Translate this page into:
Evaluation of fatigue in head and neck cancer patients undergoing (intensity modulated radiation therapy) radiotherapy: A prospective study
Address for correspondence: Dr. Mranalini Verma, Department of Radiotherapy, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow - 226 014, Uttar Pradesh, India. shilpisinghal2003@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction: Fatigue is a common symptom in cancer patients and persists after the completion of cancer-directed treatment. We attempted to study temporal variation in fatigue levels in head and neck cancer (HNC) patients when they were treated by radiotherapy (RT) using intensity modulated radiation therapy techniques.
Materials and Methods: Histologically proven HNC patients (AJCC stage II and III with Karnofsky performance status [KPS] ≥80) receiving RT between August 2009 and October 2011 were included. Fatigue was assessed before, during and at 3, 6, and 12 months following RT and compared with age-matched healthy controls by using EORTC QOLQ C30 (using question number 10, 12, and 18).
Results: Twenty-six patients were evaluated, whose baseline average fatigue score was 22.4, which was significantly higher as compared to controls (average fatigue score = 12.8; P = 0.04). During RT, average fatigue score increased to 30 by 3 weeks (P = 0.02) and rising to 33.2 (P = 0.029) towards the end of RT. Three months following RT, average fatigue score decreased to 22.8 and remained between 23 and 20 at 6 and 12 months respectively. Significant higher fatigue scores were observed in patients with advanced stage (P = 0.000). Lower KPS score did not show significantly higher fatigue scores (P = 0.5).
Conclusion: Our study shows that HNC patients suffer greater fatigue than age-matched healthy individuals which is further aggravated by RT. It gradually comes back to the pretreatment level by 3 months following treatment, but does not reach to a normal healthy level even at 12 months following treatment.
Keywords
Cancer
fatigue
head and neck
quality of life
radiotherapy
Introduction
Fatigue is a multifaceted, subjective condition. It can be defined as a multi-dimensional phenomenon, which evolves over time, compromising physical energy, mental capacity and the psychological condition of any patient. Fatigue can be described using a range of general characteristics (severity, negative sensations, and temporal features) and specific weaknesses (lack of energy, weakness, somnolence, difficulty in concentrating.[1]
Fatigue is the most common symptom in a cancer patient.[2] Almost 70–100% patients of cancer are affected by fatigue.[3] Cancer-related fatigue is the most common distressing symptom, and it persists for months or even years after the completion of cancer-specific treatment. The high degree of fatigue even affects the quality of life (QOL).[4,5,6]
Fatigue associated with cancer has both physical and psychological causes; the former include anemia,[7] various metabolic disturbances and inadequate nutrition due to anorexia, nausea, vomiting or gastro-intestinal obstruction.[8] The psychological factors which may contribute to fatigue include depression, anxiety. These factors may lead to chronic sleep deprivation. In addition, the releases of endogenous inflammatory cytokines have been reported to contribute to the severity of fatigue in some patients.[9]
Qualitative reports indicate that cancer-related fatigue differs from normal fatigue, which is related to lack of rest or overexertion, as it involves more severe and enduring mental, physical, and emotional domains. Although substantial research on cancer-related fatigue has been conducted, but a few longitudinal studies have been conducted that assess patients before and after radiotherapy (RT) completion. RT is also known to cause or add to fatigue in cancer patients. In fact, the incidence of fatigue in cancer patients on RT has been reported between 65% and 100%.[10,11,12,13,14] Fatigue could be quantitatively measured in directly from QOL scales or directly by fatigue-specific instruments. The fatigue scale of EORTC QLQ-C30 consists of three items that assess how much (using a four point Likert scale) the individual required rest, felt weak, and felt tired during the past week.[15,16] We tried to study prospectively the degree of fatigue that sets in head and neck cancer (HNC) patients, while they are on RT. Fatigue related to cancer or its treatment should not be ignored, rather it should be addressed if possible, for greater patient satisfaction.
Materials and Methods
A prospective study was carried out from August 2009 to October 2011 at Department of Radiotherapy SGPGIMS, Lucknow. The study was approved by the Institutional Ethics Committee. All patients were biopsy proven HNC receiving RT and informed consent were taken from all patients.
