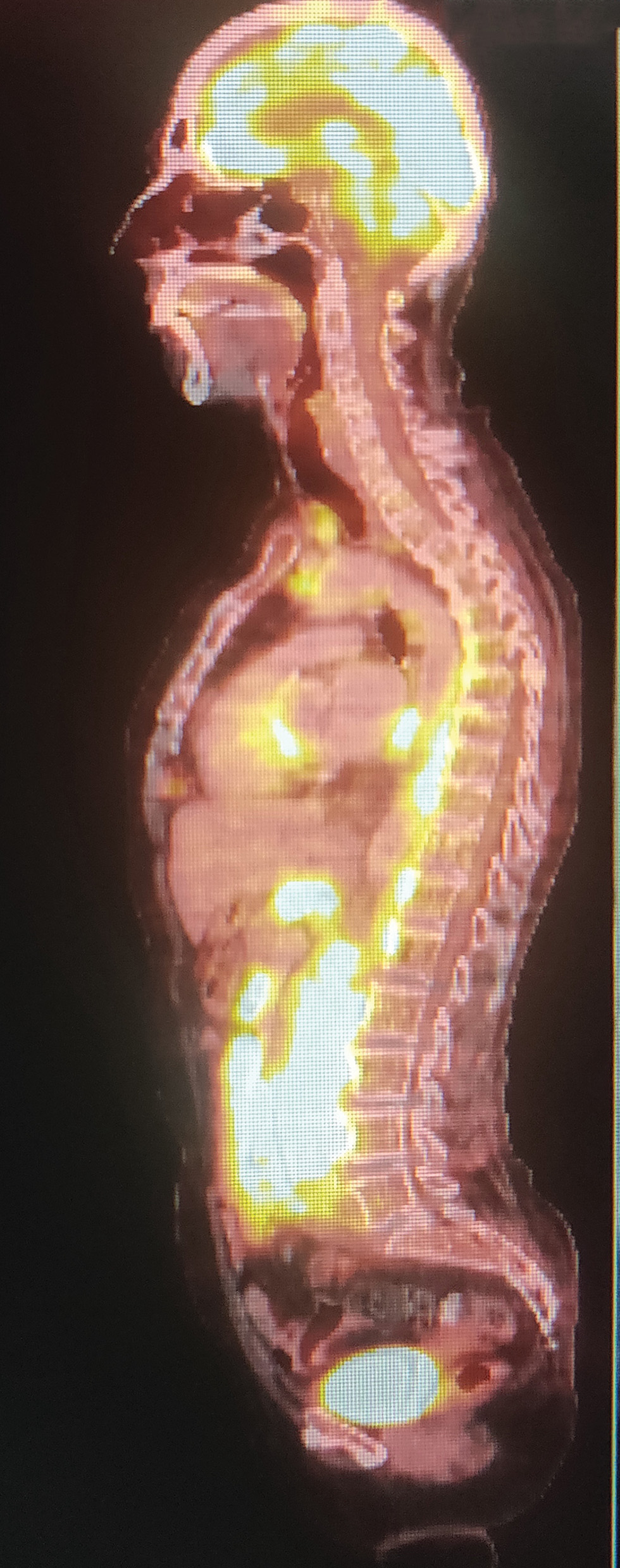
A 64-year-old female presented with dyspnea on exertion and dry cough for 15 days with no history of fever, chest pain, reduced appetite, weight loss, or generalized weakness. On physical examination, vitals were stable. Auscultation revealed reduced breath sounds on the left side. Chest radiograph revealed left-side massive pleural effusion. Milky pleural fluid was aspirated which revealed cholesterol of 77 mg/dL and triglyceride of 195 mg/dL. Left intercostal drainage tube was inserted and approximately 2 L fluid was drained. Computed tomography (CT) thorax revealed multiple supra- and infradiaphragmatic lymphadenopathies with left lower lobe consolidation (Fig. 1). Bronchoscopy was normal, bronchoalveolar lavage for Gene Xpert plus was negative, cytology revealed no malignant cells, and transbronchial lung biopsy was also negative. Left supraclavicular lymph node biopsy revealed reactive hyperplasia. IHC showed NHL of follicular type grade I/III (2008). Tumor cells expressed CD 20, 10, bcl-2 and -6 and immunonegative for cd3 and 23. Positron emission tomography-computed tomography (PET-CT; Fig. 2) showed hypermetabolic areas in supra- and infradiaphragmatic lymph nodes and also in multiple bones (with surrounding regions encasement). Patient received two cycles of chemotherapy with Bendamustine and Rituximab. She is on regular follow-up with the oncologist and doing fine.

