Translate this page into:
B-cell non-Hodgkin lymphoma of the larynx: Case report and review of literature
Corresponding author: Dr Mehdi Ferjaoui, Department of Otorhinolaryngology, Fattouma Bourguiba University Hospital, Monastir, University Hospital Fattouma Bourguiba Monastir, Tunisia. fmahdi85@gmail.com
-
Received: ,
Accepted: ,
How to cite box for Continuous Journals: Ferjaoui M, Kolsi N, Bergaoui E, Naouar M, Njima M, Bouatay R, et al. B-cell non-hodgkin lymphoma of the larynx: Case report and review of literature. Asian J Oncol. 2023;9:17. doi: 10.25259/ASJO-2022-33
Abstract
Objectives
The aim of the study is to expose and highlight the clinical, imaging and therapeutic features of B-cell laryngeal lymphoma, with a brief review of literature.
Material and Methods
We report a rare case of B-cell laryngeal lymphoma
Results
A 42-year-old female was referred to the Otorhinolaryngology department for progressive dyspnea and dysphonia. Endoscopic examination and imaging reveals a supraglottis mass. The final diagnosis is a B-cell non-Hodgkin lymphoma of the supraglottis.
Conclusion
Primary laryngeal lymphoma is a rare condition that should be considered in the differential diagnosis of a laryngeal mass, especially if it affects the supraglottic region. The diagnosis is difficult. Direct laryngoscopy with multiples and deep biopsies makes the diagnosis. The treatment and prognosis depend on the stage and grade of the lymphoma.
Keywords
Chronic dysphonia
Dyspnea
Laryngeal lymphoma
Imaging
Chemotherapy
Prognosis
INTRODUCTION
Most head and neck lymphomas arise within the Waldeyer ring. Approximately 25% of cases originate at extra nodal sites. The most common extra nodal sites are the paranasal sinuses, the salivary glands, and the thyroid gland.[1,2] The larynx is an uncommon site for primary non-Hodgkin lymphoma. Less than 1% of laryngeal tumors are hematopoietic neoplasms.[1,2]
MATERIAL AND METHODS
We aimed to present a rare case of B-cell laryngeal lymphoma with a review of the literature, to expose our clinical, imaging, and therapeutic features.
RESULTS
A 42-year-old female was referred to the Otorhinolaryngology department for progressive dyspnea and dysphonia for the last three months. The patient had a past history of B-cell nodal lymphoma treated with chemotherapy and has been in full remission since 2003. She had no smoking history, and no recent intubations were reported. She had no fever, weight loss, or night sweats.
On endoscopic examination, a voluminous mass was seen to extend from the right supraglottis, hiding the glottis area. There were no palpable cervical lymph nodes. The Waldeyer ring was clinically normal.
Cervical-thoracic tomodensitometry demonstrated a right tissular mass involving the supraglottic area measuring 22 × 20 × 26 mm [Figure 1]. A Computed Tomography of the chest, abdomen, and pelvis was negative for additional lymphadenopathy.

- (a) Axial CT scan demonstrates a right tissular mass with regular margins involving the supraglottis with a uniform enhancement. (b) Axial CT scan reveals a discreet infiltration of the hyo-thyro-epiglottic space.
After obtaining patient consent, direct laryngoscopy with multiple biopsies was performed under general anesthesia [Figure 2].