Previously untreated, histology proven with normal hematological and biochemical parameters, AJCC stage II and III HNC patients with Karnofsky performance status (KPS) of 80 or more were included. All patients were counseled for oral hygiene and alimentation. Patients who received chemotherapy were excluded from the study. Since all of them were treated by an accelerated RT protocol, RT alone was given by 6-MV photons from a linear accelerator using intensity modulated radiation therapy (IMRT) technique and the dose was 66 Gy in 30 fractions at 2.2 Gy/fraction, five fractions per week delivered over 6 weeks. During RT, patients were seen by the radiation oncologist at least once a week. Treatment toxicity (according to the Radiation Therapy Oncology Group criteria) and weight loss were recorded at weekly intervals. Diet counseling and enteral feeding by Ryle's tube as per need (weight loss more than 5%) were also given. All these patients are free of disease at 1-year.
The Hindi versions of the EORTC QLQ-C30 and QLQ-H and N35 questionnaires were obtained from the QOL Unit of the EORTC Data Center. Fatigue was assessed using question number 10, 12, and 18 from the EORTC QOL C30 questionnaire (Hindi version). The following questions were asked: (1) Did you need rest? (2) Have you felt weak? (3) Were you tired?
HNC patients were further asked to fill EORTC QOL C30 questionnaire once before start of treatment, during radiation (3rd and 6th week of radiation) and after 3, 6, 12 months of radiation. Age-matched healthy individuals were also asked to fill the same questionnaire for comparison. Fatigue was scored using EORTC QOL C30 scoring manual version 3.0 that is, Raw scores (RS); RS = (I1 + I2 + I3 + ...................... + In)/n and symptom scales (SS): The values ranged from 1 to 4; SS = [(RS-1)/range] × 100.
All the scores were measured in the 0–100 scale. A high score for the SS represents a low QOL that is, higher fatigue.
Statistical analysis
Mean fatigue score of all patients and age-matched healthy volunteers were calculated. A unpaired t-test was applied to quantify the statistical significance of the difference between a cancer patient and healthy subjects, and paired t-test was applied to quantify the statistical difference in cancer patients before, during and after RT. The trend of the fatigue score over time was evaluated through different time point.
Results
A total of 26 HNC patients were evaluated for fatigue associated with RT. The median age of the cancer patients was 60 years (38–80 years) and median age groups of healthy patients were 59 years (40–70 years). Demographic features of this cohort are given in Table 1.
|
Characteristic |
Median (range) (n=26) |
|---|---|
|
Age (years) |
60 (38-80) |
|
Gender |
|
|
Male:female |
25:1 |
|
KPS |
|
|
80 |
15 (60) |
|
90 |
11 (40) |
|
Smoking |
|
|
Yes |
21 (90) |
|
No |
5 (10) |
|
Co-morbid illness* |
|
|
No illness |
21 (80) |
|
Diabetes |
3 (11) |
|
Hypertension |
5 (19) |
|
Primary site |
|
|
Oropharynx |
8 (45) |
|
Larynx |
12 (35) |
|
Hypopharynx |
6 (20) |
|
T-stage |
|
|
T2 |
9 (35) |
|
T3 |
17 (65) |
|
N-stage |
|
|
N0 |
18 (50) |
|
N1 |
5 (30) |
|
N2 |
3 (20) |
|
Overall stage |
|
|
Stage II |
9 (35) |
|
Stage III |
17 (65) |
|
Percentage weight loss during RT |
|
|
<5% |
15 (58) |
|
5-10% |
6 (23) |
|
>10% |
5 (19) |
|
Hemoglobin (%) |
|
|
Pretreatment levels (g/dL) |
13.5 (10.8-15.7) |
|
Posttreatment levels (g/dL) |
11.1 (10.1-14.6) |
|
RTOG toxicities-mucositis |
|
|
Grade II |
19 (73) |
|
Grade III |
07 (27) |
*Three patients have both diabetes and hypertension. IMRT - Intensity modulated radiation therapy; KPS - Karnofsky performance status; RT - Radiotherapy; RTOG - Radiation Therapy Oncology Group
All the patients received RT using IMRT-Simultaneous Integrated Boost technique. A dose of 66 Gy in 30 fractions over 6 weeks was delivered to the high-risk volume and 54 Gy in 30 fractions to elective nodal regions (low-risk volume).
