Translate this page into:
An unusual late complication of peridural anesthesia: The case of a subdural spinal epidermoid cyst: A case report and literature review
Corresponding author: Dr. Abdoulaye DIOP, Department of Neurosurgery, Civil Hospitals of Colmar, PASTEUR Hospital, France, a.diop@univ-zig.sn
-
Received: ,
Accepted: ,
How to cite this article: DIOP A, Limi J, Natacha S, Mortada J, ROBIN S. An unusual late complication of peridural anesthesia: The case of a subdural spinal epidermoid cyst: A case report and literature review. Asian J Oncol. 2024;10:15. doi: 10.25259/ASJO_63_2024
Abstract
The peridural approach is primarily used today to provide analgesia in obstetrics and postoperative care. Peridural analgesia is not only more effective than systemic analgesia, but it also has benefits in terms of morbidity, particularly regarding postoperative respiratory complications and the shortened duration of postoperative ileus. Unlike dural tears, immediate and severe neurological complications such as hematomas or abscesses are very rare. Long-term sequelae are less well known because the relationship with epidural analgesia performed several months or years earlier is not always well established. We report a rare case of a 35-year-old patient with a history of epidural anesthesia five years ago during childbirth, who was admitted with cauda equina syndrome. MRI (magnetic resonance imaging) of the lumbar spine showed a subdural lesion at the level of L3. The patient underwent resection of the lesion, and the pathological examination of the surgical specimen concluded it was an epidermoid cyst.
Keywords
Peridural anesthesia
Subdural spinal
Epidermoid cyst
INTRODUCTION
Epidermoid cysts are rare benign neoplasms that represent less than 1% of all intraspinal tumors. Due to their rarity, only a few cases have been reported in the literature. They can be congenital or acquired. Congenital epidermoid cysts are often associated with spinal dysraphisms such as syringomyelia, dermal sinus, and spina bifida, while the most common etiology of an acquired cyst is repeated lumbar punctures. We report the case of a 35-year-old female patient with a history of epidural anesthesia during childbirth who later developed a lumbar epidermoid cyst revealed by cauda equina syndrome.
CASE REPORT
This is a 35-year-old patient with a history of appendectomy and epidural anesthesia during childbirth five years ago. She presented with low back pain evolving for about a year, associated for the past four months with bilateral cruralgia, more pronounced on the left side. She also reported tingling sensations on the anterointernal aspect of both legs, dysuria, and constipation. Upon examination, cauda equina syndrome was observed, characterized by paraparesis with motor strength rated at 4, diminished deep tendon reflexes, and saddle hypoesthesia. MRI (magnetic resonance imaging) revealed an intradural tumor at the L3-L4 level, compressing the cauda equina roots [Figure 1]. She underwent complete excision of the lesion, which was intraoperatively pearly white and which encased the cauda equina roots [Figure 2]. The postoperative course was marked by full recovery of motor deficit, but some genitourinary disturbances persisted, such as dysuria and urgency. Pathological examination of the surgical specimen concluded that it was an epidermoid cyst lined with keratinizing squamous epithelium without atypia, underlaid by a fibroinflammatory stroma with a few vessels and no signs of malignancy [Figure 3]. Postoperative MRI showed a collection behind the surgical site extending from L2 to L5, measuring approximately 50*20 mm in the axial plane with a height of 10 cm without compressing the cauda equina roots [Figure 4].

- T2 lumbar MRI showing a subdural lesion regarding L3-L4 compressing the cauda equina roots.
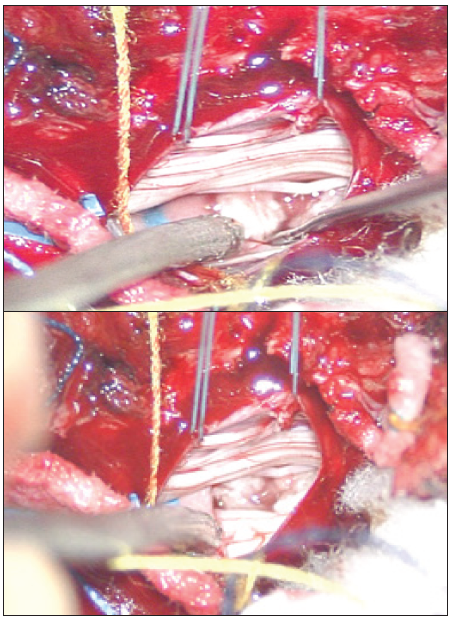
- Peroperatory image of a whitish, pearly lesion enveloping the roots of the ponytail.
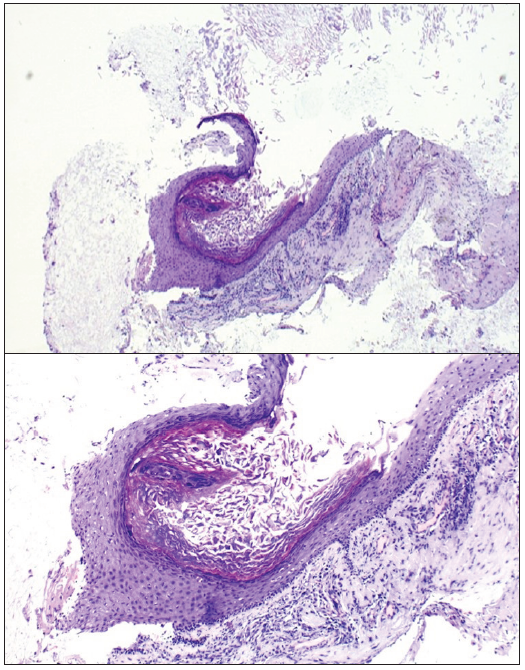
- Pathological image showing an epidermoid cyst, bordered by a keratinizing squamous epithelium without atypia, subtended by a fibroinflammatory stroma containing a few vessels with no sign of malignancy.