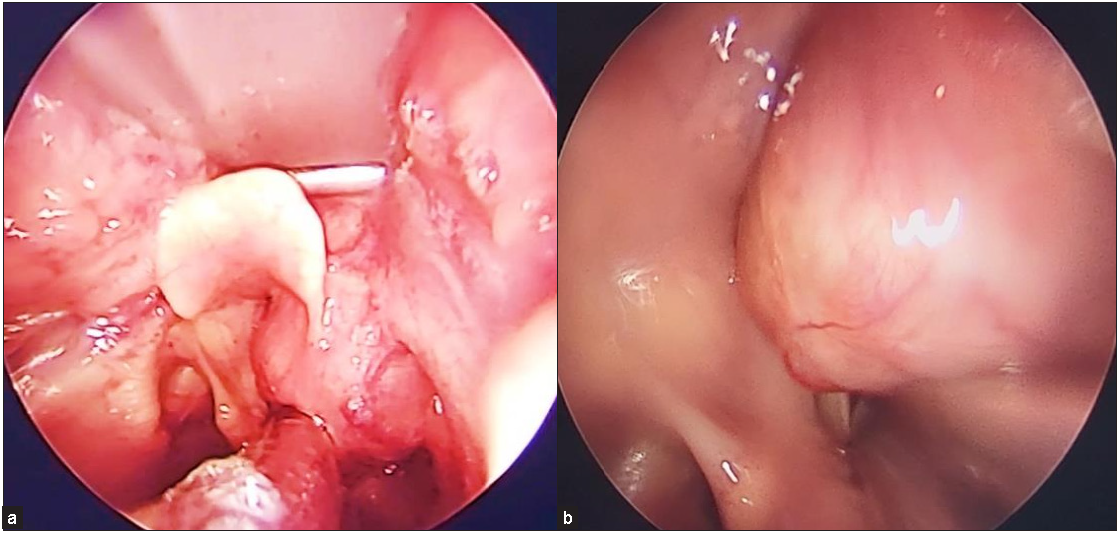
- (a) Direct laryngoscopy shows a supraglottic mass. (b) The mass has smooth submucosal swelling and regular surface. No ulcerations were noted.
Histological examination suggested chronic inflammation of the laryngeal mucosa. After two weeks, we decided to repeat the direct laryngoscopy with deeper biopsies. Neoplastic cells stained positive for clusters of differentiation before (CD) CD20, B-cell lymphoma 6 (Bcl-6), Multiple Myeloma Oncogene 1 (MUM1), and negative for CD10. The proliferative index was 90% with Ki67: a surfactant of mitotic chromosomes. The tumor was consistent with diffuse large cell B-cell lymphoma of the larynx [Figure 3].
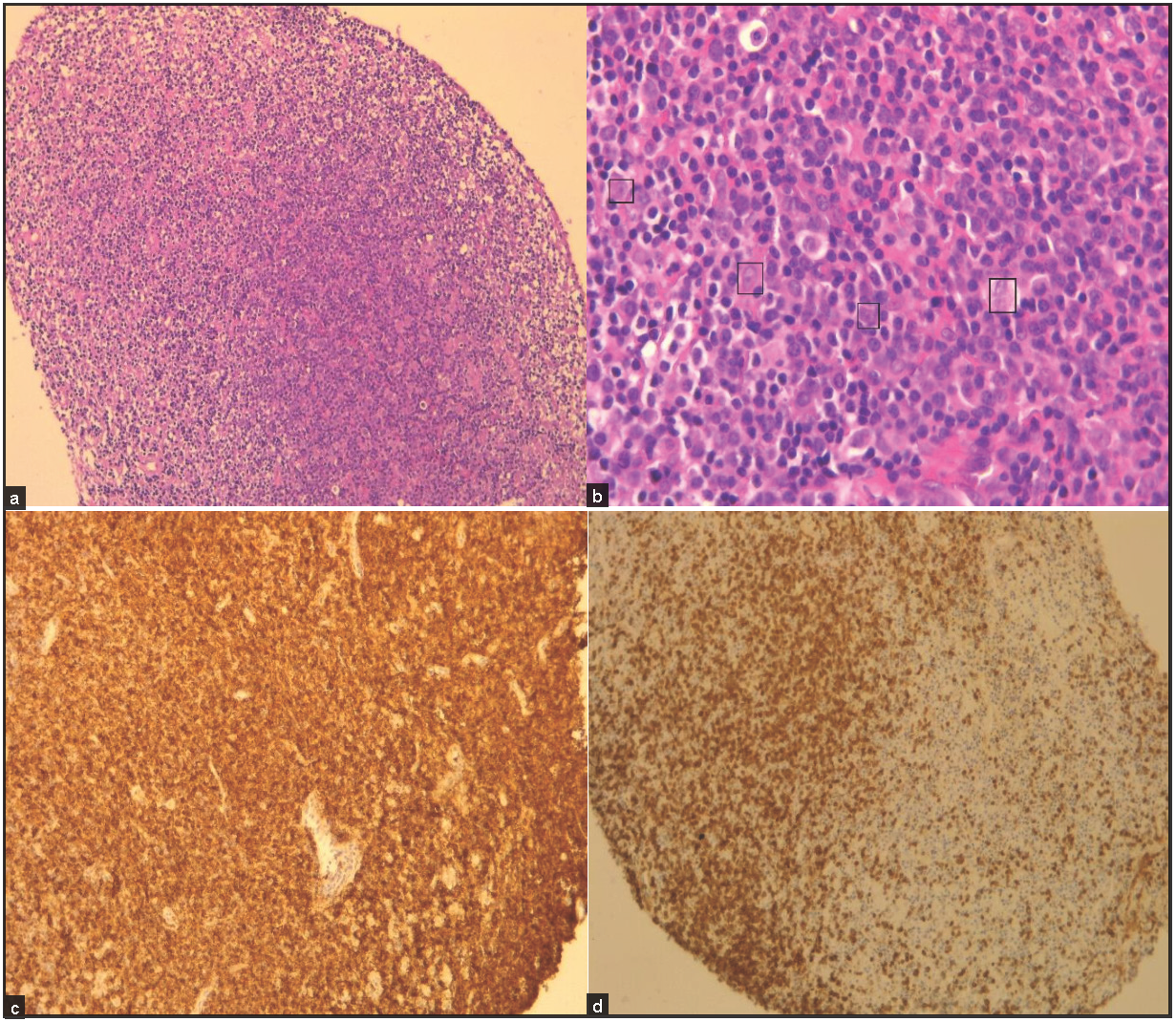
- (a, b) Infiltrate of small mature appearing lymphocytes, abundant histiocytes, and large centroblasts and immunoblasts (black