A Case of Malignant Pericardial Effusion, Complicated by COVID-19: Challenges and Successful Management in Rural India
Address for correspondence A.C. Mahantesh, M.D Radiation Oncology, Department of Radiation Oncology, Hassan Institute of Medical Sciences, Sri Chamarajendra Hospital Campus, Krishnaraja Pura, Hassan 573201, Karnataka, India. dracmahantesh@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background Malignant pericardial effusion (MPE) is a rare presentation in cancer, associated with high morbidity and mortality. Pericardial effusion may cause cardiac tamponade and sudden death without timely intervention. Management of MPE in rural setting during coronavirus disease 2019 (COVID-19) pandemic would require a multidisciplinary team in a center with expertise and could be a challenge in rural India with limited resources.
Methods Here we present a case of MPE of unknown origin in a 40-year-old woman, complicated by COVID-19 infection, which was successfully managed in a rural health setting in southern India.
Results She was subjected to prompt pericardiocentesis to relieve symptoms and dose-dense palliative chemotherapy followed by metronomic chemotherapy and pro-anakoinosis therapy during COVID-19 home isolation. She currently has no evidence of disease and is tolerating treatment well.
Conclusion Complex oncological emergencies like MPE of unknown origin can be managed in rural setting in India, with a slight modification of existing facility resulting in successful outcomes. This case of MPE in a 40-year-old lady is a glaring example of how the same can be achieved. Principle of pro-anakoinosis can be of value not only during pandemics and lockdowns but also otherwise, the feasibility of which has to be elucidated in larger studies.
Keywords
malignant pericardial effusion
breast cancer
rural
pro-anakoinosis
metronomic
Introduction
Hassan Institute of Medical Sciences (HIMS) is a District Hospital and Medical College in rural Karnataka, India. Its oncology wing comprises of one consultant medical oncologist, two radiation oncology senior residents on compulsory annual rural service, a telecobalt unit with limited resources, and general pathology department and general medicine department with no dedicated onco-pathology and cardiology facilities. This is the only oncology center in a radius of 150 km with annual oncology outpatient department (OPD) footfall of around 10,000 patients, of both solid malignancies and hemato-oncology cases.
Case Description and Results
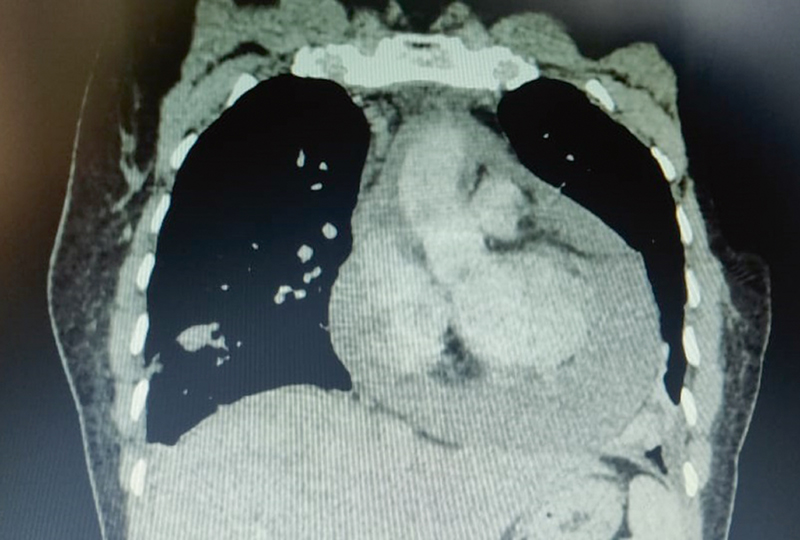
With this background, during second wave of coronavirus disease-2019 (COVID-19) pandemic, a 40-year-old lady came to oncology OPD in March 2021 with exertional dyspnea, tachypnea, and chest tightness, suggestive of cardiac tamponade. On examination, the patient had a moderate degree of respiratory distress, and moist rales were heard in both lungs on auscultation. Her blood pressure was 110/70 mmHg, and her heart rate was regular and ∼120 beats/min. Electrocardiography revealed short PR-Progesterone Receptor intervals, and echocardiography also showed a 3 to 4 mm pericardial effusion on RV-Right Ventricle side and 19 to 20 mm on RA-Right Atrium side. Emergency contrast enhanced computed tomography (CT) scan of whole body (which includes brain, neck, thorax, abdomen, and pelvis) on a 16 slice Philips MX CT scanner (as positron emission tomography-computed tomography is not available in a radius of 150 km) revealed isolated pericardial effusion (Fig. 1).