-
Fig. 1 CT chest shows multiple mediastinal lymphadenopathy. CT, computed tomography.
-
Fig. 2 PET-CT showing multiple bones involvement. PET-CT, positron emission tomography-computed tomography.
Discussion
Chylothorax is a rare cause of pleural effusion. Malignancy is the leading cause of nontraumatic chylothorax.6 The most common effusion site is pleural, affecting 20 to 30% of NHL and HL, followed by pericardial and peritoneal. Presence of an effusion historically portends a poor prognosis with higher risk for relapse after chemotherapy and decreased overall survival. While effusions in general are common in lymphoma, chylous effusions are exceedingly rare.4
There are two mechanisms described in the literature by which chyle may influx into the pleural cavity. First, increased pressure in the thoracic duct may cause retrograde flow of chyle via the lymphatics of the parietal pleura into the pleural cavity. Another mechanism is thoracic duct rupture due to infiltration of the duct by a lymphoma which causes the susceptibility of the duct to rupture.5,6 Chylothorax often becomes a chronic problem that persists, although the lymphoma has been treated successfully. There are few reports on the management of chylous effusions. In some cases, chylous effusions seem to respond to systemic chemotherapy.7,8
When chylothorax is nontraumatic, treatment of the underlying disease (chemotherapy, irradiation) can lead to improvement, but success rates are limited, ranging for example from 0 to 20 or 33%. Repeated thoracocentesis is usually only performed when improvement is expected from short-term treatment of the underlying disease, or clinical symptoms are present that only require occasional aspiration. Otherwise, in patients with high volume or, especially symptomatic chylothorax, continuous drainage is put in place to allow the lung to reexpand and to optimize pulmonary function. Generally, the success rate of conservative treatment ranges from 16% to more than 75%; at output rates of more than 1,000 mL/day, the success rate of conservative treatment is low. If the lymph leak is due to direct tumor or lymphoma infiltration, it is unlikely that permanent adhesive occlusion will be induced merely by reducing the lymph flow rate. If the drain output reduces markedly under conservative treatment, it is advisable to consolidate the therapeutic outcome with a strict medium chain triglyceride diet for a few weeks.9
Conclusion
This case presents as an example of left-sided chylothorax with multiple lymphadenopathy as the first manifestation of NHL with chyle drainage which showed good response to chemotherapy.
Acknowledgment
We would like to thank Dr. Gajanan S Gaude (Professor and HOD, Department of Respiratory Medicine, JN medical College) for his valuable support in evaluation of this case.
Conflict of Interest
None declared.
References
- 2013. Chylothorax and pseudochylothorax. In: Light’s Pleural diseases. 6th ed. Philadelphia, PA: Wolters Kluwer; 412–426
- Recurrent chylothorax in a patient with non-Hodgkins lymphoma: case report. East Afr Med J. 2004;81(04):215-217.
- [Google Scholar]
- A case of chyloperitoneum secondary to follicular lymphoma and a review of prognostic implications.
- [Chylothorax resulting from malignant non Hodgkin’s lymphoma] Nihon Kokyuki Gakkai Zasshi. 1998;36(05):473-477.
- [Google Scholar]
- [Chylothorax as the initial manifestation of malignant Hodgkin lymphoma] Praxis (Bern 1994). 1998;87(20):690-693.
- [Google Scholar]
- [Treatment options in patients with chylothorax.] Dtsch Arztebl Int. 2013;110(48):819-826.
- [Google Scholar]