Cancer-related fatigue was evaluated at baseline, during and following RT in cancer patients. Baseline average fatigue score of cancer patients was 22.4. Ten ages matched healthy volunteers were chosen for 1 time assessment of the fatigue score for comparison. The scores of cancer patients were significantly higher as compared to healthy volunteer subjects (average fatigue score 22.4 vs. 12.8 respectively) (P = 0.04) [Tables 2 and 3].
|
n |
Median age (range) |
|
|---|---|---|
|
Age group of healthy control |
26 |
59 years (40-70 years) |
|
Healthy persons |
Cancer patients |
|
|---|---|---|
|
AFS |
12.8 |
22.4 |
HNC - Head and neck cancer; AFS - Average fatigue score
During RT average fatigue score of cancer patient significantly increased to 30, midway during treatment (P = 0.024) and further increased to a maximum of 33.2 (P = 0.029) by the end of RT. Average fatigue score further decreased to 22.8 3 months following treatment and then became static at 6 (score = 23) and 12 months (score = 20) post-RT [Figure 1].
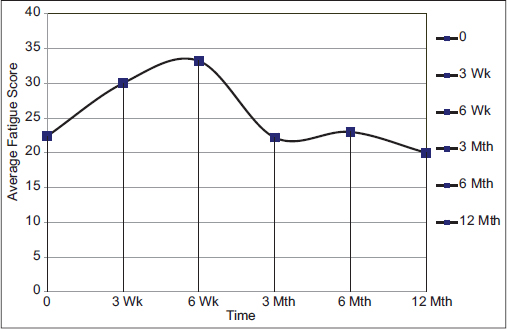
- Temporal changes in fatigue score of head and neck cancer patients at baseline, during radiotherapy and follow-up at 3, 6, and 12 months of completion of radiotherapy treatment
Correlation of fatigue with other variables: Significantly higher fatigue scores were observed in patients with more advanced AJCC stage (P < 0.001). Fatigue scores were insignificantly higher in patients with lower KPS (P = 0.574).
The other factors which were found not to be of significance towards contribution of fatigue were age (<60, ≥60), site (oropharynx, larynx, hypopharynx), percent weight loss during RT (<5%, ≥5%), pretreatment hemoglobin levels (<13, ≥13) and degree of mucositis (grade 2, grade 3).
Discussion
In this study, fatigue was higher in cancer patients as compared to healthy subjects. RT consistently added to fatigue in these patients, while they were on treatment. During follow up a dramatic improvement followed by a slow improvement in feeling of fatigue was observed by these patients, over 1-year. Even when the patients were free of disease, but their fatigue levels did not reach to those of healthy individuals – at 1-year after completion of radiation treatment. This could be due to the debilitating sequel that mend lifestyle modification, experienced by HNC patients who have received radical RT.
Fatigue is thought to be a nonspecific, multidimensional concept that involves subjective feeling of tiredness, weakness, and/or lack of energy. The distinct dimension of fatigue, e.g., sensory, emotional and cognitive, have to be measured.[3] Fatigue in oncology is unique. Unlike acute fatigue level, in which tiredness comes on quickly, last a short time, and is relieved by rest, cancer fatigue is prolonged, debilitating, that is persistent or recurring.[17] Cancer-related fatigue is present in the majority of the patients before the start of treatment. Several clinical factors have been identified as causative elements in fatigue: Pain, emotional distress, sleep disturbance, anemia, nutrition, activity level, hypothyroidism and other co-morbidities. It has been reported that 43% of patients presented with significant fatigue in cancer patients. Cancer-related fatigue is not relieved by rest.
