Translate this page into:
Botryoid rhabdomyosarcoma of common bile duct: Diagnostic imaging features of an unusual pathology: Case report and review
Address for correspondence: Dr. Ashish Verma, Department of Radiodiagnosis and Imaging, Institute of Medical Sciences, Banaras Hindu University, Varanasi - 221 005, Uttar Pradesh, India. drdnv5@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Rhabdomyosarcoma (RMS) is the most common tumor of biliary tree in childhood. Biliary tree is an uncommon site for RMS to occur, accounting for about 1% of all pediatric RMS. A preoperative diagnosis is not difficult with background knowledge of its imaging features. The diagnosis of this malignancy is especially important as it many times mimics a more common and benign condition of choledochal cyst. The key to diagnosis is to distinguish solid component of the tumor from organized sludge seen in choledochal cyst. Imaging plays a vital role for preoperative staging as well.
Keywords
Biliary tree
botryoid rhabdomyosarcoma
magnetic resonance cholangiopancreatography
Introduction
Sarcoma botryoides (botryoid in Greek means “bunch of grapes”) is an embryonal variant of rhabdomyosarcoma (RMS) which arises in proximity to the mucosal surface of a hollow viscus or body cavity. Botryoid RMS (B-RMS) of the biliary tree is a rare tumor, and the first case was described by Wilks and Moxon in 1875 and only accounts for 0.04% of childhood cancers.1,2 The lesion accounts for 1% of all RMSs.1,3 Though this tumor is commonly seen in children and infants, the common sites are head and neck, genitourinary tract, and retroperitoneum.4,5,6 Tumors of the extrahepatic biliary tract are rare in childhood, but RMS is most common among these unusual tumors.7,8 It has been noted that unlike RMS at other sites, where alveolar or undifferentiated histology may be present, the biliary tract contains tumors of only embryonal or botryoid histology.9
It is a rare tumor; however, it is the most common cause of obstructive jaundice due to neoplastic biliary obstruction in children,4 following nonneoplastic conditions such as choledochal cyst, congenital anomalies of the biliary tree, biliary atresia, and gallstones.1,2 The management and prognosis of this tumor are constantly changing as new imaging techniques and chemotherapy as initial treatment become available.4 Timely diagnosis is important since the prognosis depends on the stage of the disease at diagnosis. The present report highlights certain imaging features that may help in early diagnosis of B-RMS and differentiation from other mimicking conditions.
Case Report
A 4-year-old boy presenting with fever, progressive jaundice, pruritus, loss of appetite, and fatigue over a month's duration was referred for sonography of abdomen. The child was alert but in distress and had jaundice and pallor. Sonography revealed mild hepatomegaly without splenomegaly or ascites. Laboratory investigations showed a deranged liver function test with leukocytosis while the urine was positive for bile salts and pigments. Further, on sonography, the biliary tree was dilated with peribiliary focal lesions in liver raising a suspicion of cholangitis abscesses. Heterogeneous solid appearing tissue was filling up the lumen of dilated common bile duct (CBD). This tissue had multiple cystic areas within which color Doppler flow noted in the solid component. On close inspection, the mass appeared attached to the wall of middle CBD at a focal point only with no suggestion of invasion of the deeper layers or pericholedochal tissue Figure 1. A suspicion of biliary RMS with cholangitis was raised, and a magnetic resonance imaging (MRI) with magnetic resonance cholangiopancreatography (MRCP) was done to confirm the same, as the initial clinical diagnosis was one of choledochal cyst with biliary sludge and cholangitis. The intracholedochal heterogeneous lesion was seen with solid hypointense and cystic hyperintense areas on T2 weighted (T2W) images. This was associated with a heterogeneous hepatic parenchyma (due to cholangitis) and intrahepatic biliary dilatation. There were no round/target lesions in liver parenchyma showing morphology suggestive of metastasis; also no regional adenopathy was noted. A contrast study using intravenous gadobenate dimeglumine (MultiHance) was done. Renal function parameters were within normal limit (serum creatinine - 0.8 mg/dL and blood urea - 21 mg/dL). Postcontrast imaging revealed a heterogeneous lesion with cystic and enhancing solid areas. The solid area shows the internal area of “ring enhancement” located in the CBD Figure 2. The lesion was seen completely filling CBD, hila, right and left hepatic ducts. Secondary and tertiary ducts were not dilated, and no obvious intraluminal content was seen. No enhancing round/target lesions suggesting a metastatic deposit were noted in the liver. Cholecystectomy with open exploration of CBD was performed which revealed “grape-like” gelatinous material and solid tissue within the lumen, which was attached to the wall of mid-CBD by a pedicle. Primary purpose of open exploration was to resolve biliary obstruction by evacuating the lesion as much as possible and placing T-tube in situ before closure. Postoperative, combined chemotherapy including vincristine, dactinomycin, and cyclophosphamide regimen was started as per evidence-based protocol for biliary RMS. The microscopic examination showed spindle-to-oval cells in a myxomatous background. The nuclei were fusiform-to-oval and hyperchromatic with coarse chromatin in variably eosinophilic cytoplasm. There was typical condensation of cells beneath the surface epithelium forming a characteristic “cambial layer” Figure 3. These features were suggestive of B-variant RMS.
