Translate this page into:
Equitable and affordable cancer program in Assam: An initiative of Tata trusts and Government of Assam
Corresponding author: Subrata Chanda, Preventive Oncology, Assam Cancer Care Foundation, Guwahati, India. drsub05@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Chanda S, Das D, Sen S, Koyyala VPB, Gupta SK. equitable and affordable cancer program in Assam: An initiative of Tata trusts and Government of Assam. Asian J Oncol. 2024;10:6. doi: 10.25259/ASJO_31_2023
Abstract
Objectives
The highest cancer incidence and mortality are observed in the northeastern states of India including Assam. The cancer treatment centers in Assam are located only at the state headquarters. Therefore, patients have to travel a long distance, incurring a good number of out-of-pocket expenses. Considering the severity of the issue, the Tata Trusts, in collaboration with the Government of Assam, established the Assam Cancer Care Foundation and developed the distributed cancer care model with a vision to develop cancer institutions to deliver equitable and affordable care closer to the patient’s homes.
Material and Methods
This is a four-level model. L1 facility is an apex center providing all sophisticated forms of cancer care services including clinical research. L2 facilities developed in Dibrugarh, Silchar, Barpeta, Dhubri, and Diphu provide basic comprehensive oncology services. L3 facilities are being established in Sivasagar, Tinsukia, Nagaon, Nalbari, Golaghat, Goalpara, Tezpur, Darrang, Lakhimpur, Jorhat, and Kokrajhar. These centers will provide diagnostic services to at-risk populations and day-care services for cancer patients. L4 level includes community interventions: preventive health packages delivered at the community level.
Results
Seven hospitals at Barpeta, Dibrugarh, Tezpur, Lakhimpur, Jorhat, Kokrajhar, and Darrang are functional since 28 April 2022. The rest are at different stages of development. Up to August 2023, 2,78,344 people were screened for common cancers where 211 were confirmed for cancers. During the same time, 31,005 patients were registered, and 18,319 chemotherapy sessions and 62,160 radiation therapy sessions were delivered across the 7 hospitals under government schemes resulting in no financial burden to patients.
Conclusion
This intervention by Tata Trusts addresses the barriers of affordability, accessibility, and availability and is replicable to any geography of interest.
Keywords
Assam Cancer Care Foundation
Distributed Cancer Care Model
Community Outreach
Noncommunicable Diseases (NCDs)
INTRODUCTION
Cancer is the second most common cause of death globally with 10 million deaths recorded in 2020. The largest proportion of cancer burden was found in low- and middle-income countries (LMICs) including India, contributing about 70% of cancer-related deaths worldwide.[1] LMICs have limited resources to address the issue of cancer adequately, resulting in late diagnosis and increased mortality.[2] In India, cancer is one of the leading causes (9%) of death.[3] In India, about 14 lakh cases of cancer were detected in 2020.[4] The highest cancer incidence and mortality are observed in the northeastern states of the country including Assam. The incidence of cancer in Assam is 90.2 per 1 lakh population against the national average of 81.2 per 1 lakh population.[5] The delivery of affordable and equitable cancer care is one of Assam’s greatest public health challenges due to multiple factors. It has a difficult terrain with a population of 30.12 million.[6] As per rural health statistics, 2017, Assam has a shortfall of 21% of subcenters (SCs), 1% of primary health centers (PHCs), and 28% of community health centers (CHCs),[7] with no dedicated cancer facility available in rural Assam. Most cancer centers are located at the state headquarters. So, patients have to travel a long distance, incurring a good number of out-of-pocket expenses in traveling and staying in the headquarter city. This also results in these hospitals getting overburdened with patients causing delay in diagnosis and treatment, causing a rise in cancer mortality.[8] Out of pocket expenses in cancer hospitalization are 2.5 times higher than any other ailments’ hospitalization expenditure.[9,10] The financial burden leads patients to acute misery through borrowing, sale of assets, loan from friends and relatives, etc.[11-13] About one-third of cancer patients spend 50% of their annual per capita household income which is increasingly responsible for catastrophic expenditure that negatively affects the patients and several generations of their family.[14,15]
Considering the severity and financial burden, a two-pronged strategy can be implemented—first to develop cost-effective cancer care programs for prevention and early detection of cancer, and second to ensure quality and affordable care for all cancer patients. Hence, to implement these strategies, Tata Trusts, in collaboration with the Government of Assam, developed an equitable and affordable cancer care model called the Distributed Cancer Care Model with a vision to create patient-centric cancer institutions to deliver standardized and affordable care closer to the patient’s homes and aiming for one-third reduction in cancer mortality in 10 years.