-
Fig. 1 Computed tomography scan of thorax, suggestive of pericardial effusion.
Patient had a past history of carcinoma of left breast diagnosed in July 2017 in HIMS, Hassan, where she underwent modified radical mastectomy of left breast and axillary lymph node dissection, and was diagnosed with surgical stage IIIC (pT3N3M0) invasive ductal carcinoma of the left breast, triple negative. She received adjuvant anthracycline-based chemotherapy (Adriamycin and cyclophosphamide for four cycles and paclitaxel four cycles from July 2017 to January 2018) and postmastectomy radiation therapy (intensity-modulated radiotherapy 50 gy/25fr from March 2018 to April 2018) at metropolitan city Bangalore, which is 180 km from Hassan town due to unavailability of the same in our institute.
Patient was immediately referred to the in-house general physician who advised oral Furosemide, following which she was referred to an experienced interventional cardiologist serving at nearby private hospital, where she underwent therapeutic and diagnostic pericardiocentesis, which relieved her symptoms. Postprocedure cardiac functions were normal.
Cytology of hemorrhagic pericardial fluid revealed metastatic adenocarcinoma. Meanwhile, aspirated hemorrhagic pericardial fluid was submitted to the general pathology department at HIMS, Hassan, for cytospin, cell block, and histopathology. CEA-Carcino Embryonic Antigen, CA-19.9-Cancer Antigen 19.9 were normal.
Meanwhile, based on her past history of breast carcinoma and pericardial cytology report, our medical oncologist empirically started her on dose-intense chemotherapy (Inj Paclitaxel 80 mg/m2 every week) as per standard protocol. Blood tests and COVID-19 Reverse-transcription polymerase chain reaction (RT-PCR) test were performed before each chemotherapy administration. Patient tolerated chemotherapy well and remained asymptomatic till the fourth cycle, when she contracted severe acute respiratory syndrome coronavirus 2 infection and developed fever, cough, conjunctivitis, Spo2 94%, which was managed as per Indian protocol. After 2 weeks of treatment and home isolation, patient tested negative for COVID-19 RT-PCR. During home isolation, she was advised oral metronomic chemotherapy (Cyclophosphamide 50 mg OD daily) with pro-anakoinosis therapy (Pioglitazone 30 mg BD, Etoricoxib 60 mg OD).
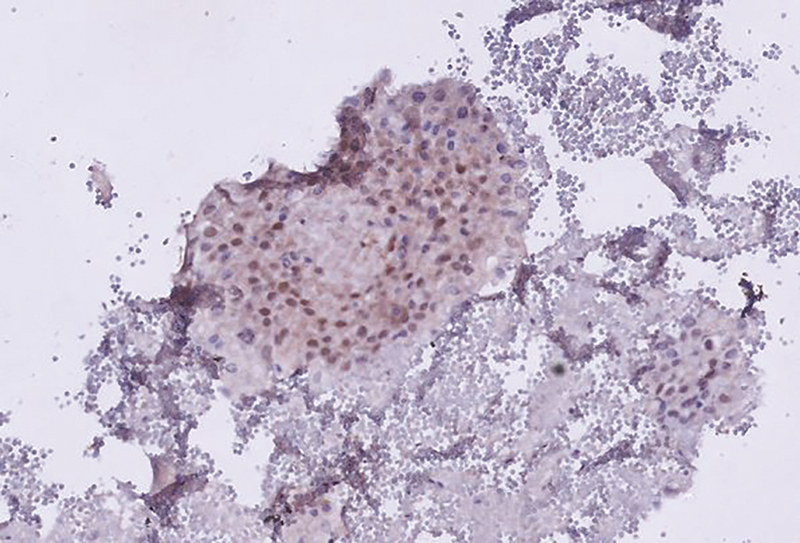
In the meantime, cell block and histopathology reports revealed adenocarcinoma; the blocks and slides were submitted for limited panel immunohistochemistry (IHC) by courier to a dedicated onco-pathology laboratory in metro city, Bangalore (as there was no in-house onco-pathology laboratory at HIMS), at a discounted price, as patient was financially weak. IHC suggested adenocarcinoma of breast cancer origin (tumor cells positive for CK7 and GATA-3; negative for TTF-Thyroid Transcription Factor 1, ER-Estrogen Receptor, PR-Progesterone Receptor, and PAX8 (Fig. 2). HER2-Human Epidermal growth factor Receptor/neu was equivocal and further confirmation with fluorescence in-situ hybridization was not done as patient could neither afford the test nor the treatment in case HER2 came positive, thus justifying chemotherapy of weekly paclitaxel.
-
Fig. 2 Immunohistochemistry of cell block prepared from malignant pericardial effusion, suggestive of breast origin by immunohistochemical marker GATA3.