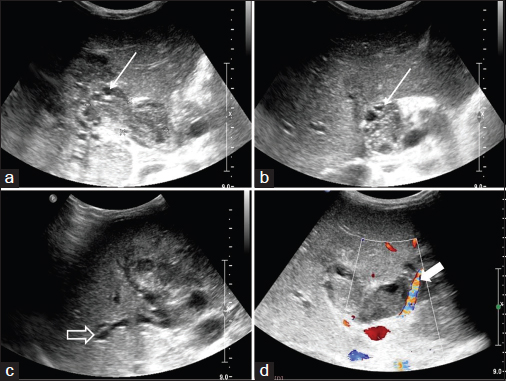
- (a-c) Ultrasonography of the patient shows a solid echogenic lesion with multiple cystic areas within (straight arrow) filling up the lumen of common bile duct. Note the intrahepatic biliary dilatation (hollow arrow) resultant to biliary obstruction caused by the tumor. The color Doppler examination (d) reveals a prominent vessel running along and supplying the tumor (solid arrow). This was separate from the common hepatic artery (not shown here)
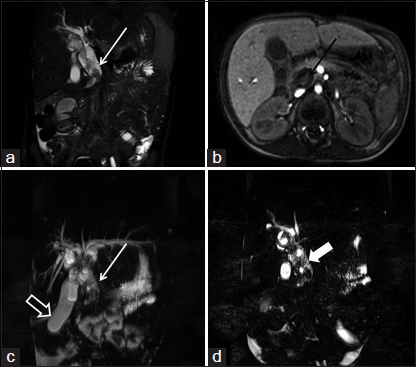
- (a) T2-weighted image fat suppressed coronal image showing the “bubbly appearance” (isointense tumor interspersed with hyperintense cystic areas) typical for botryoid-rhabdomyosarcoma (white arrow). (b) The contrast enhanced axial scan shows heterogeneous lesion with cystic and enhancing solid areas. The solid area shows the internal area of “ring enhancement” located in the tumor (black arrow). (c and d) The magnetic resonance cholangiopancreatography images show intrahepatic biliary dilatation with a distended gall bladder (hollow arrow). Note the “bubbly appearance” is better seen on the thin section magnetic resonance cholangiopancreatography images (solid arrow in d)
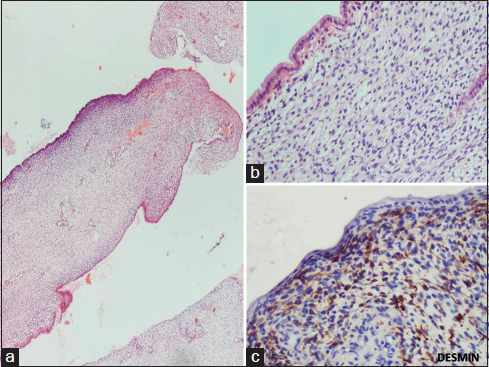
- (a) Tumor showed polypoid nodules, with an abundant, loose, myxoid stroma embedded in which are present small undifferentiated cells and showing distinctive hypercellular zone (cambium layer) just below the columnar mucosal epithelium (H and E, ×40). (b) High power view showed round to oval-, spindle-, and stellate-shaped primitive mesenchymal cells embedded in a loose myxoid matrix present (H and E, ×400). (c) Several tumor cells show immunoreactivity for desmin (Desmin, ×400)
Discussion
B-RMS of biliary tree is a disease of young children with slight male preponderance, (median age 3 years; range 1–9 years).7,8,10 The tumor may arise in any part of the biliary tree9,11,12 or in a choledochal cyst.13 The main imaging differential of B-RMS is a choledochal cyst with organized sludge,14 sonography being the primary diagnostic tool for initial diagnosis. In the present case, the modality revealed biliary system filled with solid cystic content giving “network/lace-like” appearance, described as being characteristic in the literature.15,16 On color Doppler application, the presence of intralesional vascularity, as in the present case, confirms the possibility. The current evidence labels MRI with MRCP as the next step in an ambiguous case, as being noninvasive.16,17,18 T2W intensity of lesions has been correlated with the density of cellular architecture and decreases as the compactness increases.19 B-RMS may be of varying cellular compactness,4,14,20 hence the T2W intensity pattern, which may be useful toward the diagnosis of lesion cellularity and grade.21 Contrast study adds to the level of confidence toward the diagnosis, but no added information is usually provided by the same.22 MultiHance is a safer drug in the background risk of nephrogenic systemic fibrosis, and the same was used in this case. Positron emission tomography-computed tomography would have been a much better modality for distant metastasis work up but could not be done due to nonavailability in our institute.