MATERIAL AND METHODS
The intervention
In contrast to the current situation where few centralized referral hospitals at the state headquarters handle a cancer patient’s journey end-to-end, it is proposed that smaller centers close to the patient’s home and interlinked with the referral hospitals handle diagnosis and care delivery, thereby shifting the load away from the centralized referral hospitals, providing high-quality cancer care closer to patients’ homes and reducing out-of pocket-expenses for the cancer patients. A memorandum of understanding was signed between the Tata Trusts and the Government of Assam on 3 February 2018, to set up Assam Cancer Care Foundation, for rolling-out the project. Assam Cancer Care Foundation (ACCF) has equal representation from Tata Trusts and Government of Assam on the Board of Directors. The legal nature is a nonprofit company registered under Section 8 of the Companies Act, 2013. ACCF has rolled out a cancer care program in the state of Assam consisting of a network of health infrastructure and avenues for better cancer screening through this network. This model is key for promoting early detection so that the at-risk population (∼40% of all Assam residents) can access confirmatory diagnostics and day-care services closer to their homes.
Distributed Cancer Care Model
The distributed cancer care model consists of four levels as described below.
Level I will be the apex center at the State Cancer Institute Guwahati and will be a 350-bedded cancer care hospital with most advanced radiation, medical, and surgery facilities, along with advanced diagnostics and an institution for teaching, training, and research.
A total of five Level II cancer care hospitals are planned at Barpeta, Dibrugarh, Silchar, Diphu, and Dhubri. These are 150-bedded comprehensive cancer care facilities with surgical, medical, and radiation oncology supported by advanced radiology, laboratory diagnostics, and nuclear medicine. Advanced pathological examination such as histopathology, cytology, immunohistochemistry, etc., are also done in Level II hospitals. Currently, the hospitals at Barpeta and Dibrugarh are functional. The one at Silchar will be functional by April 2024. The hospital at Diphu will be functional by end 2024 And the hospital at Dhubri is expected to be operational by 2025.
A total of eleven Level III facilities are being planned at Tezpur, Lakhimpur, Darrang, Kokrajhar, Jorhat, Sivasagar, Tinsukia, Golaghat, Nagaon, Goalpara, and Nalbari. Level III hospitals are 45-bedded facilities with services for medical and radiation oncology supported by diagnostics facilities including Computed Tomography Scan, Magnetic Resonance Imaging, mammography, ultrasonography, and a variety of others. Of these facilities, five hospitals at Tezpur, Lakhimpur, Darrang, Kokrajhar, and Jorhat are presently functional.
Level IV includes community interventions: preventive health packages delivered at the community level by primary healthcare workers.
All the above ACCF hospitals are empanelled under government schemes such as Pradhan Mantri Jan Aarogya Yojana (PMJAY) and Atal Amrit Abhiyan (AAA). Under these schemes, patients avail cashless treatment of up to Rs 5 lakhs and Rs 2 lakhs, respectively, in empanelled hospitals.
The model is depicted in Figure 1.

- Distributed cancer care model (DCCM).
The geographical distribution of these cancer care hospitals is given in Figure 2
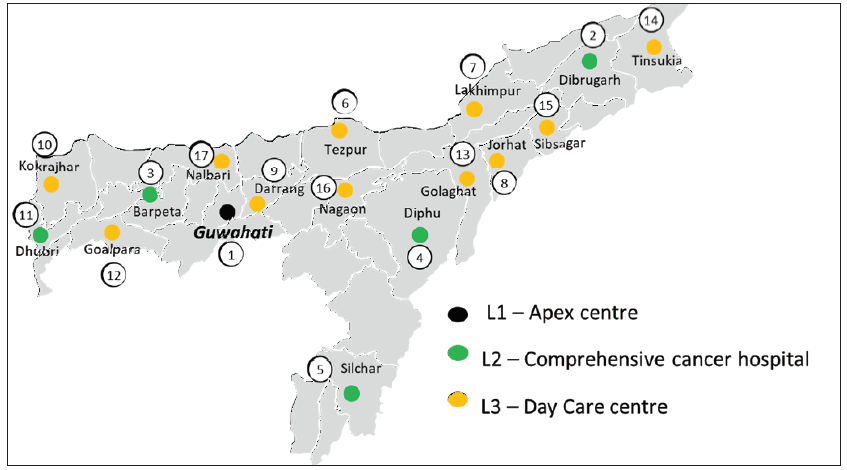
- Geographical location of Assam Cancer Care Foundation cancer hospitals.