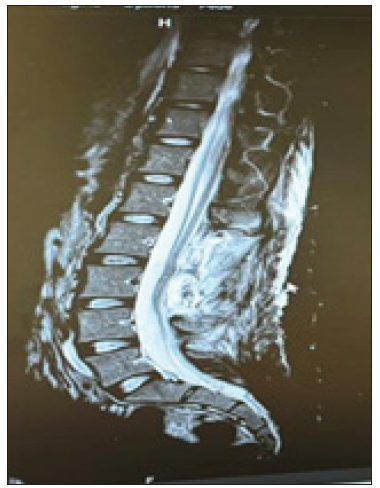
- Postoperative lumbar MRI showing a collection of posterior to the surgical site extending from L2 to L5, approximately 50*20 mm in the axial plane and 10 cm in height, non-compressive on the ponytail roots.
DISCUSSION
The epidermoid cyst is a benign tumor of embryonic origin linked to abnormal localization of ectodermal tissue. The cyst wall is made of squamous epithelium. It is believed that spinal epidermoid cysts have two possible origins: congenital or acquired.[1,2] Congenital epidermoid cysts, more common and often associated with other spinal dysraphisms, are due to abnormal implantation of ectodermal cells during neural tube closure between the third and fifth week of embryonic life. Acquired cysts are attributed to the displacement of epithelial tissue secondary to repeated lumbar punctures, leading to the implantation of ectodermal cells in the spinal canal or trauma.[3] Epidermoid cysts are often intradural and extramedullary in the lumbosacral region.[4] Their symptoms are generally nonspecific, often marked by progressive paraparesis, motor and sensory disturbances, and sphincter disorders due to their slow growth.[5] In our patient, the etiology of this lesion is likely attributable to the epidural anesthesia procedure she underwent during childbirth five years ago. She later developed lower back pain and a progressively worsening deficit, which is the most common sign, according to the literature.[6] The initial diagnosis is based on a spinal MRI. Lesions are usually hypointense on T1-weighted images and hyperintense on T2-weighted images. However, these characteristic signals are not always consistent, and variations have been reported in the literature.[6,7] Typically, there is no contrast enhancement or only a slight rim of enhancement. However, after intravenous gadolinium injection, some peripheral edema may be observed.[7] In our case, MRI showed an intradural lesion at the L3-L4 level, hypointense on T1, and hyperintense on T2, compressing the cauda equina roots. The treatment of choice remains at complete resection after laminectomy or laminoplasty, preserving neurological functions. This resection is indicated for compressive cysts, whether or not associated with clinical signs.[8] In some cases, en bloc resection is not possible. In these situations, cyst drainage and electrocoagulation of the epithelial wall are recommended to delay recurrence. Electrocoagulation of the wall must be carefully performed to avoid creating new neurological deficits or worsening those already present after surgery.[8,9] Although radiotherapy has been used in cases of epidermoid cyst recurrence with relatively good results, this treatment should be reserved for patients who refuse surgery or those who are inoperable for any medical reason.[9] Historically, epidermoid cysts consist of stratified squamous epithelium supported by an external collagen layer. Progressive desquamation of keratin from the epithelium into the cyst produces a soft white substance rich in cholesterol crystals.[10]
CONCLUSION
Epidural anesthesia is associated with the occurrence of serious complications, sometimes leading to permanent neurological sequelae. Spinal epidermoid cysts are among the rarest. Their progression is slow, with pain and neurological deficits as the main clinical signs. Therefore, to ensure the safe practice of epidural anesthesia, adhering to best practice guidelines is essential to avoid serious complications that may arise long after the procedure.
Author Contribution
DIOP Abdoulaye was responsible for the conception and design of article. DIOP Abdoulaye and SAMBOU Natacha were contributed in manuscript writing. JIHED Mortada and SROUR Robin were contributed for final approval of manuscript.
Acknowledgments
We thank everyone who participated in the development of this work.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- A cervico-dorsal intramedullary epidermoid cyst: Case report and review of the literature. J Neurosurg Sci. 1991;35:111-5.
- [PubMed] [Google Scholar]
- Iatrogenic intraspinal epidermoid cyst. Korean J Spine. 2014;11:195-7.
- [CrossRef] [PubMed] [Google Scholar]
- Skin fragments removed by injection needles. Lancet. 1958;2:983-5.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery and outcomes of six patients with intradural epidermoid cysts in the lumbar spine. World J Surg Oncol. 2014;12:50.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Intramedullary spinal epidermoid cyst-a rare cause of spastic paraparesis. Asian J Neurosurg. 2024;19:309-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sporadic spinal lumber epidermoid cyst in an obese adolescent: A radiological and pathological review. Am J Case Rep. 2023;24:e938811.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Iatrogenic intraspinal epidermoid tumor: Myelo-CT and MRI diagnosis. Neuroradiology. 1989;31:273-5.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery and outcomes of six patients with intradural epidermoid cysts in the lumbar spine. World J Surg Oncol. 2014;12:50.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Surgery and outcomes of six patients with intradural epidermoid cysts in the lumbar spine. World J Surg Oncol. 2014;12:50.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sporadic spinal lumber epidermoid cyst in an obese adolescent: A radiological and pathological review. Am J Case Rep. 2023;24:e938811.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