square) dispersed throughout the mucosa (a: microscopic magnification x100, b: microscopic magnification x400). Neoplastic cells stained positive for CD20 (c) and CD3 (d).
The patient was referred to the Department of Hematology for therapeutic management. Chemotherapy according to the rituximab cyclophosphamide hydroxyl doxorubicin vincristine prednisolone (CHOP21) protocol associated to targeted therapy with Rituximab for 21 days was initiated. After six cycles, there was no evidence of residual laryngeal lymphoma on endoscopic examination [Figure 4]. After a 6-month follow-up, there was no recurrence.
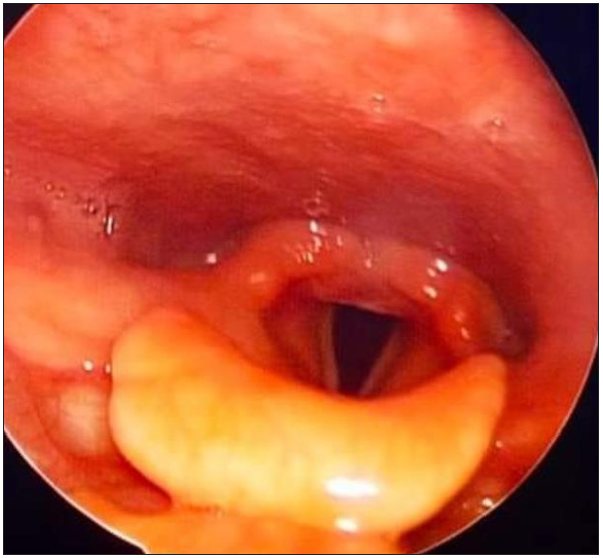
- Post therapeutic indirect laryngoscopy with no evidence of residual laryngeal lymphoma.
DISCUSSION
Although non-Hodgkin’s lymphoma typically presents in lymph nodes, about 25% of cases can develop in extra nodal locations.