Outreach programs
The outreach cancer preventive activities are now ongoing in eight districts of Assam, namely, Barpeta, Cachar, Darrang, Jorhat, Dibrugarh, Kokrajhar, Lakhimpur, and Karbi Anglong. The program is divided into following intervention components:
Programmatic staffs
The ACCF outreach team consists of district health managers (DHM), health camp managers (HCM), dentists, nurses, patient navigators, and data entry operators (DEO). DHM leads all cancer-related activities in the district. HCM organizes and monitors the screening and awareness camps. Oral and breast cancers are screened by dentists and nurses, respectively. They also give demonstration and handholding to the Health and Wellness Centre (HWC) staff. Nurses do cervical cancer screening at PHC and give handholding to the Primary Health Centre (PHC) staff. Patient navigators track all cancer suspected patients so that the patients can complete all necessary investigations and treatment. DEO does all registration of cancer patients during screening and captures vitals of all patients. This is done on an IT application developed in-house so that all data are centrally reposited.
Screening and early detection
There is evidence that oral, breast, and cervical cancers are curable if diagnosed at an early stage. These cancers are preventable with access to high-quality care, periodic screening tests, and regular follow-up. The developed world shows that effective population-based screening programs can easily reduce mortality due to cervical and breast cancers.[16] ACCF program leverages existing government programs—National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS), National Oral Health Program (NOHP), National Tobacco Control Program (NTCP), Ayushman Bharat-Health and Wellness Centers (AB-HWC) to strengthen early cancer detection and prevention of oral, breast, cervical cancers; diabetes; and hypertension.
The screening is divided at the community level and institution level.
Community level
a. Screening
At the community level, the team does handholding support and capacity building of HWC staff such as Community Health Officers (CHOs), Multi-Purpose Workers (MPWs) and Auxiliary Nurse Midwives (ANMs), so that they can confidently screen the above-mentioned clinical conditions. To reinforce the screening process, our dentists and nurses give a demonstration of all screening protocols and methods for two days. Oral cancer and breast cancer screening are done by dentists and nurses, respectively. Oral screening is done through visualization of the oral cavity and breast cancer is screened through clinical breast examination (CBE). All these patients are reported in the government system also under the heading of screening with ACCF. Screening for cervical cancers is done on the third day by nurses in the PHC level through visualization inspection under acetic acid (VIA). Government of India recommends using screening of cervical cancer to be done by VIA in low-resource setting such as subcenters, PHCs of Assam, etc. This is also endorsed by other international bodies. Papanicolaou smear test can be done if adequate resources are available.[17,18]
b. Mobilization
Our camp managers give training to Accredited Social Health Activists (ASHAs) in filling up of community-based assessment checklist (CBAC) forms relevant to NCDs and mobilization activities. They visit house to house along with ASHA workers, at the rate of 10 houses in 2 days of screening camps.
Institution level
ACCF runs the following intervention at the institution level to complement the activities at the community level:
Health kiosks
To enhance the coverage of screening programs, screening kiosks are set up in the Out-Patient Department (OPD) of Medical College Hospitals of Silchar, Diphu, Barpeta, Dibrugarh, and Tezpur Assam. These kiosks are manned by two nurses, and they do opportunistic screening of oral, breast, and cervical cancers along with diabetes and hypertension for all patients and attendants visiting medical college OPDs.
Awareness and preventive activities
Second line of intervention by ACCF generates awareness among the population regarding cancer and its risk factors. ACCF works on the following strategies:
Capacity building of frontline workers
Training and capacity building of frontline health workers to deliver cancer control messages to the community result in positive behavior change. Under the NPCDCS program, the information, education, and communication (IEC) materials developed are adapted by the ACCF screening team for awareness generation and mobilization through the frontline health workers (FLHWs).
Tobacco control activities
ACCF coordinates with the State NCD cell to disseminate awareness material on tobacco and oral cancers to the health and wellness centers of the target districts.
Digital nerve center (DiNC)
All ACCF hospitals are connected to a centralized digital platform, known as DiNC. It plays a pivotal role in facilitating access to healthcare services of our hospitals and completes patient care coordination. The center runs one toll-free no., where patients can call for query, registration, scheduling appointments, follow-ups, etc. As of now, all functional hospitals are connected and all patient management is being handled through this. The details are depicted in Figure 3.