Discussion
Malignant pericardial effusion (MPE) either at presentation or during the course of a malignancy heralds ominous prognosis. Studies suggest a median survival of 2 to 3 months after an MPE is diagnosed, with a mean survival of 5 months for solid tumors and 20 months for hematologic malignancies.1,2
The most common sites of metastatic breast cancer are the brain, lungs, liver, soft tissues, and bone.3 Although less frequent than solid organ and bone metastasis, MPE is somewhat common in breast cancer. The prevalence of pericardial involvement varies from 4% in general autopsies to 15 to 30% in autopsies of cancer patients.4
This index patient being a farmer, after completing her primary treatment for breast cancer in 2017 at Bangalore, was on follow-up at our department of oncology in HIMS, Hassan, until one day, she presented with exertional dyspnea. At that juncture, the differential diagnosis of anthracycline-/radiation-induced cardiotoxicity versus COVID-19 pneumonia was considered. She tested negative for RT-PCR and CT-thorax did not suggest COVID-19 pneumonia; hence we revised our differential diagnosis to MPE or anthracycline-/radiation-induced cardiotoxicity. On pericardiocentesis, the hemorrhagic nature of the fluid was highly suggestive of MPE and sample was sent for cytospin and histopathology.
All these were accomplished by a swift, coordinated effort between two institutes and three laboratories. As the postpericardiocentesis cytology suggested adenocarcinoma of unknown origin, and in view of her past history of breast cancer and CA-125, CEA-Carcino Embryonic Antigen, and CA-19.9 being normal, the empirical diagnosis of MPE of breast cancer origin was arrived at and the patient was started on dose-dense chemotherapy of weekly paclitaxel. Patient tolerated the treatment well with complete resolution of pericardial effusion. Meanwhile, the course of treatment was interrupted by her testing positive for COVID-19 and she had to be started on oral metronomic chemotherapy (Cyclophosphamide 50 mg OD daily) with pro-anakoinosis5,6 therapy (Pioglitazone 30 mg BD, Etoricoxib 60 mg OD) in addition to anti-COVID-19 medications. (Principle of communicative reprogramming of tumor tissues, i.e., anakoinosis is a novel anticancer therapeutic approach.)
Patient is asymptomatic now with no evidence of disease, and management of this complicated situation at her town has given her a sense of wellbeing while otherwise she would have had to travel to far-off cities like Bangalore, etc., causing immense inconvenience to her and her family.
Here, we have an instance where we have successfully managed a case of MPE as per contemporary standards. Even though the delay in the arrival of pericardial aspirate cell block (took almost 2 months) did not negatively impact the treatment decisions in our index patient fortunately, it has the potential to derail optimal management in such cases. In addition, this approach had positive impact on psychology of patient, with entire treatment being available within the vicinity of her home.
Conclusion
Complex oncological emergencies like MPE of unknown origin can be managed in rural setting in India on par or even better than tertiary cancer centers in metro cities, with a slight modification of existing facility resulting in successful outcomes. This case of MPE in a 40-year-old lady is a glaring example of how the same can be achieved, albeit with an optimal organization of resources and a high index of clinical suspicion. Principle of pro-anakoinosis can be of value not only during pandemics and lockdowns but also otherwise, the feasibility of which has to be elucidated in larger studies.
Acknowledgments
Dr. Thejaswini, Consultant Onco-pathologist, Strand Life Sciences, Bangalore, Karnataka, India.
Pathology Department, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
Conflict of Interest
None declared.
References
- Subxiphoid pericardial drainage for pericardial tamponade. J Thorac Cardiovasc Surg. 1995;109(03):546-551. , discussion 551–552
- [Google Scholar]
- Risk factors affecting the survival of patients with pericardial effusion submitted to subxiphoid pericardiostomy. Chest. 2003;124(01):242-246.
- [Google Scholar]
- Metastatic breast cancer shows different immunohistochemical phenotype according to metastatic site. Tumori. 2010;96(03):424-432.
- [Google Scholar]
- Pericardial disease in patients with cancer. The differentiation of malignant from idiopathic and radiation-induced pericarditis. Am J Med. 1981;71(03):407-413.
- [Google Scholar]
- Anakoinosis: correcting aberrant homeostasis of cancer tissue-going beyond apoptosis induction. Front Oncol. 2019;9:1408.
- [CrossRef] [Google Scholar]
- Anakoinosis: communicative reprogramming of tumor systems - for rescuing from chemorefractory neoplasia. Cancer Microenviron. 2015;8(02):75-92.
- [Google Scholar]