Laryngeal lymphoma occurs commonly in the seventh decade of life.[2–4] The sex ratios vary between reports.[2–8] In comparison to squamous cell carcinoma, which is strongly correlated with tobacco, alcohol, and human papillomavirus infection, non-Hodgkin’s laryngeal lymphoma does not have a well-established risk factor.[9] In a meta-analysis of 50 studies and over 2,00,000 participants, smoking was associated with a higher risk of developing non-Hodgkin’s lymphoma of the larynx.[10] Suspected factors in the literature include Epstein-Barr virus infection, chemical exposure (benzenes/herbicides), autoimmune diseases, and genetic predisposition.[9,11]
The diagnosis can be challenging. The symptoms of laryngeal lymphoma are non-specific.[5,12,13] Common warning signs include dysphonia, dysphagia, dyspnea, and stridor. Systemic signs of fever and weight loss were also reported.[3–5,14,15] Dyspnea and dysphonia were present in our patient. The macroscopic appearance of laryngeal lymphoma is not specific either. It is usually described in endoscopy as a smooth submucosal swelling or as a polypoid tumor without ulceration.[15]
As a result, laryngeal lymphoma can easily be misdiagnosed. In a Chinese meta-analysis of about 115 cases of laryngeal lymphomas, 14.8% were misdiagnosed as having chronic laryngitis, and 9.6% underwent unnecessary laryngectomy, which would definitely compromise the patient’s quality of life.
The supraglottic region is considered the most commonly involved area as it contains a relatively high follicular lymphoid tissue compared to other sites of the larynx.[5,16–18]
There are certain imaging characteristics that should suggest lymphoma. The tumor most frequently involves the false cords and aryepiglottic folds but can also involve the epiglottis and true cords. A large non-necrotic lesion localized in the supraglottic area with a submucosal component showing a uniform moderate enhancement with intravenous contrast is more representative of lymphoma than of squamous cell carcinoma.[2,6,7] Like squamous cell carcinoma, lymphoma can extend into the subglottis, oropharynx, strap muscles, with laryngeal cartilage lysis and is not a characteristic feature. Calcifications are not seen with laryngeal lymphoma, usually. Cervical lymphadenopathy commonly seen in supraglottic squamous cell carcinoma, is not habitually present in laryngeal lymphoma.[6,7]
Magnetic resonance imaging characteristics are still diagnostically nonspecific. Laryngeal lymphoma in Magnetic Resonance Imaging (MRI) appears as a homogeneous intermediate T1-weighted and variable T2-weighted signal intensity tumor with homogeneous gadolinium enhancement.[6,7,19] Lymphomas elsewhere show restricted diffusion compared with many other neoplasms.[6,7,19] An MRI was not performed in our case.
Histologically, lymphoma of the larynx is more frequently of the B-cell pattern, T-cell and NK-cell lymphomas are rarely found.[5,19] It is difficult to diagnose it with a biopsy. Generous tissue quantity, deep and multiple biopsies are frequently needed.[20,21] In our patient, we were required to repeat the biopsy to ultimately reach the diagnosis. The unique feature of lymphomas is the fact that they are considered clonal proliferations of lymphocytes, arrested at different stages of differentiation. Immunohistochemistry with various antibodies identifies the specific lineage and the developmental stage. The B-cell lineage demonstrates CD19, CD20, and CD22 immunoglobulins. T-cell lineage demonstrates CD2 and CD3.[22] Furthermore, cytogenetic and molecular studies can be performed to tailor the therapeutic approach.[22]
Therapy for laryngeal lymphoma is not very well-defined. Surgery based on tracheotomy or laser debulking is only used for biopsy and diagnosis, or in cases of important dyspnea. Recent studies have suggested possible treatment of laryngeal lymphoma with radiotherapy only, chemotherapy only, or combined radiation and chemotherapy.[14,15,23] Combined chemo-radiotherapy is the preferred treatment modality, especially for high-grade lymphomas, and provides excellent outcomes.[15,24–27] As for our case, we opted for chemotherapy according to the CHOP21 protocol associated to targeted therapy with Rituximab.
Generally, the prognosis of non-Hodgkin’s laryngeal lymphoma patients is good, with a high survival rate after 5 and 10 years.[14,28]
CONCLUSION
Although primary laryngeal lymphoma is a rare condition, it should be considered in the differential diagnosis of a mass in the larynx, especially if it affects the supraglottic region. The diagnosis is difficult. Direct laryngoscopy with multiples and deep biopsies makes the diagnosis. The most frequent histologic subtype is B-cell non-Hodgkin’s lymphoma. Treatment and prognosis depend on the stage and grade of the lymphoma.
Ethical Approval
Not Applicable.
Declaration of patients consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- T-cell non-Hodgkin’s lymphoma of the larynx and hypopharynx. Otolaryngol Head Neck Surg. 1999;121:335-6.