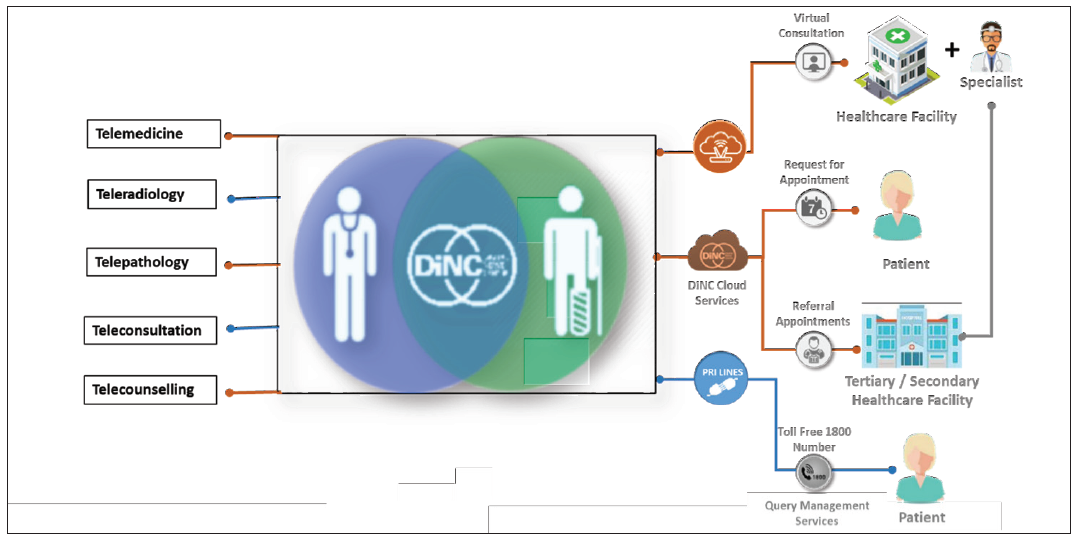
- Digital nerve center (DiNC).
Ethical approvals
Assam Cancer Care Foundation Ethics Committee approved the study with letter no. ACCF/IEC/2023-24/01. We did not interact with the program beneficiaries directly. Anonymous beneficiary data and program were accessed. Therefore, there was no need to obtain informed consent. This model has government approval for implementation.
RESULTS
1. Hospital operations
Seven hospitals were inaugurated by the Hon’ble Prime Minister of India, Mr Narendra Modi on 28 April 2022. Since then, all these hospitals are fully functional and delivering all services, diagnostics, and management of cancer cases. As of August 2023, 31,005 patients were registered, and 18,319 chemotherapy sessions and 62160 radiation therapy sessions were delivered across the seven hospitals. The service details of the hospitals are given in Table 1.
| Center | Total Registrations | Chemotherapy Sessions | Radiation Therapy Sessions |
|---|---|---|---|
| Barpeta | 4,436 | 5,322 | 14,304 |
| Darrang | 3,886 | 1,041 | 3,390 |
| Dibrugarh | 7,954 | 3,184 | 20,577 |
| Jorhat | 4,689 | 3,401 | 10,299 |
| Kokrajhar | 2,424 | 1,106 | 2,230 |
| Lakhimpur | 3,883 | 974 | 4,570 |
| Tezpur | 3,733 | 3,291 | 6,790 |
| Total | 31,005 | 18,319 | 62,160 |
2. Outreach programs
Community outreach programs for cancer prevention activities are functional in Barpeta, Cachar, Dibrugarh, Darrang, Karbi Anglong, Jorhat, Lakhimpur, and Kokrajhar. Twelve tea gardens have been covered so far for screening and preventive activities. Ninety-six model Tobacco Free Educational Institutes have been established as per Cigarettes and Other Tobacco Products ACT, 2003 till August 2023. Five health kiosks for cancer screening are operational in medical colleges of Barpeta, Dibrugarh, Tezpur, Silchar, and Diphu. Till August 2023, Training and handholding support was given regarding the NPCDCS (NCD screening) program to 10,392 Frontline health workers (ASHAs/MPWs/CHOs/ANMs). In the same time period, 2,78,344 beneficiaries were screened for common cancers, where 211 were confirmed for cancer. The screening details in the health kiosk (HK), tea gardens (TG), and community outreach program (COP) are depicted in Table 2.