Jereczek-Fossa et al. showed a different pattern of fatigue scores, that is, there was a significant increase in fatigue in the first 2 weeks and then a decrease. They attributed it to patient anxiety during the initial phase of treatment and his ability to adapt to treatment thereafter.[18] Their observation clearly differed from ours since the fatigue scores continued to rise as the treatment progressed in our study. Poor nutritional reserves coupled with an inability to take adequately due to radiation-related acute oral mucositis in HNC patients could be responsible for this observation.
The presence of anemia, directly or indirectly, causes fatigue as has been reported by several authors. Corrections of anemia improve the patient fatigue status.[19] The present study did not show any correlation between pretreatment hemoglobin levels and fatigue, possibly due to small sample size of the study. Age and decreased thyroid function have also been correlated with increasing fatigue during treatment.[20] We did not find any correlation with age in the present study, and thyroid function assessment was not carried out before or after treatment in these patients.
Treatment of cancer, especially RT, is prolonged and may be spread over 1–2 months. Daily visits to the hospital are bound to add to tiredness and fatigue in these patients. Literature is limited on the impact of radiation on cancer-related fatigue. Numerous physical and psychological factors are thought to contribute to fatigue in patients treated with radiation therapy. The list of possible causes includes anemia, cytokine activation and anxiety and depression. It has been studies that cytokine release contributes to the development of fatigue by exerting effects on the endocrine system and neurotransmitters. High concentrations of tumor necrosis factor, interleukin 1, and interleukin 6 have been described in various cancers that can contribute to fever, weight loss, sweats, and anemia, as well as fatigue. The correlation between fatigue and treatment-related factors is not yet clear, and conflicting data have been published. It has been seen that the incidence of fatigue is proportionate to the radiation field size. Patients undergoing magna-field RT for bone marrow transplantation or palliation extensive bone metastases experience significant fatigue.[3,21] The above symptoms are also observed among patients undergoing total axial nodal irradiation for lymphoma. The incidence of fatigue is comparatively less among patients undergoing limited field RT as in carcinoma of the glottis larynx.[3,21]
Site of irradiation also affects the intensity of fatigue. Irradiation of the head and neck showed higher fatigue scores than chest wall irradiation in breast cancer patients. Higher fatigue score in HNC patients during RT is due to mucositis, odynophagia, decreased oral intake and thickened saliva. Dose per fraction and stage of the disease also impacted the incidence and severity of fatigue.[16] The present study clearly reflected a similar rising trend during RT, in case of HNC patients. Comparison of fraction size was not possible in this study as all patients were treated by the same protocol.
Unlike the findings of the present study, Irvine et al. showed that there were no differences in the mean level of fatigue experienced by cancer patients and the mean level experienced by healthy controls before the start of cancer treatment. However, cancer patients experienced a significant increase in fatigue over a 5- or 6-week course of RT and 14 days after treatment with chemotherapy, and these increases were significantly greater than the fatigue reported by healthy control subjects.[14]
In an Indian study Janaki et al. also showed that fatigue gradually increases over the course of radiation (treated by conventional RT) and peaked in last week. It reached to pretreatment level few weeks following treatment.[22] Similar to our study, a study by Zmijewska-Tomczak et al. showed that radiation significantly influenced QOL life in patients with head and neck squamous cell carcinoma by the end of treatment, as compared to baseline parameters. They reported higher baseline fatigue scores as compared to our study, that is, 32, and a clear rise to a score of 47 was observed by them by the end of radiation, clinical important value (⋄ =15) confirming that this is at least one of the symptoms that gradually worsened QOL.[23] In our study, fatigue scores increased at the end of radiation from score 20 to a modest 33 in comparison (⋄ = 13). Nutting et al. in the PARSPORT trial assessed the level of acute fatigue using EORTC QLQ 30 and HN 35 tools. They compared the level of fatigue in IMRT with the conventional arm. It was observed that acute fatigue (>grade 2) was seen in more number of patients in IMRT arm as compared to conventional RT arm (74% vs. 41% respectively).[24]
The explanation offered for this observation was that extra volume of the normal brain got irradiated with IMRT technique because of the use of multiple beams from different directions.