- [CrossRef] [PubMed] [Google Scholar]
- Laryngeal lymphoma: The high and low grades of rare lymphoma involvement sites. Case Rep Med. 2014;284643
- [Google Scholar]
- Extra nodal lymphoma of the head and neck: A 67-case series. Eur Ann Otorhinolaryngol Head Neck Dis. 2015;132:71-5.
- [CrossRef] [PubMed] [Google Scholar]
- Primary laryngeal lymphoma in China: A retrospective study of the last 25 years. J Laryngol Otol. 2019;133:792-5.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging characteristics of primary laryngeal lymphoma. AJNR Am J Neuroradiol. 2010;31:1261-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-Hodgkin lymphoma of the larynx: CT and MR imaging findings. AJNR Am. J Neuroradiol. 2004;25:12-5.
- [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology and prognostic indicators in laryngeal lymphoma: A population-based analysis. Laryngoscope. 2018;128:2044-9.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and etiology of non-Hodgkin lymphoma: A review. Acta Oncol. 2006;45:258-71.
- [CrossRef] [PubMed] [Google Scholar]
- Cigarette smoking and risk of lymphoma in adults: A comprehensive meta-analysis on Hodgkin and non-Hodgkin disease. Eur J Cancer Prev. 2013;22:131-50.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck lymphomas—A retrospective ten-year observation. Contemp Oncol. 2017;21:66-9.
- [Google Scholar]
- Primary marginal zone B-cell lymphoma of the larynx. J Craniofac Surg. 2012;23:1-2.
- [CrossRef] [PubMed] [Google Scholar]
- Primary laryngeal natural killer/ T-cell lymphoma--Report of a rare case. Head Neck. 2008;30:1527-30.
- [CrossRef] [PubMed] [Google Scholar]
- Individual participant data meta-analysis of primary laryngeal lymphoma: Focusing on the clinical characteristics and prognosis. Laryngoscope. 2015;125:2741-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary laryngeal lymphoma: Report of 3 cases and review of the literature. Head Neck. 2010;32:541-9.
- [CrossRef] [PubMed] [Google Scholar]
- Subglottic tracheal stenosis as primary manifestation of a marginal zone B-cell lymphoma of the larynx. In Vivo. 2005;19:547-50.
- [PubMed] [Google Scholar]
- Extranodal lymphomas of the head and neck. Ann Diagn Pathol. 2005;9:340-50.
- [CrossRef] [PubMed] [Google Scholar]
- Primary Burkitt lymphoma of the supraglottic larynx: A case report and review of the literature. J Med Case Rep. 2017;11:65.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- MR imaging of primary malignant lymphoma in the larynx. Eur Radiol. 2001;11:1079-82.
- [CrossRef] [PubMed] [Google Scholar]
- Primary laryngeal T/NK-cell lymphoma, nasal-type: An unusual location for an aggressive subtype of extranodal lymphoma. Eur Arch Otorhinolaryngol. 2008;265:705-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary laryngeal lymphoma: Report of 3 cases and review of the literature. Head Neck. 2010;32:541-9.
- [CrossRef] [PubMed] [Google Scholar]
- Primary lymphoma of the larynx: New diagnostic and therapeutic approaches. ORL J Otorhinolaryngol Relat Spec. 2003;65:321-6.
- [CrossRef] [PubMed] [Google Scholar]
- All that wheezes is not asthma: A case of diffuse large B-cell lymphoma of the larynx. Case Rep Oncol Med. 2017;2017:7072615.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary malignant non-Hodgkin lymphoma of the larynx: Report of a case. The Pan African Medical Journal. 2011;17
- [Google Scholar]
- Primary non-Hodgkin lymphoma of the larynx. Southern Med J. 2005;98:388-9.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated primary non-Hodgkin’s malignant lymphoma of the larynx. J Laryngol Otol. 2001;115:324-6.
- [CrossRef] [PubMed] [Google Scholar]
- Primary lymphoma of the larynx: A case report and literature review. Open Jr Clin Diag. 2015;5:81-5.
- [Google Scholar]
- Plasmablastic lymphoma of the larynx: Report of two cases. J Laryngol Otol. 2013;127:96-9.
- [CrossRef] [PubMed] [Google Scholar]