| Indicators | Oral Cancer | Breast Cancer | Cervical Cancer |
|---|---|---|---|
| People screened (HK) | 89,453 | 31,195 | 20,839 |
| People screened (TG) | 17,416 | 7,566 | 5,984 |
| People screened (COP) | 1,71,475 | 1,28,429 | 2,131 |
| Total screened | 2,78,344 | 1,67,190 | 28,954 |
| People suspected (HK) | 887 | 565 | 209 |
| People suspected (TG) | 217 | 89 | 42 |
| People suspected (COP) | 1,241 | 889 | 128 |
| Total suspected | 2,345 | 1,543 | 379 |
| Confirmed and under follow-up (HK) | 46 | 40 | 25 |
| Confirmed and under follow-up (TG) | 0 | 1 | 0 |
| Confirmed and under follow-up (COP) | 41 | 33 | 25 |
| Total Confirmed | 87 | 74 | 50 |
HK: Health kiosk, TG: These are tea gardens that are owned by Amalgamated Plantations Private Limited (APPL), COP: Community outreach program where beneficiaries are screened in health wellness centers.
3. Hospital revenue
Out of these 31,005 patients, 27,000 patients availed treatment under a government scheme (PMJAY/AAA) generating hospital revenue of Rs 7 million. Average expenditure under the scheme for each patient is Rs 26,000. The patients were not required to pay anything out of their pocket, as they were covered under schemes, thereby making the model viable and affordable for the beneficiaries.
DISCUSSION
The mortality and morbidity due to cancer occurred synchronous to the increasing addictions for tobacco, alcohol, and lifestyle changes amongst especially the young population of India.[19] Of all the chronic illnesses, cancer is considered probably to be the most preventable disease.[20] In 2020, cancer alone contributed to 9.9 million deaths worldwide and by 2040, the number of cancer cases is projected to increase to 28.4 million.[21] Five-year survival for female breast cancer in India is about 66% and in the USA it is 90%.[22] Major factors responsible are the late presentation of the patients with advanced disease, poor access to treatment, and financial constraints.
Low- and middle-income countries have 0.71 teletherapy units/million population, in contrast to 7.62 teletherapy units/million population for high-income countries.[23,24] Presently, only 24.5% of the geographical extent of India is covered by the currently installed radiotherapy units, leaving the rest three-fourths of the nation faced with an inadequacy of cancer treatment facilities. The shortfall in radiotherapy facilities is mostly due to the lack of policy and planning, limited resources, and budget constraints.[25,26]
There has been a metro-centric bias in this relation. The high concentration of good facilities of cancer treatment in metro regions is not reachable to most of the Indian population who are in the suburbs or rural areas, as more than 70% of the Indian population is based in villages. Almost 75% of all healthcare expenses are borne out of pocket by patients and their households, more so in cases of chronic noncommunicable diseases like cancer.[27]
Districts of northeastern seven sister states are lacking decent radiation treatment facilities. These areas comprise hilly and remote terrain with poor connectivity and therefore are difficult to be traversed by the patient for availing treatment. In Assam, till 2020, out of 34 districts, only 3 districts are equipped with radiotherapy units for cancer treatment. Thus, residents of 31 districts barely have a reach to modern cancer care.[28]
There are many models for cancer care in the world, mostly metro-centric and working on a fee for service.[29-30] Our distributed cancer care model is different and unique because it is a joint cancer care project of the Tata Trusts (public sector company) and the Government of Assam with a vision to create patient-centric cancer institutions to deliver standardized and affordable care closer to the patient’s homes. Our ACCF is a non-profitable organization registered under Section 8 of the Companies Act, 2013, and shares common resources with existing hospitals wherever possible keeping patient centricity at the core of planning operations. As per National Sample Survey Office (NSSO) survey 2014, average out-of-pocket expense for a cancer patient is Rs 27,427 and Rs 30,835 for males and females, respectively, in public sector hospitals. ACCF is providing these services for free for the patients, which are being reimbursed to ACCF from government schemes. This results in a sustainable model and is affordable for the patients, saving the likely out-of-pocket expenses.[31]
CONCLUSION
Cancer is emotionally and financially draining the state of Assam. The intervention by Tata Trusts and Government of Assam has addressed the barriers of affordability, accessibility, and availability. The intervention is complemented by outreach community screening which helps in detecting early and improving the survival of the patients. The above program will go a long way in reducing cancer incidence and mortality in the state.
Acknowledgements
The authors are thankful to all those who have shown an active interest in their program and got screened. They also extend their gratitude to all team members for working tirelessly for this program.