The strengths of the present study are that it is a prospective work, where a comparison with similar age healthy individuals has been studied. The impact of RT alone (i.e., without chemotherapy) has been studied unlike the PARSPORT trial where patients received both neoadjuvant and concomitant chemoradiotherapy This study was limited by its small numbers of patients and other caveats are that we did not correlate fatigue with other known causes like thyroid functions, psychological factors, and other comorbidities.
Conclusion
Our study shows that fatigue was higher in cancer patients as compared to healthy subjects. Radiation treatment added to fatigue in HNC patients. Patients felt maximum fatigue at the end of treatment. By 3 months, the levels returned back to the pretreatment levels of a cancer patient and continued to remain almost the same for 6 months. Significant higher fatigue scores were observed in patients with more advanced cancer (stage 3 disease). Poor general condition, age, site, percent weight loss, pretreatment hemoglobin levels and grade of mucositis, did not correlate with the fatigue level in these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Fatigue and the cancer experience: The state of the knowledge. Oncol Nurs Forum. 1994;21:23-36.
- [Google Scholar]
- The impact of fatigue on patients with cancer: Overview of FATIGUE 1 and 2. Oncologist. 2000;5(02):9-12.
- [Google Scholar]
- Patient, caregiver, and oncologist perceptions of cancer-related fatigue: Results of a tripart assessment survey. The Fatigue CoalitionSemin Hematol. 1997;34(02):4-12. 3
- [Google Scholar]
- The Functional Assessment of Cancer Therapy-Anemia (FACT-An) Scale: A new tool for the assessment of outcomes in cancer anemia and fatigue. Semin Hematol. 1997;34(02):13-9. 3
- [Google Scholar]
- The development of an instrument to measure the subjective dimension of fatigue In: Key Aspects of Comfort: Management of Pain, Fatigue, and Nausea. New York: Springer; 1989. p. :199-208.
- [Google Scholar]
- Treatment-related fatigue and serum interleukin-1 levels in patients during external beam irradiation for prostate cancer. J Pain Symptom Manage. 1993;8:196-200.
- [Google Scholar]
- Fatigue and radiotherapy: (A) experience in patients undergoing treatment. Br J Cancer. 1998;78:899-906.
- [Google Scholar]
- Pathophysiological Phenomena in Nursing: Human Response to Illness London, UK: Saunders; 1993. p. :279-302. editors.
- [Google Scholar]
- The prevalence and correlates of fatigue in patients receiving treatment with chemotherapy and radiotherapy. A comparison with the fatigue experienced by healthy individualsCancer Nurs. 1994;17:367-78.
- [Google Scholar]
- Psychometric validation of the EORTC Core Quality of Life Questionnaire, 30-item version and a diagnosis-specific module for head and neck cancer patients. Acta Oncol. 1992;31:311-21.
- [Google Scholar]
- Fatigue states after cancer treatment occur both in association with, and independent of, mood disorder: A longitudinal study. BMC Cancer. 2006;6:240.
- [Google Scholar]
- Factors influencing quality of life in cancer patients: Anemia and fatigue. Semin Oncol. 1998;25(03)(07):43-6.
- [Google Scholar]
- Assessment and management of cancer-related fatigue in adults. Lancet. 2003;362:640-50.
- [Google Scholar]
- Fatigue during head-and-neck radiotherapy: Prospective study on 117 consecutive patients. Int J Radiat Oncol Biol Phys. 2007;68:403-15.
- [Google Scholar]
- Prevalence of fatigue among cancer patients undergoing external radiotherapy. Southeast Asian J Trop Med Public Health. 2004;35:463-7.
- [Google Scholar]
- Magnitude of fatigue in cancer patients receiving radiotherapy and its short term effect on quality of life. J Cancer Res Ther. 2010;6:22-6.
- [Google Scholar]
- Factors influencing quality of life in patients during radiotherapy for head and neck cancer. Arch Med Sci. 2014;10:1153-9.
- [Google Scholar]
- Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): A phase 3 multicentre randomised controlled trial. Lancet Oncol. 2011;12:127-36. et al.
- [Google Scholar]