The “bubbly ” appearance and “multiple ring enhancements” seen on postcontrast images and T2W MRI features (hypointense solid areas interspersed with bright cystic areas), in this case, and described well in the literature as the “botryoid sign,” is sufficiently diagnostic for B-RMS.13 MRCP, on the other hand, may map the intrabiliary extension of lesion and the anatomy of pancreaticobiliary junction, which may be important for planning of the surgery.21,22 Surgery in the first stage allows exploration and biopsies. Gross total excision is not possible in most cases due to disease spread at the time of diagnosis. Generally, chemotherapy forms the second stage. These turnouts are chemosensitive and rapid tumor shrinkage is observed.16 The extent of surgical resection currently recommended depends on the primary tumor site.
Diagnostic imaging in biliary tree B-RMS is directed at its characterization, assessment of extent of the tumor within the liver (and especially along the intrahepatic bile ducts), regional spread, and distant metastases. Ultrasound with color Doppler is the primary diagnostic tool and may be the best technique to assess response to preoperative or postoperative chemotherapy. Contrast MRI with MRCP provides multi-planar images which further helps in characterization and detailed mapping of tumor. Gross surgical excision is not possible in advanced stages, higher rates of recurrence in postoperative cases and chemosensitive nature of tumor-considering these facts, preoperative diagnosis by above-mentioned imaging modalities can give strong suspicion of B-RMS which helps in early detection and early initiation of chemotherapy. This helps in reduction of operative and postoperative complications. “Rare malignancy” which often mimics a benign etiology (choledochal cyst). The intent of the article is to emphasize the diagnostic features of RMS of biliary tract so that an early diagnosis can be achieved which will have an impact on prognosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Hepatobiliary rhabdomyosarcoma in children: diagnostic radiology. PediatrRadiol. 1998;28:101-8.
- [Google Scholar]
- Botryoid Rhabdomyosarcoma of Biliary Tree: A Diagnostic puzzle. IOSR Journal of Dental and Medical Sciences. 2015;14:94-6.
- [Google Scholar]
- Botryoid rhabdomyosarcoma of the biliary tract in children: a unique case report. Eur J Cancer Care. 2006;15:463-6.
- [Google Scholar]
- Botyroid Rhabdomyosarcoma of the Common Bile Duct. Bombay Hospital Journal. 2010;52:108-10.
- [Google Scholar]
- Embryonal rhabdomyosarcoma of the biliary tree mimicking a choledochal cyst. Journal of Cancer Research and Therapeutics. 2007;3:40-2.
- [Google Scholar]
- Gall Bladder and Extra hepatic biliary tree In: Stephen S, ed. Sternberg Diagnostic Surgical Pathology (Third edition.). Philadelphia: Lippincott Williams and Wilkins; 1999. p. :1666. In Chap. 38
- [Google Scholar]
- Case report: Sarcoma botryoides of the common bile duct. Indian J Radiol Imaging. 2001;11:101-2.
- [Google Scholar]
- Biliary rhabdomyoscarcoma mimicking choledochal cyst. J Gastrointestin Liver Dis. 2008;18:95-7.
- [Google Scholar]
- Rhabdomyosarcoma of the biliary tree in childhood. A report from the Intergroup Rhabdomyosarcoma StudyCancer. 1985;56:575-81.
- [Google Scholar]
- Two different manifestations of botryoid sarcoma (embryonal rhabdomyosarcoma) of the biliary tree. Bildgebung. 1994;61:40-3.
- [Google Scholar]
- Intergroup rhabdomyosarcoma study-IV: Results for patients with nonmetastatic disease. Journal of Clinical Oncology. 2001;19:3091-3102. et al.
- [Google Scholar]
- Embryonal rhabdomyosarcoma of the biliary tree in children: a case report. Pediatr Radiol. 1987;17:250-1.
- [Google Scholar]
- Embryonal rhabdomyosarcoma of the common bile duct mimicking choledochal cyst. J Hepatobiliary Pancreat Surg. 2005;12:263-5.
- [Google Scholar]
- Obstructive jaundice may be due to a malignant tumor of the common bile duct. Pediatr Surg Int. 1995;10:496-7. et al.
- [Google Scholar]
- The Turkish Journal of Pediatrics. 2012;54:654-7.
- Embryonal rhabdomyosarcoma within a choledochal cyst. Can AssocRadiol J. 1992;43:145-8.
- [Google Scholar]
- Embryonal rhabdomyosarcoma (sarcoma botryoides) of the biliary tree. Cancer. 1969;24:333-342.
- [Google Scholar]
- Sarcoma botryoides arising from the biliary tract of children a case report with review of the literature. Acta Pathol Jpn. 1976;26:709-718.
- [Google Scholar]
- The ”botryoid sign”: a characteristic feature of rhabdomyosarcomas in the head and neck. Neuroradiology. 2001;43:331-5. et al.
- [Google Scholar]







