Translate this page into:
Central Bronchogenic Carcinoma Presenting with Ipsilateral Vocal Cord Palsy, Metastases to the Brain, and Contralateral Lung
Address for correspondence Reddy Ravikanth, MBBS, MD,, Department of Radiology, Holy Family Hospital, Thodupuzha, Iddukki district 685605, Kerala, India. ravikanthreddy06@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
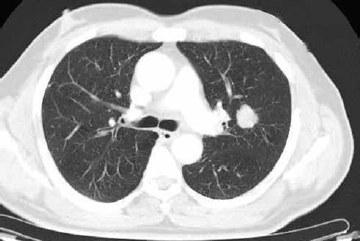
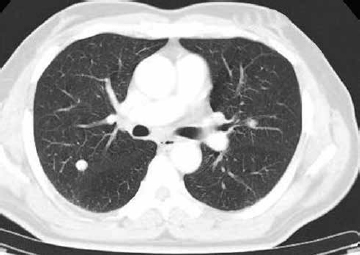
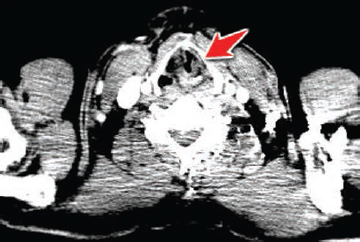
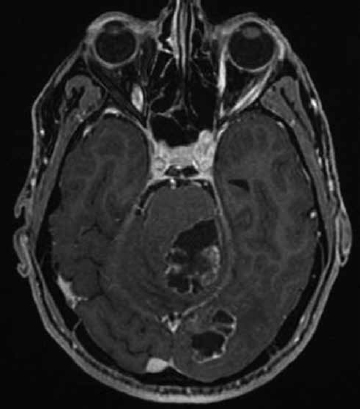
A 62-year-old man presented to the emergency department with one episode of hemoptysis (30 mL volume) and a 3-week history of hoarseness of voice. The patient described a progressive decline in his voice, resulting in the inability to speak. The patient’s other medical history was significant for hypertension and congestive heart failure. The patient had a 30-pack-year history of tobacco use. On physical examination, the patient’s supine blood pressure (BP) was 114/74 mm Hg, with a pulse rate of 74 beats/min. He also described headaches, giddiness attacks, inability to move his eyes, and loss of visual acuity. Direct laryngoscopy revealed left vocal cord paralysis. The cord was fixed in the paramedian position with left bowing of the cord and decreased laryngeal elevation. Contrast-enhanced computed tomography (CECT) of the thorax revealed left parahilar irregular and spiculated, mildly enhancing soft tissue mass lesion in the superior lingular segment of the left upper lobe and was seen extending to the aortopulmonary window (Fig. 1). It measures 2.1 × 2 × 2.5 cm in its anteroposterior, mediolateral, and craniocaudal diameters. The lesion is associated with desmoplastic reaction of the left upper lobe. Metastatic lesions were noted in the contralateral lung as well in the posterior segment of the right upper lobe (Fig. 2). On CT, medialization of the left vocal cord with ipsilateral enlargement of the laryngeal ventricle and pyriform sinus were noted, suggesting left vocal cord palsy (Fig. 3). Precontrast and contrast-enhanced magnetic resonance imaging (MRI) of the brain demonstrated multiple thick, ring-enhancing lesions in the left occipital lobe and left cerebellar hemisphere and middle cerebellar peduncle with prominent surrounding edema and mass effect on the pons (Fig. 4). Hemoptysis is coughing out of frank blood/blood clot or sputum tinged with blood. Blood streaking is due to ulceration of the bronchial mucosa by the tumor and usually is rather minimal in degree. However, some patients report significant hemoptysis of 25 to 200 mL, related to rupture of bronchial veins or venules.1 Hoarseness in association with lung cancer is almost always caused by involvement of the left recurrent laryngeal nerve. The recurrent laryngeal nerves innervate the vocal cords. In the thorax, the left recurrent laryngeal nerve is more vulnerable than the right because it pursues a longer intrathoracic course, coming into contact with the mediastinal surface of the left lung, continuing along the mediastinal lymph nodes, and finally looping around the aortic arch. In patients with lung carcinoma, the left recurrent laryngeal nerve is most frequently involved as it courses through the aortopulmonary window.2 Vocal cord paralysis may be caused by a variety of mediastinal disease entities including various neoplastic conditions such as bronchogenic carcinoma and may be the presenting symptom of an otherwise clinically occult disease. Brain metastases are not only the most common intracranial neoplasm in adults but also very prevalent in patients with lung cancer. Brain metastases are the most common intracranial neoplasm, occurring in 8 to 10% of cancer patients and are a significant cause of cancer-related morbidity and mortality worldwide.3 The most common origins of brain metastasis include primary cancers of the lung, breast, skin (melanoma), and the gastrointestinal (GI) tract. Among these, primary tumors in the lung are the most common cause of brain metastases, as up to 65% of patients with lung cancer will ultimately develop brain metastases.4 Among the various histologies, small cell lung cancer (SCLC) is most likely to metastasize to the brain, followed by non–small cell lung cancer.5 SCLC is known for its high risk of early hematogenous dissemination, especially to the brain. Contralateral lung metastasis may represent hematogenous metastases or synchronous primary tumors. Size of the primary tumor and N-stage may help distinguish hematogenous metastasis from those with a synchronous tumor and second primary.6 The CT images analyzed can more accurately detect the extent and location of the responsible pathology than a chest radiograph. Careful evaluation of findings at CT examination, which should include the upper mediastinum, can then be helpful in directing and guiding appropriate intervention, whether surgery or watchful waiting.
-
Fig. 1 CECT of the chest showing parahilar irregular, spiculated, enhancing soft tissue mass lesion in the superior lingular segment of the left upper lobe. CECT, contrast-enhanced computed tomography.
-
Fig. 2 CECT of the chest showing a metastatic lesion in the posterior segment of the right upper lobe in the contralateral lung. CECT, contrast-enhanced computed tomography.
-
Fig. 3 CECT at the level of vocal cords demonstrating medialization of the left vocal cord with ipsilateral enlargement of the laryngeal ventricle and pyriform sinus suggesting left vocal cord (arrow) palsy. CECT, contrast-enhanced computed tomography.
-
Fig. 4 CEMR of the brain demonstrating thick, ring-enhancing lesions in the left occipital lobe and left cerebellar hemisphere encroaching into the middle cerebellar peduncle with prominent surrounding edema and mass effect on the pons. CEMR, contrast-
enhanced magnetic resonance image.
Conflict of Interest
None declared.
FundingNone.
References
- Hemoptysis: a retrospective analysis of 108 cases. Respir Med. 2002;96(09):677-680.
- [Google Scholar]
- Vocal fold paralysis as a sign of chest diseases: a 15-year retrospective study. World J Surg. 2006;30(03):293-298.
- [Google Scholar]
- Management of brain metastases: the indispensable role of surgery. J Neurooncol. 2009;92(03):275-282.
- [Google Scholar]
- Prognosti.factors of synchronous brain metastases from lung cancer. Lung Cancer. 2001;33:143-154. 2-3
- [Google Scholar]
- Brain metastases in small cell lung cancer. Oncology (Williston Park). 2004;18(08):961-972, discussion 974, 979–980, 987.
- [Google Scholar]
- Additional pulmonary nodules in the patient with lung cancer: controversies and challenges. Clin Chest Med. 2011;32(04):811-825.
- [Google Scholar]