Ethical approval
The research/study was approved by the Institutional Review Board at Assam Cancer Care Foundation, number ACCF/IEC/2023-24/01, dated 9th October 2023.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Estimated number of deaths in 2020, all cancers, both sexes, all ages. Cancer today. Published 2020. Accessed January 14, 2022.
- Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209-49.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer Statistics, 2020: Report from national cancer registry programme, ICMR, India. JCO Global Oncology. 2020;6:1063-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- ICMR-NCRP. 2020. [accessed 2023 Oct 29]. https://main.icmr.nic.in/sites/default/files/reports/NCRP_2020_2012_16.pdf
- The burden of cancers and their variations across the states of India: The Global Burden of Disease Study 1990-2016. Lancet Oncol. 2018;19:1289-306.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Census of India 2011: Population, size and decadal change, chapter 1. In: Census. Vol 2013. 2011. p. :561-3.
- [Google Scholar]
- The challenges confronting public hospitals in India, their origins, and possible solutions. Adv Public Health 2014:898502.
- [Google Scholar]
- Delivery of affordable and equitable cancer care in India. Lancet Oncol. 2014;15:e223-e233.
- [CrossRef] [PubMed] [Google Scholar]
- Economic burden of cancer in India: Evidence from cross-sectional nationally representative household survey, 2014. PloS one. 2018;13:e0193320.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Distressed financing of out-of-pocket healthcare payments in India: Incidence and correlates. Health Policy and Planning. 2015;30:728-41.
- [CrossRef] [PubMed] [Google Scholar]
- The economic burden of cancers on Indian households. PLoS ONE. 2013;8:e71853.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLOS ONE. 2013;8:e56873.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Borrowing and selling to pay for health care in low- and middle-income countries. HealthAffairs.. 2009;28:1056-66.
- [CrossRef] [PubMed] [Google Scholar]
- World Health Assembly, 70. (2017). Cancer prevention and control in the context of an integrated approach. World Health Organization. [accessed 2023 Oct 29]. https://apps.who.int/iris/handle/10665/275676.
- Questions about cervical and breast cancer screening knowledge, practice, and outcomes: A review of demographic and health surveys. J Women’s Health. 2017;26:403-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ministry of Health and Family Welfare, Government of India. Operational framework Management of Common Cancers. 2016. [accessed 2023 Oct 29]. https://main.mohfw.gov.in/sites/default/files/ Operational Framework Management of Common Cancers_1.pdf
- American College of Obstetrics and Gynaecologists (ACOG) Cervical cancer screening in low resource setting. Committee opinion, number 624, Feb 2015. [accessed 2023 Oct 29]. https://acog.org/clinical/clinical-guidance/committee-opinion/articles/2015/02/ Cervical cancer screening in low resource setting.
- Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2018;25:2097-116.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 Cancers in 185 countries. CA Cancer J Clin. 2021;0:1-41.
- [Google Scholar]
- Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37513025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Radiation therapy infrastructure and human resources in low- and middle-income countries: Present status and projections for 2020. Int J radiat oncol biol phys. 2014;89:448-57.
- [CrossRef] [PubMed] [Google Scholar]
- Expanding global access to radiotherapy. Lancet Oncol. 2015;16:1153-86.
- [CrossRef] [PubMed] [Google Scholar]
- Is the fast-paced technological advancement in radiation treatment equipment good for Indian Scenario? No. Journal of Cancer Policy. 2015;4:26-30.
- [Google Scholar]
- Radiotherapy services in countries in transition: gross national income per capita as a significant factor. Radiother Oncol. 2002;63:147-50.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15:489-538.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer treatment centres licenced by atomic energy regulatory board. Dec 2017; [accessed 2023 Oct 29]. https://www.aerb.gov.in/images/PDF/Radiotheraphy/rsd3dec2017.
- Models of multidisciplinary cancer care: physician and patient perceptions in a comprehensive cancer center. J Oncol Pract. 2010;6:283-88.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Centers for Medicare & Medicaid Services (CMS). Oncology care model. 2016b; [accessed 2023 Oct 29]. https://innovation.cms.gov/initiatives/Oncology-Care.
- Models of integrated cancer care: A critique of the literature. Aust Health Rev. 2000;23:163-78.
- [CrossRef] [PubMed] [Google Scholar]
- Economic burden of cancer in India: Evidence from cross-sectional nationally representative household survey, 2014. PLoS One. 2018;13:e0193320.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








